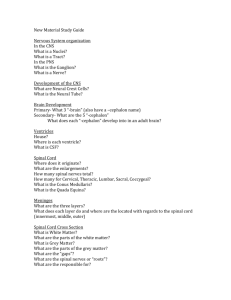
spinal cord
advertisement

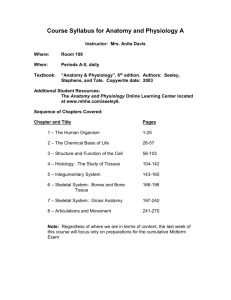
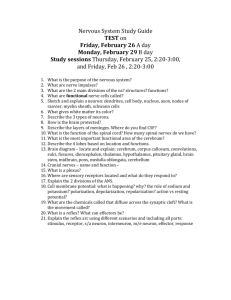
Chapter 13 The Spinal Cord & Spinal Nerves Lecture Outline Principles of Human Anatomy and Physiology, 11e 1 INTRODUCTION • The spinal cord and spinal nerves mediate reactions to environmental changes. • The spinal cord has several functions. • It processes reflexes. • It is the site for integration of EPSPs and IPSPs that arise locally or are triggered by nerve impulses from the periphery and brain. • It is a conduction pathway for sensory and motor nerve impulses. • The size of the vertebral canal varies in different regions of the vertebral column and affects spinal cord injuries. Principles of Human Anatomy and Physiology, 11e 2 Chapter 13 The Spinal Cord & Spinal Nerves • Together with brain forms the CNS • Functions – spinal cord reflexes – integration (summation of inhibitory and excitatory) nerve impulses – highway for upward and downward travel of sensory and motor information Principles of Human Anatomy and Physiology, 11e 3 SPINAL CORD ANATOMY • The spinal cord is protected by two connective tissue coverings, the meninges and vertebra, and a cushion of cerebrospinal fluid. • The vertebral column provides a bony covering of the spinal cord (Figure 13.1c). Principles of Human Anatomy and Physiology, 11e 4 Spinal Cord Protection By the vertebral column, meninges, cerebrospinal fluid, and vertebral ligaments. Principles of Human Anatomy and Physiology, 11e 5 Meninges • The meninges are three coverings that run continuously around the spinal cord and brain (Figures 13.1a, 14.4a). – The outermost layer is the dura mater. – The middle layer is the arachnoid. – The innermost meninx is the pia mater, a thin, transparent connective tissue layer that adheres to the surface of the spinal cord and brain • Denticulate ligaments are thickenings of the pia mater that suspend the spinal cord in the middle of its dural sheath. Principles of Human Anatomy and Physiology, 11e 6 Structures Covering the Spinal Cord • Vertebrae • Epidural space filled with fat • Dura mater – dense irregular CT tube • Subdural space filled with interstitial fluid • Arachnoid = spider web of collagen fibers • Subarachnoid space = CSF • Pia mater – thin layer covers BV – denticulate ligs hold in place Principles of Human Anatomy and Physiology, 11e 7 Structures Covering the Spinal Cord • Vertebrae • Epidural space filled with fat • Dura mater – dense irregular CT tube • Subdural space filled with interstitial fl • Arachnoid = spider web of collagen fibers • Subarachnoid space = CSF • Pia mater – thin layer covers BV – denticulate ligs hold in place Principles of Human Anatomy and Physiology, 11e 8 Applications • The subarachnoid space is between the arachnoid mater and pia mater and contains cerebrospinal fluid (CSF). • Inflammation of the meninges is known as meningitis. • Removal of cerebrospinal fluid from the subarachnoid space is called a spinal tap (lumbar puncture). This procedure is used to diagnose pathologies and to introduce antibiotics, contrast media, anesthetics, and chemotherapeutic drugs. Principles of Human Anatomy and Physiology, 11e 9 External Anatomy of the Spinal Cord • The spinal cord begins as a continuation of the medulla oblongata and terminates at about the second lumbar vertebra in an adult (Figure 13.2). – It contains cervical and lumbar enlargements that serve as points of origin for nerves to the extremities. • The tapered portion of the spinal cord is the conus medullaris, from which arise the filum terminale and cauda equina. Principles of Human Anatomy and Physiology, 11e 10 External Anatomy of Spinal Cord • Flattened cylinder • 16-18 Inches long & 3/4 inch diameter • In adult ends at L2 • In newborn ends at L4 • Growth of cord stops at age 5 • Cervical enlargement – upper limbs • Lumbar enlargement – lower limbs Principles of Human Anatomy and Physiology, 11e 11 Inferior End of Spinal Cord • Conus medullaris – cone-shaped end of spinal cord • Filum terminale – thread-like extension of pia mater – stabilizes spinal cord in canal • Caudae equinae (horse’s tail) – dorsal & ventral roots of lowest spinal nerves • Spinal segment – area of cord from which each pair of spinal nerves arises Principles of Human Anatomy and Physiology, 11e 12 Spinal tap or Lumbar Puncture • Technique – long needle into subarachnoid space – safe from L3 to L5 • Purpose – sampling CSF for diagnosis – injection of antibiotics, anesthetics or chemotherapy – measurement of CSF pressure Principles of Human Anatomy and Physiology, 11e 13 Spinal nerves • The 31 pairs of spinal nerves are named and numbered according to the region and level of the spinal cord from which they emerge (Figure 13.2). – 8 pairs of cervical nerves, – 12 pairs of thoracic nerves, – 5 pairs of lumbar nerves, – 5 pairs of sacral nerves, and – 1 pair of coccygeal nerves. • Spinal nerves are the paths of communication between the spinal cord and most of the body. • Roots are the two points of attachment that connect each spinal nerve to a segment of the spinal cord (Figure 13.3a). Principles of Human Anatomy and Physiology, 11e 14 Spinal Cord & Spinal Nerves • Spinal nerves begin as roots • Dorsal or posterior root is incoming sensory fibers – dorsal root ganglion (swelling) = cell bodies of sensory nerves • Ventral or anterior root is outgoing motor fibers Principles of Human Anatomy and Physiology, 11e 15 Internal Anatomy of the Spinal Cord • The anterior median fissure and the posterior median sulcus penetrate the white matter of the spinal cord and divide it into right and left sides (Figure 13.3b). • The gray matter of the spinal cord is shaped like the letter H or a butterfly and is surround by white matter. – The gray matter consists primarily of cell bodies of neurons and neuroglia and unmyelinated axons and dendrites of association and motor neurons. – The gray commissure forms the cross bar of the Hshaped gray matter. • The white matter consists of bundles of myelinated axons of motor and sensory neurons. Principles of Human Anatomy and Physiology, 11e 16 Gray Matter of the Spinal Cord • Gray matter is shaped like the letter H or a butterfly – contains neuron cell bodies, unmyelinated axons & dendrites – paired dorsal and ventral gray horns – lateral horns only present in thoracic spinal cord – gray commissure crosses the midline • Central canal is continuous with 4th ventricle of brain Principles of Human Anatomy and Physiology, 11e 17 Internal Anatomy of the Spinal Cord • Anterior to the gray commissure is the anterior white commissure, which connects the white matter of the right and left sides of the spinal cord. • The gray matter is divided into horns, which contain cell bodies of neurons. • The white matter is divided into columns. – Each column contains distinct bundles of nerve axons that have a common origin or destination and carry similar information. – These bundles are called tracts. Principles of Human Anatomy and Physiology, 11e 18 White Matter of the Spinal Cord • White matter covers gray matter • Anterior median fissure deeper than Posterior median sulcus • Anterior, Lateral and Posterior White Columns contain axons that form ascending & descending tracts Principles of Human Anatomy and Physiology, 11e 19 Principles of Human Anatomy and Physiology, 11e 20 SPINAL CORD PHYSIOLOGY • The spinal cord has two principal functions. • The white matter tracts are highways for nerve impulse conduction to and from the brain. • The gray matter receives and integrates incoming and outgoing information. Principles of Human Anatomy and Physiology, 11e 21 Sensory and Motor Tracts • Figure 13.12 shows the principal sensory and motor tracts in the spinal cord. These tracts are discussed in detail in Chapter 16 summarized in tables 16.3 and 16.4. • Sensory (ascending) tracts conduct nerve impulses toward the brain. – the lateral and anterior spinothalamic tracts and the posterior column tract. • Motor (descending) tracts conduct impulses down the cord. – Direct pathways include lateral and anterior corticospinal and corticobulbar tracts. – Indirect pathways include rubrospinal, tectospinal, and vestibulospinal tracts. Principles of Human Anatomy and Physiology, 11e 22 Tracts of the Spinal Cord • Function of tracts - highways for sensory & motor information – sensory tracts ascend – motor tracts descend • Naming of tracts – indicates position & direction of signal – example = anterior spinothalamic tract • impulses travel from spinal cord towards brain (thalamus) • found in anterior part of spinal cord Principles of Human Anatomy and Physiology, 11e 23 Location of Tracts inside Cord • Motor tracts Sensory tracts – pyramidal tract (corticospinal) ---spinothalamic tract – extrapyramidal tract ---posterior column – ---spinocerebellar Principles of Human Anatomy and Physiology, 11e 24 Function of Spinal Tracts • Spinothalamic tract – pain, temperature, deep pressure & crude touch • Posterior columns – proprioception, discriminative touch, two-point discrimination, pressure and vibration • Direct pathways (corticospinal & corticobulbar) – precise, voluntary movements • Indirect pathways (rubrospinal, vestibulospinal) – programming automatic movements, posture & muscle tone, equilibrium & coordination of visual reflexes Principles of Human Anatomy and Physiology, 11e 25 Reflexes and Reflex Arcs • The spinal cord serves as an integrating center for spinal reflexes. This occurs in the gray matter. – A reflex is a fast, predictable, automatic response to changes in the environment that helps to maintain homeostasis. – Reflexes may be spinal, cranial, somatic, or autonomic. Principles of Human Anatomy and Physiology, 11e 26 Reflex Arc • Specific nerve impulse pathway • 5 components of reflex arc – receptor – sensory neuron – integrating center – motor neuron – effector Principles of Human Anatomy and Physiology, 11e 27 Reflex Arc • A reflex arc is the simplest type of pathway; pathways are specific neuronal circuits and thus include at least one synapse. • Reflexes help to maintain homeostasis by permitting the body to make exceedingly rapid adjustments to homeostatic imbalances. • Somatic spinal reflexes include the stretch reflex, tendon reflex, flexor (withdrawal) reflex, and crossed extensor reflex; all exhibit reciprocal innervation. Principles of Human Anatomy and Physiology, 11e 28 Stretch Reflex (patellar reflex) • It operates as a feedback mechanism to control muscle length by causing muscle contraction. – Prevents injury from over stretching because muscle contracts when it is stretched • Monosynaptic,ipsilateral reflex arc • Events of stretch reflex – muscle spindle signals stretch of muscle – motor neuron activated & muscle contracts • Brain sets muscle spindle sensitivity as it sets muscle tone (degree of muscle contraction at rest) • Reciprocal innervation (polysynaptic- interneuron) – antagonistic muscles relax as part of reflex Principles of Human Anatomy and Physiology, 11e 29 Illustration of the Stretch Reflex Principles of Human Anatomy and Physiology, 11e 30 Tendon Reflex • It operates as a feedback mechanism to control muscle tension by causing muscle relaxation when muscle force becomes too extreme. • ipsilateral polysynaptic reflex • Golgi tendon organs are in tendon – activated by stretching of tendon – inhibitory neuron is stimulated (polysynaptic) – motor neuron is hyperpolarized and muscle relaxes • Both tendon & muscle are protected • Reciprocal innervation (polysynaptic) – causes contraction of ipsilateral muscle group Principles of Human Anatomy and Physiology, 11e 31 Illustration of Tendon Reflex Principles of Human Anatomy and Physiology, 11e 32 Flexor and Crossed Extensor Reflexes • The flexor (withdrawal) reflex is ipsilateral and is a protective withdrawal reflex that moves a limb to avoid pain (Figure 13.16). • This reflex results in contraction of flexor muscles to move a limb to avoid injury or pain. • • The crossed extensor reflex, which is contralateral, helps to maintain balance during the flexor reflex. • This is a balance-maintaining reflex that causes a synchronized extension of the joints of one limb and flexion of the joints in the opposite limb (Figure 13.17). Principles of Human Anatomy and Physiology, 11e 33 Flexor (withdrawal) Reflex • Step on tack (pain fibers send signal to spinal cord • Interneurons branch to different spinal cord segments • Motor fibers in several segments are activated • More than one muscle group activated to lift foot off of tack Principles of Human Anatomy and Physiology, 11e 34 Crossed Extensor Reflex • Lifting left foot requires extension of right leg to maintain one’s balance • Pain signals cross to opposite spinal cord • Contralateral extensor muscles are stimulated by interneurons to hold up the body weight • Reciprocal innervation - when extensors contract flexors relax, etc Principles of Human Anatomy and Physiology, 11e 35 Clinical Considerations • Checking a patient’s reflexes may help to detect disorders/injury • Plantar flexion reflex -- stroke the lateral margin of the sole – normal response is curling under the toes – abnormal response or response of children under 18 months is called Babinski sign (upward fanning of toes due to incomplete myelination in child) Principles of Human Anatomy and Physiology, 11e 36 SPINAL NERVES • Spinal nerves connect the CNS to sensory receptors, muscles, and glands and are part of the peripheral nervous system. – The 31 pairs of spinal nerves are named and numbered according to the region and level of the spinal cord from which they emerge (Figure 13.2). – Roots of the lower lumbar, sacral, and coccygeal nerves are not in line with their corresponding vertebrae and thus form the cauda equina (Figure 13.2). • Spinal nerves connect to the cord via an anterior and a posterior root (Figure 13.3a). Since the posterior root contains sensory axons and the anterior root contains motor axons, a spinal nerve is a mixed nerve. Principles of Human Anatomy and Physiology, 11e 37 Spinal Nerves • 31 Pairs of spinal nerves • Named & numbered by the cord level of their origin – 8 pairs of cervical nerves (C1 to C8) – 12 pairs of thoracic nerves (T1 to T12) – 5 pairs of lumbar nerves (L1 to L5) – 5 pairs of sacral nerves (S1 to S5) – 1 pair of coccygeal nerves • Mixed sensory & motor nerves Principles of Human Anatomy and Physiology, 11e 38 Connective Tissue Covering of Spinal Nerves • Spinal nerve axons are grouped within connective tissue sheathes (Figure 13.4a). – A fiber is a single axon within an endoneurium. – A fascicle is a bundle of fibers within a perineurium. – A nerve is a bundle of fascicles within an epineurium. • Numerous blood vessels are within the coverings. Principles of Human Anatomy and Physiology, 11e 39 Connective Tissue Coverings • Endoneurium = wrapping of each nerve fibers • Perineurium = surrounds group of nerve fibers forming a fascicle • Epineurium = covering of entire nerve – dura mater blends into it at intervertebral foramen Principles of Human Anatomy and Physiology, 11e 40 Endoneurium – Perineurium -- Epineurium Principles of Human Anatomy and Physiology, 11e 41 Branching of Spinal Nerve • Spinal nerves formed from dorsal & ventral roots • Spinal nerves branch into dorsal & ventral rami – dorsal rami supply skin & muscles of back – ventral rami form plexus supply anterior trunk & limbs – meningeal branches supply meninges, vertebrae & BV Principles of Human Anatomy and Physiology, 11e 42 A Nerve Plexus • Joining of ventral rami of spinal nerves to form nerve networks or plexuses • Found in neck, arm, low back & sacral regions • No plexus in thoracic region – intercostal nn. innervate intercostal spaces – T7 to T12 supply abdominal wall as well Principles of Human Anatomy and Physiology, 11e 43 Plexuses • The cervical plexus supplies the skin and muscles of the head, neck, and upper part of the shoulders; connects with some cranial nerves; and supplies the diaphragm (Figure 13.6, Exhibit 13.1). – Damage to the spinal cord above the origin of the phrenic nerves (C3-C5) causes respiratory arrest. – Breathing stops because the phrenic nerves no longer send impulses to the diaphragm. Principles of Human Anatomy and Physiology, 11e 44 Cervical Plexus • Ventral rami of spinal nerves (C1 to C5) • Supplies parts of head, neck & shoulders • Phrenic nerve (C3-C5) keeps diaphragm alive • Damage to cord above C3 causes respiratory arrest Principles of Human Anatomy and Physiology, 11e 45 Phrenic Nerve Principles of Human Anatomy and Physiology, 11e 46 Plexuses • The brachial plexus constitutes the nerve supply for the upper extremities and a number of neck and shoulder muscles (Figures 13.7a and b, Exhibit 13.2). – A number of nerve disorders may result from injury to the brachial plexus. – Erb-Duchene palsy or waiter’s tip palsy – Klumphe’s palsy – wrist drop – carpal tunnel syndrome – claw hand – winged scapula Principles of Human Anatomy and Physiology, 11e 47 Brachial Plexus • Ventral rami from C5 to T1 • Supplies shoulder & upper limb • Passes superior to 1st rib & under clavicle • Axillary n. = deltoid & teres m. • Musculocutaneous n. = elbow flexors • Radial n. = shoulder & elbow extensors • Median & ulnar nn. = flexors of wrist & hand Principles of Human Anatomy and Physiology, 11e 48 Branches off Brachial Plexus Principles of Human Anatomy and Physiology, 11e 49 Plexuses • The lumbar plexus supplies the anterolateral abdominal wall, external genitals, and part of the lower extremities (Figure 13.9a and b, Exhibit 13.3). – The largest nerve arising from the lumbar plexus is the femoral nerve. – Injury to the femoral nerve is indicated by an inability to extend the leg and by loss of sensation in the skin over the anteromedial aspect of the thigh. – Obturator nerve injury is a common complication of childbirth and results in paralysis of the adductor muscles of the leg and loss of sensation over the medial aspect of the thigh. Principles of Human Anatomy and Physiology, 11e 50 Lumbar Plexus • Ventral rami of L1 to L4 • Supplies abdominal wall, external genitals & anterior/medial thigh • Injury to femoral nerve causes inability to extend leg & loss of sensation in thigh • Injury to obturator nerve causes paralysis of thigh adductors Principles of Human Anatomy and Physiology, 11e 51 Branches of Lumbar Plexus • Notice: Femoral and Obturator nerves • Found anterior and medial to hip joint Principles of Human Anatomy and Physiology, 11e 52 Plexuses • The sacral plexus supplies the buttocks, perineum, and part of the lower extremities (Figure 13.10, Exhibit 13.4). – The largest nerve arising from the sacral plexus (and the largest nerve in the body) is the sciatic nerve. – Injury to the sciatic nerve (common peroneal portion) and its branches results in sciatica, pain that extends from the buttock down the back of the leg. – Sciatic nerve injury can occur due to a herniated (slipped) disc, dislocated hip, osteoarthritis of the lumbosacral spine, pressure from the uterus during pregnancy, or an improperly administered gluteal injection. Principles of Human Anatomy and Physiology, 11e 53 Sacral Plexus • Ventral rami of L4-L5 & S1-S4 • Anterior to the sacrum • Supplies buttocks, perineum & part of lower limb • Sciatic nerve = L4 to S3 supplies post thigh & all below knee – Peroneal nerve injury produces foot drop or numbness – Tibial nerve injury produces calcaneovalgus (loss of function on anterior leg & dorsum of foot) Principles of Human Anatomy and Physiology, 11e 54 Branches of Sacral Plexus • Notice: Sciatic nerve origins Principles of Human Anatomy and Physiology, 11e 55 Sciatic Nerve Branches • Notice: Common Peroneal nerve and Tibial nerve behind the knee • Notice: Sciatica pain extends from the buttock down the leg to the foot Principles of Human Anatomy and Physiology, 11e 56 Dermatomes • The skin over the entire body is supplied by spinal nerves that carry somatic sensory nerves impulses into the spinal cord. – All spinal nerves except C1 innervate specific, constant segments of the skin; the skin segments are called dermatomes (Figure 13.11). – Knowledge of dermatomes helps a physician to determine which segment of the spinal cord or which spinal nerve is malfunctioning. – Skin on face supplied by Cranial Nerve V Principles of Human Anatomy and Physiology, 11e 57 Dermatomes • Damaged regions of the spinal cord can be distinguished by patterns of numbness over a dermatome region • Infusing local anesthetics or cutting roots must be done over 3 adjacent spinal nerves. • Spinal cord transection – injury that severs the cord loss of sensation& motor control below the injury Principles of Human Anatomy and Physiology, 11e 58 Disorders • Neuritis – inflammation of nerves – caused by injury, vitamin deficiency or poison • Shingles – infection of peripheral nerve by chicken pox virus – causes pain, skin discoloration, line of skin blisters • Poliomyelitis – viral infection causing motor neuron death and possible death from cardiac failure or respiratory arrest Principles of Human Anatomy and Physiology, 11e 59 Clinical Correlations • Erb-Duchene palsy – waiter’s tip position – fall on shoulder • Radial nerve injury – improper deltoid injection or tight cast – wrist drop • Median nerve injury – numb palm & fingers; inability to pronate & flex fingers • Ulnar nerve injury (clawhand) – inability to adduct/abduct fingers, atrophy of interosseus • Long thoracic nerve injury (winged scapula) – paralysis of serratus anterior, can’t abduct above horizontal Principles of Human Anatomy and Physiology, 11e 60 end Principles of Human Anatomy and Physiology, 11e 61