Cesarean Section Post
advertisement

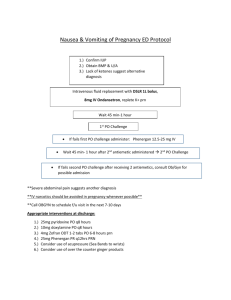
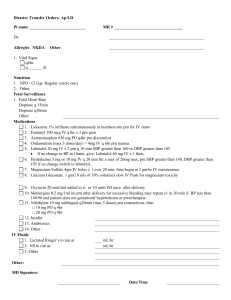
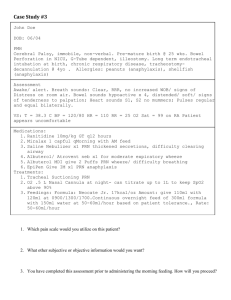
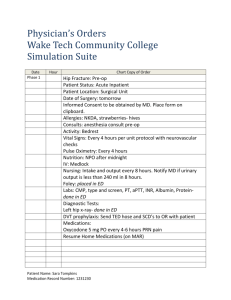
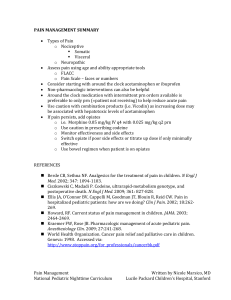
4N Labor and Delivery Cesarean Section Post-Op orders (OB) (Physician must sign all orders-check, circle and/or fill in appropriate blanks) Review orders in left window before entering new ones; discontinue or modify existing orders as needed Transfer to postpartum care 1-2 hours after delivery, following release by anesthesia 1. 2. 3. 4. Team Pager:________ Transfer to: __________ Diagnosis: Cesarean delivery, without mention of indication (669.7) Patient is delivered. All alerts in HEO that assume an ongoing pregnancy will be turned off with the execution of this order. Thank you for your cooperation NHO & vital signs for Pre-eclampsia: NHO & vital signs for All pts without BP, PIH, or HTN dx's/issues: 5. Notify house officer: T>: 100.4 T<: 95 SBP>: 160 SBP<: 100 DBP>: 100 DBP<: 50 HR>: 120 HR<: 50 RESP>: 24 RESP<: 10 UOP<: 120 ml/ 4h Other: Uop w/foley < 60ml/ 2h; if 02 sats <92% apply 02@ 2L NC and NHO; altered mental status; pain score >7 with current meds +Vital signs as directed q15 minutes x4; then if stable, q4 hours until discharge NHO & vital signs for ALL pts without BP, PIH, OR HTN dx’s/issues: 6. Notify house officer: T>: 100.4 T<: 95 SBP>: 150 SBP<: 100 DBP>: 100 DBP<: 50 HR>: 120 HR<: 50 RESP>: 24 RESP<: 10 UOP<: 120 ml/ 4h Other: Uop w/foley < 60ml/ 2h; if 02 sats <92% apply 02@ 2L NC and NHO; altered mental status; pain score >7 with current meds +Vital signs as directed q15 minutes x4; q4 hours X 3, then if stable, q8hours until discharge Treatment and Care Reminders *Tdap vaccine will be ordered for your postpartum patient, even if breastfeeding. Only cancel if given in past 10 years* 5. NURSING: postpartum assessment: assess fundus and lochia q4hours x 24 hours, then q8 hours until discharged 1 of 4 pages Initials_____________ Date ____/____/____ Time____:_____ Cesarean Section Post-Op orders (OB) (Physician must sign all orders-check, circle and/or fill in appropriate blanks) If newborn is admitted to NICU order breast pump for patient (unless contraindicated for medical reason). Initiate patient's breast pumping within 4-6 hours after delivery. Educate patient on use of breast pump no separation care Foley- remove per d/c protocol to bedside drainage; discontinue 16 hours after section or when epidural is discontinued Intake and output record discontinue when patient has spontaneously voided x3, with volume greater than 200 mL In and out cath if unable to void spontaneously within 4 hours of foley removal Turn/cough/deep breath q2h w/a no routine incentive spirometer is to be ordered Ambulate assist with ambulation 4-6 hours post c-section or in early am Ambulate at least tid Aromatic ammonia spirit inhal: 1 ea inhalatn prn (prn pre-syncope/syncope) Discontinue: IV when tolerating po and voiding successfully after foley removed Lidocaine 1% injection: 0.2 ml intrderm as dir (PRN anesthetic for IV start per patient preference) Clear Liquid diet daily X 6 hours no ice chips Advance diet to reg May liberalize diet 6 hours postop in c-section patients with low risk of complications Obtain acticoat moisture control silver dressing, to be placed post-operatively on all c-section incisions unless Dermabond is used. Sequential compression device off 1h q8h The Dept of OB/GYN recommends SCD's for all pts undergoing a C/S regardless of DVT and PE risk factors Complete Edinburgh Postnatal Depression screen 1 within 24 hrs post delivery (located in Star Panel). For non-English speaking pts, the language line must be used for screening assessment Tdap (tetanus/diphtheria/acellular pertussis) vaccine- booster 0.5 ml im as dir discharg (Call Pharmacy to order Tdap prior to discharge) 6. Consult: acute pain service 7. Lactation consultant if needed 8. Discharge instructions This OB pt was assessed & is a candidate for Discharge plus she delivered prior to 8pm.The Newborn Nursery & 4E nursing should be prepared for discharge home the day after her SVD (PPD1) or 2 days after her C/S (POD2) Discharge instructions please communicate the discharge notice to the newborn nursery 9. Discharge instructions No home health visit needed *Cord Gases do not need to be reordered if part of the admission orders. Only add these orders if not 2 of 4 pages Initials_____________ Date ____/____/____ Time____:_____ 4N Labor and Delivery Cesarean Section Post-Op orders (OB) (Physician must sign all orders-check, circle and/or fill in appropriate blanks) previously entered* 10. NURSING: Send fetal CORD blood gases (NOT maternal ABG): if fetal compromise, 5 minute apgar < 7, severe IUGR, maternal thyroid disease, abnormal fetal heart tracing, intrapartum fever, and/or multifetal gestations. Fetal Cord Blood Gas Arterial x1 (if indicated by L&D protocol) Fetal Cord Blood Gas Venous x1 (If indicated by L&D protocol) Lab 11. PCV BLD as dirx36 hours (pcv to be drawn once - 24 hours post c-section) For Rh negative mother with Rh positive infant 12. Fetal blood screen + RHO (D) Immune Glob: Rhophylac 300 mcg im x1 =+24h (to be given postpartum to Rh negative mother with an RH positive baby) IV Fluids 13. LR at 125 ml/hr 125 ml/hr iv 14. D5 LR at 125 ml/hr 125 ml/hr 15. Heparin 100UNITS/ML FLUSH SOLN (prefilled syringe) 3 ml flush q12h (flush each shift) + Heparin 100 UNITS/ML FLUSH SOLN (prefilled syringe) 3 ml flush prn (PRN after each access) For diabetic patients 16. D5 1/2 NS: 125 ml/hr iv now (discontinue when tolerating po and when voiding successfully after foley removed) Medications 17. Docusate sodium: colace 100 mg po qhs prn (give for constipation) 18. Milk of magnesia: MOM 30 ml po qday prn (for constipation) 19. Ibuprofen: motrin 600 mg po q6h prn (PRN pain score 1-2, or PRN cramping pain) 20. Simethicone: 80 mg po tid prn (for excess gas / bloating) 21. Acetaminophen: tylenol 650 mg po q6h prn (PRN headache; review all formulations that contain tylenol, do not exceed 4000mg per 24hrs) 22. Promethazine: phenergan 25 mg po q4h prn (PRN nausea/vomiting, for patients without IV access) 23. Ondansetron injection 4 mg iv q6h prn (prn nausea/vomiting, pts with IV access.) 3 of 4 pages Initials_____________ Date ____/____/____ Time____:_____ Cesarean Section Post-Op orders (OB) (Physician must sign all orders-check, circle and/or fill in appropriate blanks) 24. Oxycodone: 5 mg po q4h prnx3 days (prn for pain score 3-6; may repeat x 1 if pain score 3 or greater one hour after administration.) SECOND TIER PAIN MED 25. Oxycodone: 10 mg po q4h prnx3 days (prn for pain score >7.) THIRD TIER PAIN MED 26. Nursing: If pt has persistent pain score > 6 after receiving oral pain meds, may give Demerol per order. Administer anti-emetic for nausea prophylaxis per order. 27. Demerol 50mg po q3hr prn pain x 24hrs. May repeat x 1 within 1st hour if pain score > 4 do not exceed 8 tabs If not immune to Rubella: 28. Measles-mumps-rubella; MMR-II 0.5 ml subcut as dir @ discharge (Call Pharmacy to order MMR prior to discharge) Diet 29. Regular diet daily until d/c 30. Diets (VUH) Postpartum Educational Videos 31. Video: Postprtm care for Yrslf 32. Video: Understanding Newborns 33. Video: Your Breast Fdng Rltnshp 34. Video: Early Infant Loss Postpartum Hemorrhage 35. Postpartum Hemorrhage (OB) Physician Signature: Date: ____________ Time: ______________ 4 of 4 pages Initials_____________ Date ____/____/____ Time____:_____