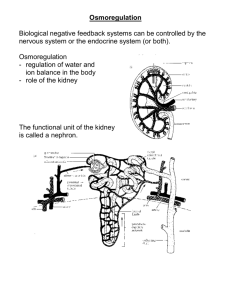
Urinary System
advertisement

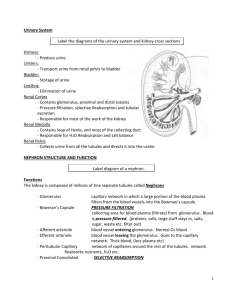
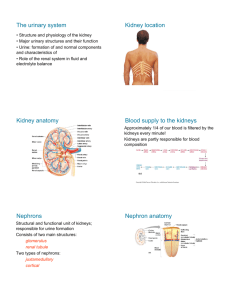
Urinary System Consists of: • • • • Kidney(s) Ureters Urinary Bladder Urethra Functions: • Filter gallons of fluid from bloodstream – Filter plasma 60 times/day • Responsible for removing: – Toxins – Metabolic Wastes – Excess ions • Regulates volume and chemical make up of blood • Maintains the proper pH between water, salts, acids and bases – Maintains blood pH between 7.35 – 7.45 Functions • Regulatory functions include: – Produce hormones Renin and erthropoietin – Renin helps regulate BP and kidney function – Erthropoietin stimulates RBC production in bone marrow – Assists in metabolizing Vitamin D to its active form. Kidney Anatomy • Kidneys are covered by fatty tissue; anchors kidneys to posterior wall • Internal Anatomy – 3 distinct regions – Pelvis – where kidneys join ureters; responsible for collecting urine – Renal Cortex – outer region; most of nephrons are found here – Medulla – Middle region; Renal pyramids Medulla • Nephron – Working Unit of Kidney; Carry out processes that form urine Nephron • Glomerulus – tuft of capillaries • Parts of Nephron – – Bowman’s capsule Renal Tubule - 3 cm in length • • • – Proximal Convoluted tubule (PCT) Loop of Henle Distal Convoluted tubule (DCT) Collecting Duct Urine Formation Involves 3 processes • Filtration glomerulus and Bowman’s capsule • Renal Reabsorption Carried out by renal tubules • Secretion Carried out by renal tubules • Glomerular Filtration – Blood enters via afferent arteriole (larger diameter) and leaves via the efferent arteriole – Difference in vessel diameter increases BP in glomerulus and assists with filtration • Podocytes (Bowman’s capsule) – surround capillaries • Passive, nonselective process where fluids and solutes are passed through a membrane • Force is cause by hydrostatic pressure – What caused pressure increase? • GFR (Glomerular filtration rate) is the amount of filtrate produced in the kidneys in one minute. • Renin regulates GFR by causing an increase in blood volume and blood pressure (Constricts blood vessels) • Filtration Pressure – Increase in BP at glomerulus forces water and solutes out of blood and into capsule. • What passes through? What remains in the blood? Filtrate is not Urine • Filtrate contains both wastes and needed water and solutes • Reabsorption begins as soon as nutrients enters the PCT • All water can’t be excreted, so tubules claim what it needs • Why is it called reabsorption and not absorption? What is reabsorbed? • 100 % of organic nutrients • Most electrolytes by facilitated diffusion • Water is passively reabsorbed – 60 – 70 % of fluid is reaborbed by PCT Rate and degree of reabsorption is regulated by hormones Problems: Hyperglycemia Where does Reabsorption occur in the nephron? • PCT are most active reabsorbers • The descending loop of Henle is permeable to water but not solutes • The ascending loop of Henle is impermeable to water and most solutes – Na and Cl are actively reabsorbed into the blood stream • DCT is impermeable to solutes • Reabsorption of Na, K, and water is controlled by hormones Na+ (65%) Glucose Amino acids H2O (65%) and many ions (e.g. Cl– and K+) Milliosmols Cortex (d) (a) 300 (e) Outer medulla (b) (c) 600 Some drugs – H+, HCO3 NH4+ Inner medulla Blood pH regulation 1200 (a) Proximal convoluted tubule: • 65% of filtrate volume reabsorbed • Na+, glucose, amino acids, and other nutrients actively transported; H2O and many ions follow passively • H+ and NH4+ secretion and HCO3– reabsorption to maintain blood pH • Some drugs are secreted Active transport (primary or secondary) Passive transport Figure 25.18a Reabsorption (b) The descending loop of Henle • Freely permeable to H2O • Not permeable to NaCl or other solutes • Filtrate becomes increasingly concentrated as H20 leaves by ____________? Active transport (primary or secondary) Passive transport Milliosmols Na+ Cl– K+ Cortex (d) (a) 300 (e) Outer medulla Urea Na+ Cl– (c) Ascending limb of loop of Henle • Impermeable to H2O • Permeable to NaCl • Filtrate becomes increasingly dilute as salt is reabsorbed (b) (c) 600 Inner medulla 1200 Active transport (primary or secondary) Passive transport Figure 25.18c Osmolality of interstitial fluid (mOsm) Active transport Passive transport Water impermeable Filtrate entering the loop of Henle is contains many substances that are needed in the body The descending limb: • Permeable to H2O • Impermeable to NaCl As filtrate flows, it becomes increasingly concentrated as H2O leaves the tubule by osmosis. The filtrate osmolality increases. H2O NaCI H2O NaCI H2O NaCI H2O NaCI Cortex Outer medulla H2O NaCI H2O H2O Inner medulla Loop of Henle The ascending limb: • Impermeable to H2O • Permeable to NaCl Filtrate becomes increasingly dilute as NaCl leaves, eventually becoming hypo-osmotic to blood . NaCl leaving the ascending limb increases the osmolality of blood. Figure 25.16a What’s left in the nephron? • Non-reabsorbed substances are: – Urea – 50 % is reclaimed; the rest is waste – Creatinine – a large lipid; insoluble molecule that is not reabsorbed at all – Uric Acid – 50 % is reclaimed; waste product of RNA synthesis Tubular Secretion – “Reabsorption in Reverse” • Urine is formed from filtered and secreted substances • Secretion occurs in the DCT tubules and collecting ducts – Hormones assist with this process • ADH (antidiuretic hormone) • Aldosterone • ANP Na+; aldosterone-regulated Ca2+; PTH-regulated Cl–; follows Na+ Milliosmols Cortex (d) (a) 300 (e) Outer medulla (b) (c) 600 Inner medulla (d) Distal convoluted tubule • Na+ reabsorption regulated by aldosterone • Ca2+ reabsortion regulated by parathyroid hormone (PTH) • Cl– cotransported with Na+ 1200 Active transport (primary or secondary) Passive transport Figure 25.18d Milliosmols Cortex H2O regulated by ADH (d) (a) 300 Regulated by aldosterone: Na+ K+ Blood pH regulation H+ Urea; increased by ADH (e) Outer medulla (c) 600 HCO3– NH4+ (b) Inner medulla 1200 (e) Collecting duct • H2O reabsorption regulated by ADH • Na+ reabsorption and K+ secretion regulated by aldosterone • H+ and HCO3– reabsorption or secretion Active transport to maintain blood pH (primary or secondary) Passive transport • Urea reabsorption increased by ADH Why? Figure 25.18e Substances that are not reabsorbed • Substances that lack carry proteins along membrane – Urea – Uric acid • Substances that are not lipid soluble • Substances that are too large to pass – Creatinine Label the parts of the nephron Describe what is occurring at sections 1-6. 1. 2. 3. 4. 5. 6. Hormonal Control of Secretion • Osmolarity – number of solute particles dissolved in one liter of water Affects osmosis • Kidneys are responsible for regulating solute concentrations in the body; the concentration of urine is regulated by hormones • Four Hormones Control Kidney Function – Renin – Aldosterone – Atrial Natiuretic Peptide (ANP) – Antidiuretic hormone (ADH) Renin • Released when glomerular pressure is low • Causes blood vessels to constrict; raising blood pressure in arteries • The efferent arteriole constricts which increases glomerular pressure • Stimulates secretion of ADH and aldosterone Aldosterone • Released by adrenal glands • When secreted causes Na+ to be reabsorbed from DCT • H20 follow Na+, so both Na+ and H2O are reabsorbed • Eliminates K+ into urine • Stimuli that cause the release of aldosterone – Decreased blood volume – Decreased sodium in blood – Increased potassium in blood (heart block) If too much aldosterone is secreted: - Excessive Na+ and H20 retention (edema, hypertension - Accelerated secretion of K ions (muscle responsiveness) Lasix – (Diuretic) inhibits Na from being reabsorbed; thus water is not reabsorbed. Atrial Natiuretic Peptide (ANP) • Works against aldosterone • Released by atrial cardiac cells when blood volume and BP are too high. • Why would the atrial cells detect a change in blood volume? • When ANP is secreted: – Causes Na+ to be dumped into tubules (urine) – H2O follows sodium into urine – Capillaries in glomerulus dilate; increasing blood flow to Bowman’s capsule; increasing UO – Inhibits the secretion of renin, aldosterone and ADH – Urine contains more Na+ H2O; blood pressure and blood volume decrease ADH (Antiduretic hormone) • When ADH is secreted, water is reabsorbed from DCT and collecting tubules • Person feels thirsty • When ADH is not secreted, DCT and collecting tubules are impermeable to water, no reabsorption occurs here. Concentration of Urine is controlled by ADH • Dilute Urine – Na and other ions are removed from filtrate – Urine appears clear in color • Concentrated Urine – ADH is secreted; distal and collecting tubules reabsorb water – When water leaves filtrate; urine concentration increases Work of the Nephron with Hormone Secretion Diuretics – chemicals which increase UO • Any substance that is not reabsorbed and carrries water out of body – Alcohol – inhibits ADH – Caffeine – Increases filtration rate (GFR) • Diuretic drugs are taken for CHF, edema and to increase UO Active transport Passive transport Collecting duct Descending limb of loop of Henle DCT Cortex NaCI H2O NaCI Outer medulla NaCI H2O Urea Inner medulla (a) Absence of ADH Large volume of dilute urine Figure 25.17a Maintaining a Balance • Fluid and Electrolyte • Other Systems assist in Balance excretion and affect – Water into body = Water out kidney function of the body – Integumentary – Respiratory – Digestive – Neither a net gain or loss of electrolytes should occur in body • Acid-Base Balance – Blood pH ranges between 7.35 – 7.45 – Kidneys will secrete H+ ions when blood pH drops • Acidosis – Blood pH drops below 7.35 – Respiratory Acidosis • Due to an increase of CO2 levels in body – Metabolic Acidosis • Due to cell metabolism in the body • Lactic acid in muscle metabolism • Ketone bodies by the breakdown of fat • Diabetics don’t use glucose due to lack of insulin; so cells will break down fat instead Blood ph < 7.05 disrupts the stability of cell membrane, alters protein function (enzyme), causes heart arrhythmias and leads to coma Kidney Stones • Hardened mineral deposits that form in kidney • Symptoms – – – – – Blood in urine Increased need to go Nausea and vomiting Pain during urination Tenderness in abdomen and kidney region • Treatment – Lithotripsy – Medication Renal Failure – Kidney Failure • Nephrons in kidney stop functioning – Unable to filter or excrete waste – Can’t regulate composition of body fluids – Can’t control erythrocyte function or blood pressure – Can’t control salt balance