Washington Association of Community & Migrant Health Centers
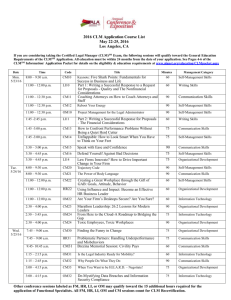
advertisement

Washington Association of Community & Migrant Health Centers PCMH Learning Community Learning Session Evolving the PCMH Care Team Presented by: Bonni Brownlee, MHA CPHQ CPEHR April 25, 2013 Advancing Healthcare Improving Health Objectives Participants will be able to: • Describe the characteristics of an effective care team • Define and roles and delegation to redistribute the work of care delivery • Define the key elements of care coordination in PCMH implementation for your organization • Define the work of care management in PCMH implementation for your organization • Take away 1 or 2 two care coordination strategies to test with your staff • Network with and steal shamelessly from other Learning Community and CHC participants 2 Challenges in Primary Care • Delivering all evidence-based guidelines for preventive and chronic disease care has been estimated to take 18 hours a day for an average sized patient panel (Yarnall et al 2009; Alexander et al 2005) • Most physicians only deliver 55% of recommended care, 42% report not having enough time with their patients (Center for Studying Health System Change 2008; Bodenheimer & Laing 2007) • Providers are spending 13% of their day in care coordination and only using their medical knowledge 50% of the time. (Gottschalk 2005; Margolis & Bodenheimer 2010) • Patient care is fragmented and patients are dissatisfied with the level of attention they receive in primary care (Bodenheimer 2008) 3 What is Team-Based Care? • A model of health care delivery that utilizes individual staff members in various roles, each functioning at their highest level according to credentials and competencies. • Shared accountability for overall patient health outcomes within a framework of clearly defined roles and responsibilities under the leadership of the Primary Care Provider. 4 What does a Patient Care Team look like? • A team is defined as a group of people working together toward a common goal. • High functioning teams demonstrate the following characteristics: – – – – – Flattened hierarchy Shared mental model Clear roles and responsibilities Effective communications Conflict resolution skills 5 Imagine a High Functioning Clinical Team • Providers assess, diagnose and treat, always doing something that requires their clinical knowledge. • Nursing role is re-established – Clinical expertise, leadership and educating becomes their focus, extending their reach • The MA/LPN role is enhanced – Using standards and training provided by providers and RN’s, they function more independently and enhance team delivery • Upward mobility strategy – Opportunities for stars to shine! 6 Engagement is the Key • Engaged team members work with passion. • Not-Engaged team members do the work expected of them, but do not put in extra effort. • Actively Disengaged team members aren’t just unhappy, but are spreading their unhappiness to other staff. 7 What makes a team successful? • Care organized through daily huddles • Brief, frequent meetings to review and plan PDSA cycles • Continuous attention to improvement eventually becomes part of the care team’s thought process, culture and daily work • Regular communication with leadership to discuss successes and barriers 8 Clinician Satisfaction with Teams NO TEAMS (work with different MAs) TEAM (work with group of MAs) TEAMLET (work with same MA) Provider Confidence in Panel Management for Cancer Screenings using Teams Source: Tom Bodenheimer 2012 9 Roles and Responsibilities 10 Who is on the Care Team? 11 The Team Identity • • • • • • Name your team – Blue team; Team A; etc Color-coded scrubs Name tags Team identification on handouts, appt cards, etc Signs and/or team photos in exam rooms Individual phone lines for each care team 12 Staffing Model To fully meet the needs of patients in the PCMH, the optimum staffing model is: 1.0 Provider 1-5 – 2.5 Support Staff (MA, CNA, LVN) 0.5 RN 3 Exam rooms 13 Use Stages of the Care Cycle to Define Team Member Roles and Responsibilities •Rooming •Exam / Assessment •Treatment Goals •Self Management Support • Scheduling • Pre-Visit Planning • Team Huddle • Nurse follow-up • Care Management • Support for care transitions • Population Mgmt / outreach Before the Visit During the Visit Inbetween Visits After the Visit • Referrals • Lab/imaging studies • Education / Support 14 Re-Evaluate Workflows Identify best practices and standardize work based on continuous quality improvement: • Flow charting processes for new workflows • Cycle Time studies – patient cycle time, provider cycle time • PDSA Cycles • Process and outcomes data by PCP/care team 15 Provider Time Study 41 min Check-in Vital Signs Med reconciliation Update PSFHRF 3 minutes MD-Patient Bonding/History/Exam/Plan 15 minutes Operationalize Decisions 5 minutes 1 minute Mini-huddle 1 minute Documentation Follow-up 6 minutes 10 minutes Modified from Kim Davis MD, MUSC 16 Impact of a Strong Support Team 22 minutes Pre-appt tests Check-in Vital Signs Med reconciliation MD-Patient Bonding/History/Exam/Plan 15 minutes Operationalize Decisions Update PSFHRF and follow standing orders Mini-huddle 1 minute Documentation 6 minutes 17 Provider Role – beyond clinical care • Will understand and work to standards of evidencebased care, review data, and receive feedback • Will understand the training protocols for support staff, will participate in evaluation of core competencies, and will become comfortable delegating tasks • Will be involved in development of workflows, offering ideas, opinions, and concerns; will have “ownership” • Will be accountable for implementation and sustainability of processes and workflows for the care team 18 RN Role The expertise and license of an RN can provide strong support to patients, providers and staff: • • • • • • • • RN Care Manager Patient educator Staff orientation and training Verification of clinical skills competencies Clinical Policy and Procedure development Triage via phone and for walk-in patients Supervises clinical support staff (if permitted by law) Committee chair (clinic operations, CQI, health education) 19 Administrative Responsibilities • Receives population management reports, reviews with Care Team / Care Manager, and conducts patient outreach • Follows up with patients who have missed important appointments • Performs Referral Management for the care team • Conducts patient check-out (prints visit summary, care plan, education, self management tools according to standards or as directed) • Is an Active participant in pre-visit planning and huddles • Develops a relationship with patients as well as the clinical team 20 The Enhanced Medical Assistant Role Team Partner, Care Coordinator, Health Coach • Allows team members to function at their highest level • Provides trusting relationships with patients, practice advice on self management when cultural background is shared • Improves job satisfaction, potential for upward mobility, and retention of excellent staff 21 California Scope of Practice - MA • Defined by Medical Practice Act (Business and Professions Code sections 2069-2071) • Performs basic administrative, clerical, and technical supportive services • May administer medication by intradermal, subcutaneous, or intramuscular injections, perform skin tests, and other technical supportive services upon the specific authorization and supervision of a licensed physician and surgeon or podiatrist. • May work from standing orders 22 MA Scope of Practice (cont’d) MAY PERFORM MAY NOT PERFORM • • • • • • • • Start IV or administer meds through IV line • Chart pupillary responses • Interpret skin tests • Independently conduct telephone triage • Inject collagen • Perform laser hair removal • Administer chemotherapy Injections Skin tests Bandaging Suture removal Ear lavage Exam preparation Shaving and disinfection of treatment sites • phlebotomy 23 Examples of Standing Orders • Lab testing – Pregnancy test, Rapid Strep, PPD placement – Random glucose (fingerstick) – In-house HbA1C • Well Child Check procedures – Hearing and vision screenings – Lead tests – Flouride varnish • Immunizations – Childhood – Flu, pneumovax • Preventive Health screenings, including depression and risk assessments • Disease management protocols (DM, HTN, asthma, etc) 24 Team Time: Optimizing the Care Team Part 1: Evaluation of Provider’s Work Activity Part 2: Redistribution of Work Activity Part 3: Identifying Barriers 25 Care Coordination and Care Management 26 Care Management - Defined • Care management programs apply systems, science, incentives, and information to improve medical practice and assist consumers and their support system to become engaged in a collaborative process designed to manage medical, social, and mental health conditions more effectively. • The goal of care management is to achieve an optimal level of wellness and improve coordination of care while providing cost effective, non-duplicative services. Center for Health Care Strategies 27 © Qualis Health 2010 4 The Evidence is Clear Team Involvement in the Care of the Chronically-Ill is the Single Most Powerful Intervention Effects of QI Strategies for Type 2 Diabetes on Glycemic Control JAMA. 2006;296:427-440. 28 Hierarchy of Care Management Support Higher Complex Case Management Chronic Illness Management Level of Support Clinic-Based Care Management Clinic-Based Care Coordination Health and Wellness Support 24-Hour Nurse Line (episodic) Lower 29 © Qualis Health 2010 5 Care Coordination An Essential Complement of Services for All Patients 30 Care Coordination Pre-Visit Planning supports the Team Huddle • Care Coordinator reviews : ⁻ ⁻ ⁻ ⁻ Lab Log to determine outstanding labs Referral Log to determine outstanding consults Health Maintenance services due Medication Reconciliation Records 31 Team Huddles Huddles enhance communication Why ? • Sets the tone for the day • Establishes competence • Disavows perfection • Predicts what will happen later When ? • Start of the day • Prior to a procedure • On the spot – as the situation changes • When joined by a new team member 32 Medication Reconciliation • • Updated at every encounter and transition of care • • New medications are added to the list • • • • No duplicates (generic vs. trade) Changes made by other providers are communicated and medication list in PCP record is updated Discontinued medications are removed from the list (or stop date documented) Herbals and supplements must be included Allergy list is up to date Ensure patient / family agrees with list! 33 Closed-Loop Test Tracking Ensures that results are received, reviewed by provider, and acted upon for every lab or imaging test ordered 34 What can be tracked – and how? • • • • • All tests ordered Which tests were scheduled Which tests were done Turn-around times Outliers Tracking tools include: • Manual log • Excel spreadsheet • Computer software 35 Communicating Test Results • Normal results • Abnormal results • Establishing a timeframe for communicating results to patients 36 Closed-Loop Referral Tracking • Types of Referrals ⁻ Internal vs external referrals ⁻ Opinion ⁻ Procedure (imaging, endoscopy) ⁻ Assume care • Ensures that the patient completed a visit and a note was received back from the specialist each time a specialty referral is ordered 37 Transitions of Care • After ED visit • After hospital admission and discharge • Coordination with other care facilities (rehab, SNF, etc.) • Transfer to new PCP • Transition from pediatric service to adult medicine 38 Why Focus on Care Transitions? • 2/3 of Medicare patients are re-hospitalized or die within one year of index hospitalization. • Half of Medicare patients are not seen in the outpatient setting within 30 days of discharge. • Care transitions are error prone • Poor care transitions have the hardest effect on the most vulnerable, causing suffering, disability and death. • Failures reflect a lethal system design flaw. • No national improvement progress since 2003. 39 Care Transitions Tasks Managing care across settings is an important care coordination effort. It requires: • Communication with other settings – Knowing when patients have been seen in the emergency department or hospital – Receiving and sending appropriate documentation between settings • Medication reconciliation and management • Availability of follow-up appointments • Knowledge of about community resources 40 GROUP DISCUSSION • Do you use huddles? • Who provides the lab and imaging tracking in your office? Who notifies patients of results? • Do you have a referral coordinator? • Who is responsible for managing care transitions? • How do these individuals interact with the Care Team? 41 Care Management An Individual Patient Focus 42 Care Management • Supplements the care of complex patients • Helps identify at-risk individuals • Utilizes evidence-based care guidelines and chronic disease management strategies • Establishes a plan of care with patient/family input, goals, assessment of progress toward goals; exploring barriers, acting to remove barriers • Coordinates services from all care givers to ensure continuity • Provides disease-specific and preventive health education • Promotes and supports self-management 43 Care Management Program Benefits • • • • Improve quality and reduce cost Reduction in acute inpatient admissions and LOS Reduction in 15 and 31 day readmissions Reduction in ED utilization and PCPs report : • Time savings of up to 30 minutes daily • Improved patient engagement • “I can do a much better job as a physician with this level of support for myself and my patients.” 44 Care Management Roles Care Coordinator / Health Coordinator • MA or LVN • Tracks tests and referrals • Facilitates communication with facilities and continuity of care at transitions • Organizes and maintains health information and registry data for population management and implementation of evidence-based guidelines • Assists in patient education and self-management support • Contributes to medication reconciliation 45 Care Management Roles Care Manager • Licensed RN or LCSW/MSW • Identifies and manages a small number of high risk/high cost or complex patients utilizing evidence-based guidelines • Works collaboratively with PCP, patient, family, and care team to develop and implement a care plan • Coordinates care with/for patient, family, and team • Provides education and self-management support • Guides Care Coordinators and Health Coaches in implementing protocols for education and self-management support • Facilitates team conferences and communication 46 Who Needs Care Management? • Consider clinically important conditions • Identify “at-risk” patients – – – – – Social or economic challenge Multiple chronic conditions High utilizers Mental/behavioral problems Other? • Allow non-providers to suggest referrals to Care Management 47 Care Management Activities • Establish plan of care – Set goals, assess progress, remove barriers • • • • Self-management support Coordinate services Provide health education Increasing patient/family activation 48 What is a Care Plan? • A collaborative tool used by: – Patients as a road map – The Care Team in goal setting, followup, issue resolution – The Provider in setting treatment goals based on evidence-based guidelines • Content should include: – Treatment Goals – Referrals (specialty and community resources) – Responsibilities of patient, medical home/care team, and specialists 49 Care Plans vs. Clinical Summaries CARE PLAN CLINICAL SUMMARY Longitudinal focus Focused on today’s visit Long-term plan for managing chronic illness Addresses today’s complaint; may or may not include chronic care issues Reviewed by Care Team in pre-visit planning Prior clinical summary may be reviewed by Care Team in pre-visit planning Reviewed with patient at every relevant visit and updated as necessary Generally not reviewed with patient during the visit PCMH 3C2, 3C3, 3C4, 4A3, 4A4, 4A5 PCMH 1C3, 3C5 50 Documenting the Care Plan • Structure – – – – Formal vs. informal What level of detail do we need? Should it be condition-specific? Whose responsibility is it? • Identify immediate needs, short term goals and ongoing needs • Set goals with patient – specific, meaningful, measurable – Determine readiness for change (confidence, importance scales) – Establish appropriate and realistic actions 51 Components of the Care Plan I want the person working with me to know: • I have challenges with : Transportation, Vision, Hearing, Mobility, ESL, other • I have issues with Diet • My religion/spirituality impacts my health care • I live : alone, partner/spouse, extended family, other • I learn best by : reading, show & tell, listening to tapes, pictures/books/video 52 Implementing the Care Plan • Develop written self-management care plan in collaboration with patient and provider • Confirm/coordinate testing and other appointments, then later follow-up with patient to ensure that test was completed and appointments kept • Discuss preventive care needs • Plan for additional teaching as needed 53 Evaluating the Care Plan • Have needs been met? Goals achieved? • Address barriers and resolve them to enable patient to receive needed care • Is the patient in the right care setting with adequate support? • Is the patient progressing? If not, – – – – why not? Reassess patient willingness to address goals Re-educate, reinforce Re-negotiate timelines and/or expectations with patient 54 Self-Management Support Self Management Support helps people to: • Understand: – Their condition and what will happen – Recommended treatments – What they can do to manage their condition / disease • Become activated, confident, and engaged in their care • Decide among treatments • Set goals • Identify their health behaviors • Adopt and/or change behaviors • Cope and overcome barriers • Develop strategies to live as fully and productively as they can • Follow-through 55 Self-Management Support is NOT… • Lecturing • Inducing fear • Finger-wagging • “You should” • Shaming • Waiting for a patient to ask 56 What is a Self-Management Goal? • Self-management goals are the specific steps and behavior changes a patient agrees to make in order to meet the treatment goal(s). • Self-Management goals can be a part of a patient’s care plan. 57 Self-Management Tasks – Examples • Self-Monitoring – Blood glucose, blood pressure, peak flow, checking feet • Recognizing red flags; managing symptoms and signs – Fatigue, pain, wheezing • • • • • Taking medication as prescribed Diet and physical activity Medical visits, lab and diagnostic tests Coping and managing emotions and stress Avoiding or quitting risky behaviors 58 Things to Consider • • • • Receptiveness of patient to learn Health literacy Language barriers Appropriateness of materials to be used – Cultural, linguistic, reading/numeracy level • • • • Family involvement (or not) Confidentiality Privacy Sensitivity 59 If you have DIABETES, here are some things you can talk about with your health care provider Choose to talk about changing any of these and add other concerns in the blank circles. Taking medications to help control blood sugar Blood glucose monitoring Physical activity Diet Taking insulin Daily foot care Depression Losing weight Smoking Adapted from Stott et al, Fam Practice, 1995 by Barbara Kondilis of the RI Chronic Care Collaborative 60 Skills to promote Patient Engagement & Self Management • Communications – Motivational Interviewing – Open-Ended Inquiries – Reflective Listening • • • • Coaching “Teach Back” Health Literacy Cultural Competency 61 Assessing Importance “How convinced are you that it is important to monitor your blood sugars?” Not at all convinced Totally convinced • “What makes you say 4?” • “What leads you to say 4 and not zero?” • “What would it take (or have to happen) to move it to a 6?” 62 Assessing Confidence “How confident are you that you can meet your goal of exercising 5 days a week? Not at all convinced Totally convinced • “What makes you say 6? • “What might help you to get to a 7 or 8?” • “What could I do to help you to feel more confident?” 63 64 Some level of Self-Management Support should occur at every Visit • Print the After Visit Summary from EHR • Offer medication refills, if needed • Use “Teach-back” to ensure patient understanding – New medications and problems – Self-management support – Follow-up plans • Review action plan (is it mutual?) • Gather patient education materials and self-monitoring tools • Schedule follow-up visits • Schedule follow-up phone call 65 66 Began Patient Follow Up Phone Calls 67 Working Together to Impact Outcomes Interventions Process Measures Clinical Outcomes 68 Extending the QI Agenda to Care Teams EXAMPLE: TEAM MEETING STRUCTURE Week 1: Well Child Outreach/Pedi-asthma Week 2: Diabetes/Depression Week 3: MA/FD: Normal PAP/Mammo RN/MD: High-Risk patient case review Week 4: Abnormal Pap/Abnormal Mammo/PSA 69 Build an Action Plan… LIST THE STEPS NECESSARY TO ADVANCE YOUR WORK IN CARE COORDINATION AND CARE MANAGEMENT PERSON RESPONSIBLE (WHO) WHEN WHERE 1. 2. 3. 4. 5. 70 Questions 71