dealing with Food Allergies and Anaphylaxis at California Schools.
advertisement

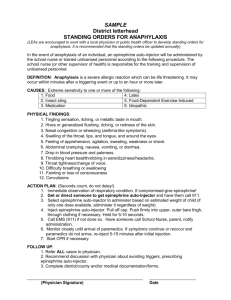
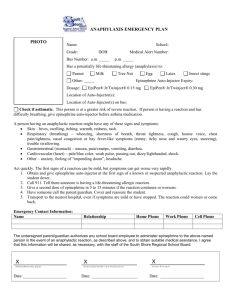
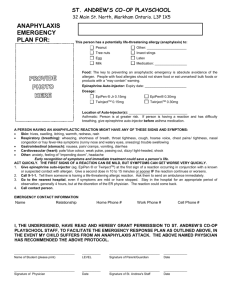
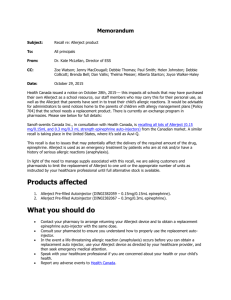
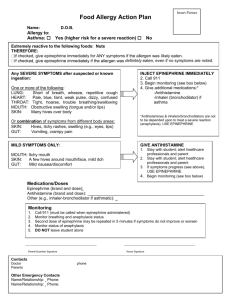
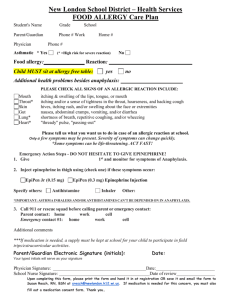
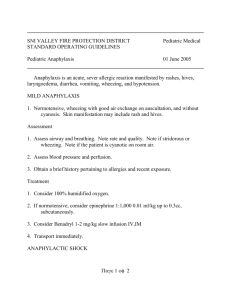
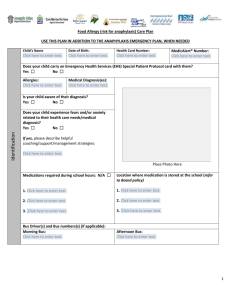
Dealing with Food Allergies and Anaphylaxis at School Cathy Owens, RN, M.Ed, NCSN, ERSN Credentialed School Nurse/Coordinator of Health Services Murrieta Valley Unified School District National Epinephrine Resource Nurse cowens@murrieta.k12.ca.us /(951) 696-1600 ext 1027 Food Allergies-A National Concern • On November 13, 2013, President Obama signed into law the School Access to Emergency Epinephrine Act • The federal legislation provides an incentive for states to enact their own laws allowing school personnel to keep and administer a non-student specific epinephrine autoinjector in case of an emergency. The Duty of Schools • Provide a safe environment for children • Act appropriately in an emergency Keeping students safe-it is our most important responsibility! Why this matters to me…. A few students we have lost to anaphylaxis Ammaria Johnson Katelyn Carlson Natalie Giorgi SB 1266-A life saving law “Peanuts” 1970’s “Peanuts” Today • Allergies tripled in past 15 yrs • More severe reactions • One in 5 reactions are without a known allergy/trigger • First reaction is often (20-25%) at school » Dr. Allen Lieberman 2014 What we know… • In 2006, about 88% of schools had one or more students with a food allergy • According to the CDC (2013), the prevalence of food allergies among children increased 50% during 1997–2011 • Nearly 20%-25% of school aged children with food allergies had their first reaction in school! • Children spend almost half their waking hours in school-out of their parents’ care • Failure to promptly treat food anaphylaxis without epinephrine is a risk factor for fatalities. So, what are some of the challenges? • Lack of school nurses • Inability to get prescription • • • Lack of school wide food allergy plan – Classroom Issues – Storage-locked vs unlocked – Cafeteria/Field trips Lack of trained staff – Resistance of staff to administer it –when to give, which one (Jr or Reg) – “Epinephrine is dangerous” – Should Benadryl be given first? IHP, ECP, 504-which one?? Lack of School Nurses • EC Section 49414(a) requires a school district, county office of education, or charter school to provide emergency epinephrine auto-injectors to school nurses and trained personnel who have volunteered • Without a school nurse-districts can avoid providing this life saving protection for students – Students in these districts are at RISK! • School nurses develop plans, communicate with physicians and parents, train staff, ensure safety precautions are in place • School nurses supervise the health and safety of all students Food allergy plan Every school should have a plan to address food allergies • Plan should include: – Classroom snacks/treats/ food – Medication storage/access – Kitchen/cafeteria issues – Field trips – Training – Emergency response plan • CDC has an excellent guideline for schools and anaphylaxis – http://www.cdc.gov/healthyyouth/foodallergies/pdf/13_243135_A_Food _Allergy_Web_508.pdf CDC Guidelines Food Allergy Management and Prevention Plan 1.Ensure the daily management of food allergies for individual children. 2.Prepare for food allergy emergencies. 3.Provide professional development on food allergies for staff members. 4.Educate children and family members about food allergies. 5.Create and maintain a healthy and safe educational environment. Classroom issues • There should be a classroom policy on food/snacks – Parents should be notified PRIOR to any party/snacks! – Parental notification regarding students with allergies – Risk can be reduced by encouraging other parents to reduce/eliminate offending foods in their child’s lunch Food allergens are often ‘hidden’ – Unable to screen every child’s lunch No use of food for rewards Classroom issues-Con’t • Classrooms are often used by outside groups (churches, girl scouts, etc.-food may be eaten on desks) • Cleaning of desk surface? • Hand washing policy – Wash hands before and after eating? Storage/Access • Medication should be kept in an UNLOCKED, but secure cabinet/place • CLEARLY marked on outside of cabinet • Students and backpacks are ‘moving targets’ – Backpacks all ‘look’ the same-critical seconds could be lost • Classroom may be locked at time of highest need Cafeteria/Kitchen issues • Food preparation-Kitchen Staff should be fully trained and aware • All peanut product food should be prepared/served away from other food • NO cross contamination • Allergy Safe Tables-pros and cons • Paper placemats Field Trips • Plans should be developed for off campus activities • Epinephrine auto-injector should always go along for students with identified allergies/prescribed medication • Staff needs to be trained for signs and symptoms and how to act in an emergency Lack of Trained Staff • Staff must ‘volunteer’-but not as restrictive as Diastat law – Notification must be done annually • Training should include when to give (if no known history) – For student with KNOWN allergy-if they have any serious symptom-GIVE epi – For students with NO known history-generally should have 2 or more symptoms • Fears that epinephrine is dangerous – “if 911 is needed”-but due to biphasic concerns – Dosage concerns (55 lbs vs 66 lbs) – What if given when not truly needed Volunteer Agreement Notification of Volunteer Agreement for training in administration of Epinephrine auto-injector Current law (SB 1266) now requires schools to provide emergency epinephrine for individuals who may be experiencing anaphylaxis. Anaphylaxis is a severe allergic reaction which can occur after expose to an allergen, an insect sting or even (rare) after exercise. Without immediate administration of epinephrine and summoning Emergency Medical Services (911), death could occur. Certain individuals may experience anaphylaxis that have no known previous history an allergy and therefore, may not have their own prescription. Legislation allows for a school nurse or a trained volunteer to administer an epinephrine autoinjector to an individual who is exhibiting potentially life-threatening symptoms of anaphylaxis after exposure or ingestion of an allergen. Training will be provided to the volunteer on signs and symptoms of anaphylaxis, how to administer the epinephrine auto-injector, calling EMS (911) and any follow up documentation or actions required. Staff members who volunteer to be trained are protected under the law and will provided defense and indemnification by the school district for any and all civil liability. This notification is provided annually to all staff. If you are willing to be identified as a volunteer and be trained, please complete the section below and submit it to your site administrator. ____________________________ __________________________ ____________ Signature Printed Name Date Epinephrine auto-injectors “No contraindications, no serious, harmful side effects if overused” “Too much better than too little” “Too little better than none” “Expired better than none at all” Who should be Trained? • Office/Health staff • Teacher/classroom staff • Playground supervisors • Transportation staff • Kitchen/cafeteria staff • Anyone who provides care of student • CSNO has an training packet including PPT • NASN has a training program ‘Get Trained’ NASN-Get Trained www.nasn.org Epinephrine is the first line treatment for anaphylaxis • Should be administered IMMEDIATELY Some protocols call for epinephrine to be administered with or without symptoms Parents & school administrators should not be concerned about adverse health effects of epinephrine – it has an impressive safety profile When in doubt – give the epinephrine Adverse effects for average healthy child not harmful – anxiety, palpitations A delay in treatment can have devastating results Schoessler & White, 2013 Robinson & Ficca, 2011 Sicherer & Simons, 2007 NASN-Get Trained (sample slide) CDE Training Guidelines “Person suffering or reasonably believed to be suffering for an anaphylactic reaction” • Techniques for recognizing symptoms of anaphylaxis. • Standards and procedures for the storage, restocking and emergency use of epinephrine auto-injectors. • Emergency follow-up procedures, including calling the emergency 911 phone number and contacting, if possible, the pupil's parent and physician • Recommendations on the necessity of instruction and certification in cardiopulmonary resuscitation. • Instruction on how to determine whether to use an adult junior epinephrine auto-injector, considering pupil’s grade level or age as a guideline of equivalency for the appropriate pupil weight determination Recommendations for CPR CPR certification is recommended However, it may present a roadblock to training staff • Due to lack of staff who are CPR certified/ or willing to volunteer • Only health professionals, coaches, bus drivers and a few other positions ‘required’ to have CPR • Cost to districts to have to provide certification • Training should at least include ‘training’ in CPR (review of steps/what to do) Epinephrine auto-injectors Requires a qualified supervisor of health to obtain from an authorizing physician a prescription for epinephrine autoinjectors • that, at a minimum, includes, for elementary schools, one regular epinephrine auto-injector and one junior • For junior high schools, middle schools, and high schools, if there are no pupils who require a junior epinephrine autoinjector, one regular epinephrine auto-injector. • Qualified supervisor of health shall be responsible for stocking the epinephrine auto-injector and restocking it if it is used (within 2 weeks after use) Inability to obtain prescription • School districts are having difficulty finding a physician to write orders • Hesitancy from physicians because they are not the physician of record for individual who may need epinephrine (questions regarding training, etc.) • SB 738 –amendment that provides indemnification for physicians who write order - "An authorizing physician and surgeon shall not be subject to professional review, be liable in a civil action, or be subject to criminal prosecution for the issuance of a prescription or order pursuant to this section, unless the physician and surgeon’s issuance of the prescription or order constitutes gross negligence or willful or malicious conduct." • Standing orders should be standardized to reduce liability concerns Obtaining epinephrine auto-injectors • Need to submit a prescription • Can obtain two 2-packs: – .15 mg or 0.3 mg • http://www.epipen4schools.com/ • Auvi Q now has a school program (California only) www.directrelief.org/auvi-q/ Types of Plans… ‘Alphabet Soup’ Student with Food Allergy may qualify for any of these…. • IHP-Health Care plan designed to address specific medical condition or treatment protocol • ECP- Emergency Care plan designed to give directions on how to recognize and act in emergency (allergic reaction) • 504-Federal anti-discrimination law-(equal access) part of American with Disabilities Act • IEP-Educational plan to address student’s academic needs with consideration of handicapping condition IHP-Sample form School Year ______________ Murrieta Valley Unified School District Health Services Individualized Healthcare Plan Anaphylaxis-Food Allergies Student Name: _________________________________ DOB ___________ School:______________________ Parent/Emergency Telephone Numbers: __________________________________________________________ Physician Information: _________________________________________________________________________ Medical Information:___________________________________________________________________________ _____________________________________________________________________________________________ Background Information: Anaphylaxis is a sudden, severe, potentially fatal, systemic allergic reaction that can involve various areas of the body (such as the skin, respiratory tract, gastrointestinal tract, and the cardiovascular system). Onset may be sudden (generally within minutes to two hours after contact with the allergy-causing substance such as foods, bee stings, chemical or medications, but may occur up to four hours after contact). Allergic reactions may be mild to life threatening. Patients with asthma are those most at risk for life-threatening anaphylaxis events. • If any difficulty with breathing or cardiac symptoms (such as fainting, turning blue, etc) – GIVE Epinephrine auto-injector and CALL 911 •Other Symptoms may include: • Tingling sensation, itching, or metallic taste in mouth. • Hives or generalized flushing, itching, or redness of the skin. • Nasal congestion or wheezing (asthma-like symptoms). • Swelling of the throat, lips, tongue, and around the eyes. • Feeling of apprehension, agitation, sweating, weakness or shock. • Abdominal cramping, nausea, vomiting, or diarrhea. •Drop in blood pressure and paleness. •Throbbing heart beat/throbbing in ears/dizziness/headache. •Throat tightness/change of voice. •Procedure •Get epinephrine auto-injector (seconds count!) 2nd grade and below-use .15 mg (junior) 3rd grade and above –use .3 mg If no junior-Use regular despite age • Pull off safety cap • Inject auto-injector (push tip) into side of thigh (can go through clothing) •Hold in place for 10 seconds (if removed earlier-most of medication has injected) •CALL 911 • Have someone contact school nurse and parent •.Stay with individual, keep them calm, monitor breathing • If symptoms re-occur and paramedics have not arrived (10-15 minutes later), re-inject with 2nd autoinjector •Document on log according to orders. •Special Considerations:_______________________________________________________________________ ____________________________________________________________________________________________. Prepared by:___________________________________Credentialed School Nurse Date__________________ Revised 9‐2015 Emergency Care Plans •Schools should have an emergency plan •For known and UNKNOWN cases of anaphylaxis •People with a prescription for epinephrine do not always carry/provide an auto-injector Studies show that they only have them approximately 55% of the time Stock epinephrineSAVES lives! Section 504 -definition • Plan outlines accommodations needed for the student to be safely included in all school activities • “Any person who has a physical or mental impairment that: – substantially limits one or more major life activities, – has a record of such impairment, – or is regarded as having such impairment.” • "No otherwise qualified individual with a disability in the United States . . . shall, solely by reason of her or his disability: – be excluded from the participation in, – be denied the benefits of, – or be subjected to discrimination under any program or activity – receiving Federal financial assistance . . . ." Section 504 Plan • District is responsible to notify parents annually and are responsible to refer students who may have disability • Evaluation is required to determine if qualifies • Requires team meeting (can take time to schedule) • Team develops written plan re: aids, services, and necessary providers to ensure FAPE • Includes two key components – Accommodations so student can participate in school activities – ECP-how to recognize and allergic reaction • Written plan will be provided to parent All district personnel who work with student must be informed of plan Updates/changes to 504 • On September 25, 2008 President Bush signed into law the American with Disabilities Amendment Act (ADA) of 2008. • The actual language of the definition remains the same but the Act expands the meaning of “disability” Even if an impairment that is episodic or in remission-can meet the “disability requirement” if it substantially limits a major life activity when active. (often times anaphylaxis is considered ‘episodic’ and therefore, students are denied 504 accommodations) What School Nurses Can Do • Epinephrine auto-injectors should be available at all sites • Every school should identify trained personnel • School nurses should train other staff to recognize and treat anaphylaxis • Emergency care plan with standing orders should be developed – Written protocol created for recognizing signs and symptoms and treating anaphylaxis – Procedures for calling 911 should be in place Most importantly…. Schools need to be prepared for students with anaphylaxis One life lost is ONE too many… Questions…. Sudden Cardiac Arrest • A student has no known hx of cardiac problems • He starts feeling anxious • He starts to run and within a couple of minutes… • He collapses and lay unresponsive on the field. ARE YOU PREPARED?? Automated External Defibrillators A life lost-but a legacy lives on What we know… • Nearly 360,000 sudden cardiac arrests occur outside of hospitals each year. • About 2/3 of the deaths in young people are due to heart abnormality • Less than 8% survive outside of hospital (without CPR/AED) • Abnormal rhythm-ventricular fibrillation – Most common causes: • Hypertrophic cardiomyopathy (most common) • Coronary artery abnormalities (congenital defect) • Long QT syndrome (inherited heart arrhythmia) • Commotio cordis –blunt blow to chest –causes VF Symptoms/Red flags • Unexplained fainting (syncope) during physical activity • Family history of sudden cardiac death • Chest pain/shortness of breath (usually not related to cardiac but to other underlying issues). • If frequent or increasing in severity, should be evaluated by a physician So, what are some of the challenges? • Lack of school nurses • Lack of trained staff-(cost/time) – Resistance of staff (fear) • Cost of equipment • Maintenance program • Lack of school wide/District AED policy AED Program in Schools Districts should have: • Program Advisory-policy and procedures • Board Policy • Training program • Monitoring program • Equipment (AED/Cabinets/Signage) Program Management • Districts should develop a Program Manual • Includes guidance in management of AED program-brochure provided annually to all staff • Responsibilities of Staff-calling 911 • Placement of AEDs • Maintenance program Storage/Accessibility Signage • Signs need to identify where AED is stored • Brochure must be located next to unit describing how to use an AED in 14 pt font Cabinet • Cabinet should be alarmed (but not locked) Maintenance • Need to do checks (per manufacturers specifications)-but at least every 3 months • Check for placement in cabinet • Check for light/battery indicator • Document according to District plan Field Trips/Sporting Events CORRECTION…!! • NO language regarding being available for all schoolsponsored school athletic events!! • However, for safety purposes, it would be good to consider a plan for sporting events/field trips Training • AB 2217-Ed Code 49417-provides liability protection • The principal shall ensure that the school administrators and staff annually receive information that describes sudden cardiac arrest, the school’s emergency response plan, and the proper use of an AED. • Requirement for school principal to designate trained employees who are available to respond-DELETED from current law • However, NO cost to employee for training if they volunteer and liability is provided Education Is Paramount • Educate School Board, Staff, and the Community at large for the need for AEDs! • Train and educate students and staff to be knowledgeable of CPR (besides certificationyou can provide overview/training to all staff) • Know how to act or train others on how to act • Work to support having AEDs in all schools