Hemochromatosis - Morgan Millett, FNP-S
advertisement
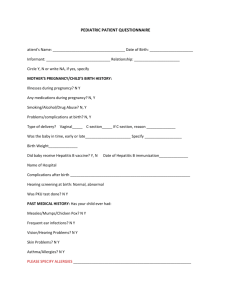
Case Study Morgan Millett, FNP-S Client/Source/CC • Patient is N.S., 28 year old G2 P1 African American female • Source was office visit. Patient was 25 weeks pregnant, coming in for a problem visit. • Chief Complaint: “abd pain, N/V/D, unable to keep anything down.” History of Present Illness • Patient is a 28 year old G2 P1 female who presented to the office with complaints of N/V (c/o she has had since 12 weeks pregnant in which she has been in and out of the hospital for) that has worsened over the past week, in which she is now unable to keep anything down. She also has diarrhea, upper abd pain, 8/10, weight loss >10% and fatigue. Nothing makes abd pain better, but pain is much worse after eating and not relieved by vomiting. She is unable to work, and barely able to complete ADL’s. She denies fever, chills, & being around anyone ill. What are we thinking ??? • Hyperemesis??? N/V • GI bug- less likely as she has been sick her whole pregnancy • Preeclampsia??? Epigastric pain • Abruption??? Abd Pain • Diverticulitis??? Pain • Pancreatitis??? Pain, Nausea Past Medical History • Benign Pancreatic cyst diagnosed in 1999 requiring surgery x2 to drain, no complications in 10+ years • Severe hyperemesis with first pregnancy • Hyperemesis occurs in only about 1% of pregnancies- however if you have it in your first pregnancy, there’s a 48% recurrence chance • No other PMH Social History • Does not smoke or use illicit drugs • Does not drink alcohol Family History • Father: HTN • Mother: None • Only child • Has 3 year old daughter at home, healthy. Allergies & Medications • Allergies: She has no known drug allergies. She denies allergies to food, environment, and latex. • Medications: • Prenatal vitamins Review of Systems • General: fatigue, weight loss • Respiratory: Patient denied a history of respiratory infections, cough, recent chest xray, exposure to TB, difficulty breathing, wheezing, and night sweats. • Mouth/Throat: Patient denies taste disturbances, excessive dryness, and sore throats. • Cardiac: She denied hypertension, heart murmurs, chest pains, palpitations, and dyspnea. • Gastrointestinal: She reports N/V/D, food intolerance, and abd pain. She denies heartburn and constipation. ROS continued • Hematological: Patient denied unusually bleeding/bruising, history of anemia, and history of blood transfusions • Neuro/Musculoskeletal: Patient denies headache and pain/neck stiffness. She denied back pain, paralysis, and deformities. • Psychiatric: Patient denied a history of anxiety and depression. She denied nightmares, insomnia and mood changes. • Endocrine: Patient reported benign pancreatic cyst. She denied thyroid problems, cold/heat intolerance, polydypsia, and polyuria • Skin: Patient c/o very itchy skin. Physical Exam • General: Underweight, 28-year-old female who is alert, oriented, and cooperative. FHR 135. • Vitals signs: T 98.6, BP 110/58, HR 82, R 20, O2 98% on room air. Height: 5’7” Weight: 110#. BMI 17.2 • Thorax/Lungs: Respiratory rate is equal and regular. Lungs are clear to auscultation in all lobes. No rales, rhonchi, or wheezes appreciated. Physical Exam Continued • Cardiovascular: S1 and S2 present in APETM with bell and diaphragm. Regular apical rate. No heaves, thrills, murmurs, rubs, or gallops appreciated. • Abdominal: Gravid, symmetrical, soft. Umbilicus midline. Auscultation yields bowel sounds x4 quadrants. No aortic, renal, iliac, or femoral bruits. Difficult to assess for organomegaly r/t pregnancy. No CVA tenderness, guarding or rebound tenderness. Pain in RUQ, not worsened or relieved by pressure, radiating to back. • Skin: Warm and dry. Visually excoriated r/t patient constantly itching. Slightly yellow tinged, but otherwise appropriate for race. Assessment/Plan • Admission to hospital- fluids for dehydration • CMP, CMP, LD & Uric acid, urine analysis (r/o pre-e & electrolyte imbalances r/t hyperemesis) • Ultrasound (r/o abruption) • Consults: GI & Nutrition Consult • Nutrition- recommended TPN during hospital admission • GI consult- GI would see her outpatient 4-6 weeks after delivery for f/u on questionable pancreatic cyst issues Lab Results • Patient was anemic- H/H= 7/25 • Her alk phos= 96 U/l (normal 37-98) • An increase of 2 to 3 times normal alk phos may be observed in women in the third trimester of pregnancy, although levels may not exceed the upper limit of the reference interval in some cases. The additional enzyme is of placental origin. • Her albumin (ordered by GI to determine protein absorbtion r/o kidney & liver diseases)= 2.5 g/dL (3.4-5.4) • Labs were otherwise all normal. Differential Diagnosis • Hyperemesis- N/V, weight loss • Preeclampsia- likely not r/t labs and BP • Abruption- likely not r/t normal u/s and no vaginal bleeding • Diverticulitis- no fever or bowel issues • Pancreatitis- nausea, pain • Kidney/liver diseases Plan • Inpatient management until delivery • PT for to reduce muscle wasting • Pain management for medications to keep patient’s pain controlled • Nutrition: start TPN with lipids Delivery & beyond • Patient remained inpatient for 7 weeks and was induced for worsening weight loss and pain issues. She had a normal uncomplicated vaginal delivery of a baby boy at 32 weeks, who went to NICU. • She had a rough two day recovery on the postpartum floor, still having the same complaints. • Finally, she had her CT scan….. Pancreatic Cancer (157.9) • Carcinoma of the exocrine pancreas is the 4th most common cause of cancer deaths in the US. • It is rarely curable; overall 1 year survival rate is 25%, 5 year is 5%. • 60-70% of cancers occur in the head of the pancreas • For advanced or unresectable cancers, survival is <1 year at five years but most patients die within one year • Median age for diagnosis is 72. Rare < age 45. Occurrence rises sharply after 45. Incidence • In 2009, an estimatd 43470 people were diagnosed with pancreatic cancer; 35240 deaths. • AA men 16.7/100,000 AA women 14.4/100,000 • 10.3/100,000 White men & women Risk Factors Smoking Diabetes Genetic factors Chronic pancreatitis Non-O blood type High intake of dietary fat Obesity Alcohol consumption Clinical Manifestations • Weight loss- 90% • Pain- 75% • Jaundice- 70% • Diabetes- 15% • Malnutrition- 75% • Anorexia- 60% • Weakness/fatigue- 30-40% • Dark urine How is it diagnosed? • Routine labs may indicate increased serum bilirubin and alkaline phosphatase, anemia, and decreased serum albumin • CT scan using thin section, multiphase multidetector heliac is choice for diagnosis and staging. • Abd U/S: to assess jaundice and duct dilation Tumor Staging • Stage I: Limited to the pancrease • Stage II: Regionally invasive; may involve lymph nodes but without celiac or mesentaric artery involvement • Stage III: Direct involvement of celiac or superior mesenteric artery • Stage IV: Distant metastases Treatment • Surgical resection: Only chance of cure; no role for resection in metastatic disease. As few as 15-20% of patients are candidates for resection. • Whipple procedure: en bloc resection of the head of the pancreas, distal common bile duct, duodenum, jejunum, and gastric antrum • Criteria for unresectability: extrapancreatic spread, encasement or inclusion of major vessels, distant metastases. Management • Stage I & II: Radical pancreatic resection with chemotherapy • Stage III: Chemotherapy and radiation • Stage IV: Chemotherapy; pain relieving procedures such as celiac nerve block, supportive care, palliative decompression Outcome • This patient passed away within two months of her diagnosis. • Her pregnancy masked common symptoms, especially because she had hyperemesis with her first pregnancy. • CT scan delayed because of pregnancy. References: • Berry, L. (2014). Pancreatic Cancer Diagnosis Delayed in Patients Under 55 Years Old. The Journal of Cancer Nursing Practice, 13(5), 7. • De La Cruz, M., Young, A., Ruffin, M. (2014). American Family Physician, 89(8), 626-32. • Domino, F. (2014). The Five Minute Clinical Consult, 22nd ed. Philadelphia, PA: Lippincott, Williams, & Wilkins. • Hartman, D. J., & Krasinskas, A. M. (2012). Assessing Treatment Effect in Pancreatic Cancer. Archives Of Pathology & Laboratory Medicine, 136(1), 100-109.