Sports Medicine 2013
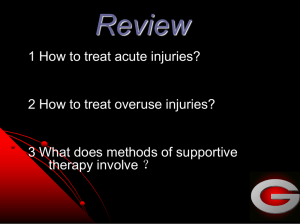
advertisement

Sports Medicine 2013 Jacqui McCord-Uys Sports Physiotherapist Who am I ? • • • • • • • • Practising since 1989 Sports injuries since 1990 Beijing Olympics team Common Wealth teams (Snr & Jnr) All Africa Games SA Schools Rugby, Women's Rugby Falcons Rugby Team (4 yrs) SuperSport United Football Club Medical Team Leader & Physio (16yrs) • Course presenter in India 2011 & 2012 • Conference Presentations 2008,2010,2011, • ETC……. Sports Medicine • • • • Why the need for specialization? GP orthopaedic surgeon not sufficient? Work opportunities? Qualifications needed? – MSc Sports Medicine Degree(TUKS, Wits, UCT & Bloemfontein) – College of medicine & HPCSA approved Specialist rating awaiting Government approval. Sport Injuries • Acute Bone Articular Cartilage Joint Ligament Muscle Tendon Bursa Nerve Skin Sports Injuries • Chronic ie overuse Bone stress Osteitis & Periostitis Articular cartilage Joint Ligament Muscle Tendon Nerve Bursa Skin AND the unknown…… Sports Injury principals • • • • • Diagnosis Treatment Recovery Rehabilitation Return to Play Diagnosis There is no more difficult art to acquire than the art of observation. (William Osler) • Clinical assessment: NB to make an accurate pathological Dx. Too often broad terms like “swimmers shoulder” or “Runners 'knee” are used Enables better explanation to sportsman of way forward. Enables optimum treatment Enables optimum rehabilitation. Diagnosis • Special Investigations – Should be a tool confirm or exclude a diagnosis not a replacement of a thorough physical examination. – Old saying by James M Hunter “Treat the patient and not the X-Ray” – Radiological Investigations • • • • • X-ray CT scan MRI Ultrasound Radio isotopic Bone scan Special Investigations • Neurological Investigations EMG Nerve conductivity Neuropsychological testing (head injuries) • Muscle assessments Compartment pressure testing • Cardiovascular Investigations • Respiratory Investigations Pulmonary function tests Treatment • Randomized controlled trial evidence for all treatments given? • Eg Parachute • We must take note of evidence that is around but never forget our craft remains much an art as science. • Standard principals – Acute management RICE RICE • Rest: First 48hrs Sportsman • Ice: Reduce tissue metabolism – Reduced hematoma, inflammation & tissue necrosis – Accelerated early regeneration in Muscle tissue – 20min every 2hrs • Compression: – Co-adhesive bandage or Compression sleeves • Elevation – Decrease in hydrostatic pressure Reduces accumulation of interstitial fluid Immobilization • Earlier better • Too lengthy leads stiffness degeneration, osteopenia, muscle atrophy etc. • Braces, POP, Crutches • CPM (Forms part of in hospital post operative rehabilitation) Therapeutic drugs • Analgesics : Relieve patients pain immediately post injury • Corticosteroids: Concern regarding the effects on tissue healing – Considered a bridge treatment i.e. providing immediate symptomatic relief but underlying cause of problems must be addressed • NSAID’s : Debatable effects – Avoided in first 48hrs – Long term use (more than 5 days) should be avoided. Reassess & diagnose – Be aware of gastrointestinal problems. Acute or Chronic Musculoskeletal Injuries Are antiinflammatory signs & symptoms present ? Previous History adverse effect Non-NSAID’s Analgesic YES YES NSAID’s combined with protective agent No No NSAID’s for max of 7 days NSAID’s not indicated Additional Treatments • • • • • • Electrotherapy Extracorporeal Shock therapy Manual therapy Acupuncture/ dry needling Hyperbaric Oxygen therapy Surgery Rehabilitation RETURN TO SPORT Skill Acquisition Proprioception Strength Flexibility Motor re-education & Muscle activation Correct Motor control • Poor pelvic control i.e. weak Gluteus medius can cause anterior knee pain • Poor scapular control can be cause of ant shoulder tilting causing impingement • Exercise in open or closed chain (more functional) • Remember agonist and antagonist Flexibility • Pre Event Active warm-up • Post event Passive cool down stretch • Tight muscles may be associated with injuries – Psoas :Lumbral apophyseal joints and Hamstring – Soleus : Achilles tendinopathy – Vastus Lateralis ITB : Patellofemoral syndrome Therapy progression Parameters to monitor • Pain & tenderness • ROM • Swelling • Heat & redness • Ability to perform exercises • Number of sets and reps Psychology • • • • • • Athlete must understand injury full extend Long term goal Short term goal Listen to Athlete Give alternate active rest exercise Refer if needed Recovery Common methods (Research needed) • Warm Down • Ice baths (5min 10 – 15 degrees) • Massage • Compression garments • Lifestyle factors • Nutrition • Psychology Most Common Injury summaries 1. Head - Concussions • Direct blow to head • Rapid onset of short lived impairment of neurological function • Good clinical judgement must prevail over guidelines and coach and player insistence. • When in doubt refer. • Assessment forms: 1.FIFA (SCAT2) www.bjsm.bmj.com (pocket edition) – 2. SA Rugby Bok Smart program: Concussion Management 2.Shoulder Injuries • • • • • • Rotator cuff Instability Labral injury Stiffness AC Joint Pathology Referred Pain Rotator cuff Muscles and Tendons • Acute or Chronic • Acute on Chronic ie. An acute tendon tear on a degenerative tendon • Symptoms: Shoulder pain – Overhead activity problems • Investigations: MRI • Treatment: Full thickness tear - repair – Tendons NSAID’s at first – Correct abnormalities: Muscle weakness, Glenohumeral rhythm etc…. Shoulder instability • • • • On field dislocations Reduce ASAP Damage to Capsule and Labrum (Ant, Post, Sup) Periscapular Muscle weakness Changes to passive structures ie lig, capsule or labrum • Ant Dislocations damage the labrum (Bankart lesion) • Symptoms – Pain, unstable, Weakness, Stiffness • Treatment – Non surgical – Rehabilitation and analgesic Rx – Surgical – Post operative rehab program Labral Injury • Overuse or acute • Intervention: Surgical since Conservative usually unsuccessful • Symptoms: – Impingement or Joint pain – May be unstable – History is NB on mechanism of injury – Common traction on Biceps tendon Shoulder Stiffness • May be secondary to trauma • Adhesive capsulitis or Frozen Shoulder • Possible injury to cervical nerve roots or brachial plexus • Treatment: – Conservative Rehabilitation – Manipulation Soft Tissue Acute Injuries eg. Post Thigh Sudden onset like a puncture! Return to sport 8 -25 days High re-occurance rate Key = correct Dx Anatomy History Strong incident ie sprinting (eccentric) or overstretching (ballet) None consider referred pain Special investigations : confirm grade of tear Ultrasound, MRI Management First 48hrs – RICE, early pain free M contractions Following: Stretching: Hamstring & Antagonists (Quads Iliopsoas) Neural Mobilization Soft tissue Rx Strengthening Sport specific drills esp. Agility and motor control 3.Anterior Knee conditions 7. ITB 1.OA Knee 6. Lat Lig. 2. Med Lig 5.General knee effusion 3. Pes Anserine bursitis 4. Patellar tendon / Osgood-Schlatters / Runners knee Knee injuries Medial menisci tear Patellar tendon rupture # Tibial Plateau MCL Sprain Quadriceps tendon tear Avulsion # tibial spine ACL sprain/rupture Acute patella femoral contusion Osteochondritis dissecans Knee Injuries Lateral Menisci tear LCL sprain Osteochondritis dissecans PCL Acute fat pad impingement Regional Pain Syndrome Patellar dislocation Avulsion biceps femoris tendon Quadriceps rupture Acute knee injury pricipals Is the injury significant ie fast intervention History to consider: Mechanism of injury Amount of pain Swelling & timing of onset Degree of disability Previous injuries Diagnosis knee injury Assessment: ? Damaged structures Extent of damage Degree of joint limb disability to provide safe and timely management Hints Symptom of ‘give way’ (ACL) Location of pain – Cruciate poorly localized Collaterals fairly well localized Severity of pain not always in corralation with injury severity Intra articular swelling obvious within 2 hrs damage - ACL,PCL - Pateller dislocation - Osteochondral # - Medial menisci peripheral tear Hints Effusion develops after a few hours Reactive synovitis ie. meniscal or chondral injuries Little effusion with collateral injuries Pop or snap or tear : ACL Locking : Loose body or displaced meniscal tear Lower leg Injuries • ‘Shin splints’ • Deep compartment muscle strains • Gastrocnemius / Soleus strains / tears • Achilles tendinosis or ruptures • ‘Severs’ disease Tibialis Anterior Tibialis Posterior FDL Gastrocnemius /Soleus & Achilles Sport specific injuries • Always consider the type of sport played • Level of sport ie international, national or local • Is sport the players income? • Surface where injury occurred • Gear involved • Training regime Rugby injuries Are you Listening? • Your patient is the answer to your diagnosis • Your Diagnosis is the answer to your successful treatment • So Listen Sources • Clinical Sports Medicine Fourth edition Brukner & Khan Jacq1@mweb.co.za 0123466909 Complete Physio Brooklyn Pretoria