Group Medical Insurance
Client
ASHOKA TRUST FOR RESEARCH IN ECOLOGY AND THE
ENVIRONMENT
Contents
Group Medical Insurance
Disclaimer:
This benefit summary will serve as a guide to the benefits provided by ASHOKA TRUST FOR RESEARCH IN
ECOLOGY AND THE ENVIRONMENT. The information contained here is only a summary of the policy
documents which are kept by the company. If there is a conflict in interpretation, terms & conditions of the
policy will prevail.
Prepared by
Emedlife Insurance Broking Services Ltd
No. 862, 3rdFloor
Prabhat Arcade, 80 Ft Road
Koramangala 8th Block
Bangalore – 560 095
Tel: 080-4265000 Fax: 080-4265000
Copyright © 2012. All rights reserved. No part of this publication may be reproduced, stored in the retrieval
system, or be transmitted in any form or by any means, electronic or mechanical, photocopying, recording or
otherwise, without the prior written permission of the publishers.
Help Line Numbers
For all queries and assistance, please contact Emedlife Insurance
Praveen Raj S. (Sr. Executive - Client Services) – 90081 44417 (Email: praveenraj_s@emedlife.co.in)
Arjun (Escalation 1) – 90081 44456 (Email: arjun_k@emedlife.co.in)
Ramani (Escalation 2) - 99808 11326 (Email: ramani_hs@emedlife.co.in)
The Insurance Third Party Administrator is Medi Assist India TPA and their contact details are:
Tel: 080- 26584811
Fax: 1 800 425 9559
Toll free number: 1-800-425-9449
Email: info@mediassistindia.com
Website: https://www.mediassistindia.com
Agenda
Group Medical Insurance
TPA Service Offerings
Log in Procedure
Process for Hospitalization
Escalation Matrix
Group Medical Insurance
Broker
Emedlife Insurance Broking Services Limited
Insurer
National Insurance Company Ltd
TPA
Medi Assist India TPA Pvt Ltd
Group Health Plan
Policy Holder
ASHOKA TRUST FOR RESEARCH IN ECOLOGY AND THE ENVIRONMENT
Period of the Cover
12 months
Inception Date
21th May 2015
Expiry Date
20 th May 2016
Insurer
National Insurance Company Ltd
TPA
Medi Assist India TPA Pvt Ltd.
Sum Insured Limits
INR 2 Lacs, 3 Lacs and 4 Lacs Sum Insured per Employee.
Members Covered
Self only
Geographical Limits
India (Covers treatment in India only)
Group Mediclaim Coverages
Pre-existing Diseases covered
Waiver of Time exclusion for diseases (30 days/1 Year/2 Years/4 Years )
Maternity Benefit of INR 25,000 for Normal and 35,000 for C-Section.
Maternity benefit covered from day one.
New Born baby cover.
30 and 60 days Pre & Post hospitalization covered.
Ambulance Charges covered up to 1% of Sum Insured with maximum limit of INR
1,000/- per incidence .
Room rent (Including Nursing charges) charges payable up to 1% of Sum Insured for
normal and 2% of Sum Insured for ICU with max limit of INR 5,000 per day.
Scope of Insurance Cover
Includes:
Only “in-patient” hospitalization expenses.
Active treatment with minimum 24 hours hospitalization.
Pre-hospitalization expenses of 30 days before admission and post hospitalization expenses for 60 days
after discharge for an eligible hospitalization
Cashless facility against Pre-Authorisation at Network hospital only
Excludes:
Non - Medical Expenses - Registration/Admission fees, hospital surcharge, food bills for attendants,
telephone charges, pharmacy charges for non-medical items etc.
Other standard exclusions
Stay in hospital without undertaking any treatment or where there is no active regular treatment
Standard exclusions to the Insurance Cover
Injury or disease directly or indirectly caused by or arising from or attributable to war or war like
situations and by nuclear weapons.
Circumcision unless necessary for treatment of diseases
Congenital ailments or defects/anomalies
Hospitalization for convalescence, general debility, intentional self-injury, use of intoxicating
drugs/ alcohol.
Venereal diseases, HIV and AIDS, Infertility treatment and Naturopathy
Cost of spectacles, contact lenses, hearing aids
Any cosmetic or plastic surgery except for correction of injury
Hospitalization for diagnostic tests only even if prescribed by a medical practitioner
Voluntary termination of pregnancy during first 12 weeks (MTP)
Pre and Post Natal expenses are not covered unless admitted in Hospital/Nursing
Home for active line of treatment
Unproven or experimental treatment not approved by Indian Medical Council
Any Dental treatment or surgery except arising out of an accident, which requires
Hospitalization for treatment
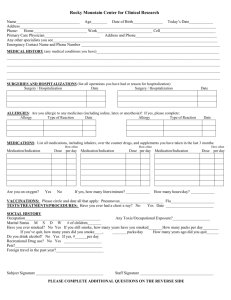
Enrollment in the program
• Existing employees are covered under the policy from 21th May 2015.
• All New joiners must enroll themselves within 20 days of joining the company.
Provide required
details of yourself to
the HR
HR sends the data to
the EMEDLIFE to
upload their system
EMEDLIFE will upload
this data and inform
ATREE on the
activation of all facility
for employees
Error in data
on E card
Send mail to
EMEDLIFE / HR with
ID Card Nos.
TPA will upload
E cards on their
Website for all
employees
Employee
verifies
details of
the E card
on TPA
website
E Card Ok
Use E card/Physical
card for cashless
hospitalization
authorization
Medi Assist India TPA Pvt Ltd – Service Offerings
•Online access to view self details, claim status and e card download
•Cashless Hospitalization
•SMS facilities for Pre-authorizations.
•24 hour telephonic Nurse line.
•Claims Administration.
Procedure for Online Access
Procedure for Online access
Please follow the below steps to Login
Log on to https//:www.mediassistindia.com .
Select “Login” option present on the top Right of the screen
Select “Corporate Employee”.
User ID:
Password:
How does the plan work ?
Hospitalization event can be:
Planned or Emergency
In a Network hospital or Out of Network
Hospitals have details of TPAs - please check with hospital helpdesk
if they accept Medi Assist Insurance card to avail cashless
hospitalization
For updated list of Network hospitals, see
http://www.mediassistindia.com
Network Hospitalization (Planned)
Fill up the Pre-Authorisation form with the help of
the treating Doctor and fax it to the Medi Assist
Nurse line with the assistance of the hospital staff 48
hours prior to Admission
Medical Management Team assesses the Preauthorisation request and after it is approved,
Medi Assist Nurse line sends Credit letter to
Network Hospital
All Medical Expenses including
Room Rent would be covered under
Cashless
Network Hospitalization (Emergency)
Call up Medi Assist Nurse line if
possible
Or else, get hospitalized into the
nearest Network Hospital with
the medical E- card/Physical card
Get the Patient treated and after the
patient has stabilized, complete the
Pre-authorisation process
You can also identify yourself as a member
of TPA so that they can assist you with the
Pre-authorisation formality.
Possibility of Denial of Cashless - examples
• Admission for investigations/ observation / evaluation only .
• Admission beyond a certain number of days apart from the normal package stay.
• Treatment not matching with disease mentioned on pre-authorisation form.
• Any treatment which otherwise could have been taken on OPD basis.
• Any congenital external disease.
• Hospital not sending proper query reply raised by TPA on time.
• Active line of treatment not mentioned in the pre-authorisation form
Non-Network Hospitalization (Planned & Emergency)
Claim Intimation has to be provided to
Emedlife/Medi Assist
Claim needs to be sent to
Emedlife within 20 days from the
Date of Discharge
Kindly make the arrangements for the
admission and pay all expenses at the
hospital
Collect all original documents from the
Hospital including the Hosp. & Doctor Registration No.
Pre & Post Hospitalization Bills
Pre Bills: 30 days prior to Date of Admission
Post Bills: 60 days after Date of Discharge
Procedure of Discharge & Claim without Cashless facility
The employee should arrange for the admission and all other payments required by the hospital.
Collect and submit to Emedlife the following documents (in original) after discharge
Discharge Card/Summary
Main pre-numbered Hospital Bill
Signed Claim Form
Pre-numbered payment Receipt
Prescriptions, reports and bills for all investigations done.
Prescriptions and bills for medicines consumed during hospitalization.
Break-up of the medicines bills amount of Rs. 200/- or more.
Sticker of lens in the case of cataract cases
GPLA certificate in maternity cases
Medico-legal certificate and FIR in accident cases
Hospital’s registration number is required and Mandatory
Claims will not be assessed if all the documents mentioned are not submitted.
• Claim Submission Timeline - All claims to be submitted to Emedlife within 20 days from date of discharge.
NOTE : Any delayed submission beyond the timeline mentioned above will not be processed. In such cases, letter
from the employee would be required with a valid reason for delay in submission. It is at the discretion of the
Insurer to provide the approval for such cases.
Claims Administration Process
•
Claims Administration Team
– Document handling
– Registration of claim with insurer
– Liaison with insurer for payment
– Explanation of paid amounts and rejection
•
Document Recovery Team (DR Team)
– Sends reminders for the missing/required document(s). In case of non-receipt of the same,
may send the entire claim back to the employee or deduct the appropriate amount and send
the balance claim for QC
•
Quality Check Team (QC Team)
– Re-assesses the claim to ensure that the claim is complete in all respect before sending it for
payment to the insurance company.
•
Claim settlement
– Approximate time to settle claim is 10 - 15 working days after receipt by TPA of complete
documentation
Some Important Do’s & Don'ts
• Submit the Reimbursement claim documents to Emedlife Helpdesk within 20 days from date of
Discharge
• Always carry photo ID proof along with your medical card.
• Photo ID proof can be: Driving license / PAN Card / Passport / Voter ID.
• For Planned hospitalization: take approval before getting admitted in hospital
• For Reimbursement cases, always collect all originals from Hospital including final bill with
break up and payment receipt.
• Any issues in getting cashless approval, please contact the Account Manager (Emedlife).
• On leaving ATREE, the Insurance card is to be returned to HR Deptt.
For any kind of clarification, please contact:
Emedlife
Medi Assist
Account Manager
Praveen Raj S.
Gajendra
Phone no
90081 44417
93425 33651
gajendra.jothimala@mediassistindia.com
Mail ID
praveenraj_s@emedlife.co.in
1st Escalation
Arjun K
Venkatakrishnan
Phone no
90081 44456
96861 95495
venkatakrishnans@mediassistindia.com
Mail ID
arjun_k@emedlife.co.in
2nd Escalation
Ramani
Phone no
99808 11326
Mail ID
ramani_hs@emedlife.co.in
THANK YOU