What is a hormone?
advertisement

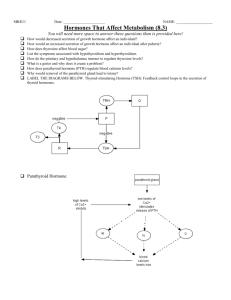
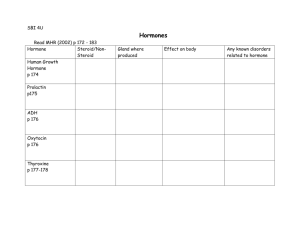
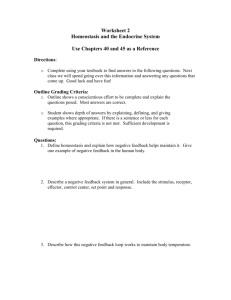
Endocrine System Huiping Wang (王会平), PhD Department of Physiology Rm C516, Block C, Research Building, School of Medicine Tel: 88208252 Email: wanghuiping@zju.edu.cn RECOMMENDED TEXTBOOK: Widmaier EP, Raff H, Strang KT (2006) Vander’s Human Physiology: The Mechanisms of Body Function, Tenth Edition. McGraw-Hill. SUPPLEMENTARY READING: Stephan Sanders (2003) Endocrine and Reproductive systems, Second Edition. Mosby. COURSE WEBSITERS: http://www.endocrineweb.com/ http://arbl.cvmbs.colostate.edu/hbooks/pathphys/endocrine/index.html http://medical.physiology.uab.edu/cardio.htm http://www.mhhe.com/biosci/ap/foxhumphys/student/olc/index.htm Endocrine System General Principles of Endocrine Physiology Hypothalamus and pituitary gland Thyroid gland Endocrine Regulation of Calcium and Phosphate Metabolism Adrenal gland Pancreatic hormones General Principles of Endocrine Physiology Outline Endocrine system and Hormone Hormone types Hormone synthesis, storage, release, transport, clearance and action modes Characteristics of hormones Regulation of Hormone Secretion Mechanisms of hormone action Endocrine System One of the two major communication systems in the body Have much longer delays Last for much greater lengths of time Integrate stimuli and responses to changes in external and internal environment crucial to coordinated functions of highly differentiated cells, tissues and organs Endocrine Glands Hypothalamus Pituitary (Anterior and Posterior) Thyroid / Parathyroid Endocrine Pancreas (islets) Adrenal Cortex and Medulla Gonad (Ovary and Testis) Endocrine gland (ductless) is a group of cells that produce and secret a hormone Endocrine System The endocrine system broadcasts its hormonal messages to target cells by secretion into blood and extracellular fluid. Like a radio broadcast, it requires a receiver to get the message - in the case of endocrine messages, cells must bear a receptor for the hormone being broadcast in order to respond. What is a hormone? Chemical messenger synthesized by specific endocrine cells in response to certain stimuli and secreted into the blood Travel via the circulation to affect one or more groups of different cells (target cells) to elicit a physiological response Hormones are primarily information transferring molecules Types of Hormones Types Amines Steroids Protein and peptides Example T4, T3, catecholamine Hormones from adrenal cortex and gonads Most of hormones insulin, oxytocin, GH Synthesis Tyrosine Cholesterol DNA – mRNA – Preprohormone Prohormone Feature lipid insoluble lipid soluble lipid insoluble Synthesis of peptide hormones NUCLEUS The DNA code is “transcribed” into mRNA. RIBOSOMES The mRNA is “translated” to give instructions for proteins synthesis. Typical synthesis of peptide hormones Preprohormones- larger hormones produced on the ribosomes of the endocrine cells Prohormones- cleavage of preprohormones by proteolytic enzymes in rER Prohormones- packaged into secretory vesicles by the Golgi apparatus Prohormones- cleaved to give active hormone and pro-fragments pre-pro-insulin pro-insulin insulin Synthesis of steroid hormones Hormone Storage and Release Thyroid and steroid hormones Not stored as secretory granules Transferring through plasma membrane Protein and catecholamine hormones Stored as secretory granules Released by exocytosis Hormones are not secreted at a uniform rate In a pulsatile pattern Diurnal (circadian) rhythm: linked to sleep-wake cycles (cortisol, growth hormone) Be aware of the pulsatile nature and rhythmic pattern of hormone secretion when relating the serum hormone measurements to normal values Hormones are not secreted at a uniform rate Rhythmic secretion Cyclic oestrogen, progesterone, LH Modes of Action Endocrine – transmission of a signal from a classic endocrine cell through bloodstream to a distant target cell e.g. testosterone Neurocrine – hormone is released from a neuron down its axon and then travels via the bloodstream to target cell Paracrine - hormone acts on adjacent cells e.g. histamine released at site of injury to constrict blood vessel walls and stop bleeding Autocrine – hormone is released and acts on the cell that secreted it. e.g. norepinephrine itself inhibits further release by that cell in the adrenal medulla A secretion may have several sites of action simultaneously Example: Norepinephrine - Autocrine action causes negative feedback on secretion. - Simultaneously, endocrine action causes respiration rate to increase, peripheral blood vessels to constrict, etc. Hormone Transport Peptides and catecholamine water soluble dissolve in blood circulate in blood mainly in free form Steroid and thyroid hormones circulate in blood mainly bound to plasma proteins the free form is biologically active the greater binding, the longer half-life Hormone Clearance The half-life of a hormone in blood is the period of time needed for its concentration to be reduced by half. Free: min Binding: mins, hrs, days Hormone concentration in blood is determined by e.g. T4 (6 days); Insulin (0.006 days) secretion rate clearance rate Ways of Clearance target cell uptake metabolic degradation urinary or biliary excretion The “metabolic fate” of a given hormone molecule in the blood Characteristics of Hormones Regulates rate of reaction Do not initiate Very specific Amplification effect Present in very small quantity pg/mL ~ g/mL Characteristics of Hormones Interaction between hormones Synergistic action Antagonistic action Permissive action Hormone A must be present for the full strength of hormone B’s effect. Up-regulation of one hormone’s receptors by another hormone the facilitation of the action of one hormone by another e.g. the ability of TH to “permit” epinephrineinduced release of fatty acids from adipose tissue cells (TH causes an no. of epinephrine receptors on the cell) Regulation of Hormone Secretion Three types of inputs to endocrine cells that stimulate or inhibit hormone secretion. Regulation of Hormone Secretion Negative feedback Most common Occurs when a hormone produces a biologic effect that, on attaining sufficient magnitude, inhibits further secretion Positive feedback Less common Amplify the initial biological effect of the hormone Negative Feedback Characteristic of control systems in which system’s response opposes the original change in the system. Hormone itself feeds back to inhibit its own synthesis. Regulated product (metabolite) feeds back to inhibit hormone synthesis. Important for homeostatic control. Example: Control of blood glucose by insulin Positive Feedback Characteristic of control systems in which an initial disturbance sets off train of events that increases the disturbance even further. Amplifies the deviation from the normal levels Example: Oxytocin (suckling) Important for amplification of level for action Mechanisms of hormone actions Hormone action mediated by the specific receptors Most hormones circulate in blood, coming into contact with essentially all cells. However, a given hormone usually affects only a limited number of cells, which are called target cells. A target cell responds to a hormone because it bears receptors for the hormone. Hormone Receptors The receptor provides link between a specific extracellular hormone and the activation of a specific signal-transduction system Structure Location Recognition domain binds hormone Coupling domain generates signal cell membrane (e.g. for insulin) cytoplasm (for steroids) nucleus (e.g. for thyroid hormone) Receptor capacity exposure to excess hormone down-regulates capacity low hormone concentration up-regulates capacity Two general mechanisms of hormone action Second messengers – enzyme activity ↑↓(rapid, cytosolic effects) Gene expression - enzymes synthesis ↑↓(slow, nuclear effects) Mechanisms of Peptide Hormone Action G proteins are GTP-binding proteins couple hormone receptors to adjacent effector molecule have intrinsic GTPase activity have three subunits: α, β, γ α subunit bound to GDP → inactive G protein α subunit bound to GTP → active G protein the effect can be either stimulatory (Gs) or inhibitory (Gi) Second messengers cAMP second message system IP3 mechanism Ca2+-calmodulin mechanism Signal transduction pathway involving adenylate cyclase Cyclic AMP signaling-sequence of events The hormone (1st messenger) binds to the membrane receptor; the membrane receptor changes shape and bind to G protein (GTP-binding protein) G protein is activated; binds to GTP (Guanosine 5’- triphosphate) and release GDP Activated G protein moves to membrane and binds and activates adenylate cyclase (GTP is hydrolysed by GTPase activity of G protein) Activated adenylate cyclase converts ATP to cAMP (second messenger) (if inhibited, no catalysed reaction by AC) cAMP is free to circulate inside the cell; triggers activation of one to several protein kinase molecules; protein kinase phosphorylates many proteins The phosphorylated proteins may either be activated or inhibited by phosphorylation Adenylyl cyclase forms cAMP, a “second messenger” that activates enzymes used in cellular responses. The phosphodiesterase enzymes “terminate” the second messenger cAMP. Amplification effect Each protein kinase can catalyse hundreds of reactions The cAMP system rapidly amplifies the response capacity of cells: here, one “first messenger” led to the formation of one million product molecules. PIP-calcium signaling mechanism This receptor-G-protein complex is linked to and activates phospholipase C, leading to an increase in IP3 and DAG, which work together to activate enzymes and to increase intracellular calcium levels. PIP-calcium signaling mechanism A hormone (first messenger) binding to its receptor causes the receptor to bind inactive G protein G protein is activated; binds GTP & releases GDP Activated G protein binds & activates a membrane-bound phospholipase enzyme; G protein becomes inactive Phospholipase splits phosphatidyl inositol biphosphate (PIP2) to diacylglycerol (DAG) & inositol triphosphate (IP3); DAG activates protein kinases on the plasma membrane; IP3 triggers calcium ion release from the ER Released calcium ions (second messengers) alter activity specific enzymes’ activity and ion channels or bind to the regulatory protein calmodulin; Calmodulin also activates specific enzymes to amplify the cellular response Ca-calmodulin system Mechanisms of steroid Hormone Action Modulation of gene expression Steroid hormones bind to intracellular receptors The steroid-receptor complex binds to DNA, turning specific genes on or off Steroid hormone receptor Sequence of events for steroid hormone binding Steroids are lipid-based and can diffuse into cells easily No need for intracellular second messenger Mobile receptors Some steroids bind to a cytoplasmic receptor, which then translocates to the nucleus Other receptors for steroids are located in the nucleus or are nuclear receptor proteins In both cases, the steroid-receptor complex formed can then bind to specific regions of DNA and activate specific genes Activated genes transcribe into messenger RNA and instruct the cell to synthesize specific enzyme proteins that change the metabolism of the target cell Radioimmunoassay (RIA) (from the Nobel lecture by Dr. Rosalyn Yalow, 1977) QUIZ The main difference between the modes of action of peptide hormones and steroid hormones is that a. peptide hormones bind to intracellular receptors whereas steroid hormones bind to receptors on the cell surface. b. peptide hormones bind to receptors in the nucleus whereas steroid hormones bind to receptors in the cytosol. c. peptide hormones bind to receptors on the cell surface whereas steroid hormones act as second messengers. d. peptide hormones bind to receptors on the cell surface whereas steroid hormones bind to intracellular receptors. e. there are no differences; both act by binding to receptors on the cell surface. QUIZ The main difference between the modes of action of peptide hormones and steroid hormones is that a. peptide hormones bind to intracellular receptors whereas steroid hormones bind to receptors on the cell surface. b. peptide hormones bind to receptors in the nucleus whereas steroid hormones bind to receptors in the cytosol. c. peptide hormones bind to receptors on the cell surface whereas steroid hormones act as second messengers. d. peptide hormones bind to receptors on the cell surface whereas steroid hormones bind to intracellular receptors. e. there are no differences; both act by binding to receptors on the cell surface. QUIZ In the absence of thyroid hormone, epinephrine stimulates release of a small amount of fatty acids from adipose cells. In the presence of thyroid hormone (which has no effect by itself), epinephrine causes a much more substantial release of fatty acids from the cells. The effect of thyroid hormone on epinephrine's actions is called a. b. c. d. e. antagonistic. agonistic. permissive. direct. paracrine. QUIZ In the absence of thyroid hormone, epinephrine stimulates release of a small amount of fatty acids from adipose cells. In the presence of thyroid hormone (which has no effect by itself), epinephrine causes a much more substantial release of fatty acids from the cells. The effect of thyroid hormone on epinephrine's actions is called a. b. c. d. e. antagonistic. agonistic. permissive. direct. paracrine. Summary Hormone Hormone types Primarily information transferring molecules Transfer information from one set of cells to another Travel via the circulation to affect one or more groups of different cells to elicit a physiological response Protein and peptides Amines Steroids Action modes of hormones Endocrine Paracrine Autocrine Neurocrine Summary Regulation of Hormone Secretion Negative feedback Positive feedback Mechanisms of hormone action Mechanisms of Peptide Hormone Action Second messenger signaling pathway cAMP second message system IP3 mechanism Ca2+-calmodulin mechanism Mechanisms of Steroid Hormone Action Modification of gene expression