Quality Assessment for the Medical Laboratory
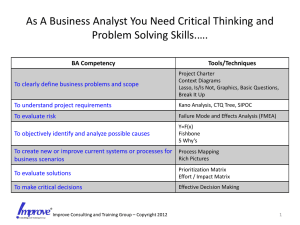
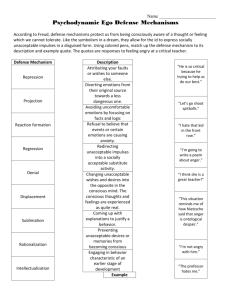
advertisement

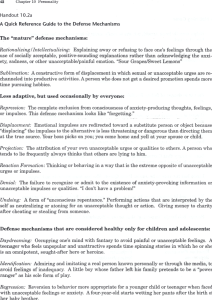
Exploring the Medical Laboratory Quality ToolBox-A Michael A Noble MD FRCPC Clinical Microbiology Proficiency Testing program Program Office for Laboratory Quality Management University of British Columbia Vancouver BC Management by the Moment Management by the Moment Management by the Moment So the better approach is… An systemic approach of organization, plan, review, and action gives you the best chance of success. The Quality Toolbox Lean What are quality tools? LEAN Six Sigma ISO 9001: 2000 A quality tool is a supplement or component part of a quality program that usually will not stand alone but can enhance the total quality system January 2009 7 Tools in the Toolbox • Mega-Tools – Lean – Six Sigma – Priority Matrices and Risk Assessment • Tools/Techniques – – – – – – Balanced Scorecards Brainstorming Control Charting Flow Charting Quality Indicators Surveys Quality Indicators are Metrics (measured process information) • Determine quality of services. • Highlight potential quality concerns, • Identify areas that need further study and investigation, and • Track changes over time. Amazon.com $30.00 A really good, inexpensive reference book Keeping Score Using the Right Metrics to Drive World Class Performance 1996 Many organizations spend thousands of hours collecting and interpreting data. However many of these hours are nothing more than wasted time because they analyze the wrong measurements, leading to inaccurate decision making. – Mark Graham Brown. Characteristics of Good Metrics Measurable objective Achievable contained Timed short and long term Engaging all levels Good Metrics Interpretable specific Balanced full cycle Actionable action oriented Seven Steps to Successful Indicators Do not start data collection until these are addressed 1. Objective 2. Methodology 3. Limits 4. Interpretation 5. Limitations 6. Presentation 7. Action plan Developing Indicators Objective What are you trying to measure? Methodology How to capture the data Limits Can I preset levels for: 1. 1. 2. 3. 4. 1. Why am I collecting this information? Be specific What data needs to be captured Who (or what) to capture the data How often to capture the data Is it achievable (time, resources, revenue)? Acceptable, Concern, Unacceptable, Critical Presentation Graphic or Text Interpretation 1. 2. 3. 4. What does it mean? Does it reflect on YOUR quality? Can I compare it? Can I trend it? Limitations 1. 2. Unintended variables What does it not mean? 1. 2. What will I do if it indicates acceptable performance? What will I do if it does not? Action Plan Developing Indicators Objective What are you trying to measure. Methodology How to capture the data Limits Can I preset levels for: 1. 1. 2. 3. 4. 1. Why am I collecting this information? Be specific What data needs to be captured Who (or what) to capture the data How often to capture the data Is it achievable (time, resources, revenue)? Acceptable, Concern, Unacceptable, Critical Presentation Graphic or Text Interpretation 1. 2. 3. 4. What does it mean? Does it reflect on YOUR quality? Can I compare it? Can I trend it? Limitations 1. 2. Unintended variables What does it not mean? 1. 2. What will I do if it indicates acceptable performance? What will I do if it does not? Action Plan Setting Relevant Limits and Ranges • • • • • • Set Objectively Validate by Study Clinical Relevancy Customer Expectation Matched Benchmarks Regulation 60 minutes Relevant or Easy? Assessing Quality Indicators • • • • Importance Scientific Acceptability Feasibility Usefulness Potential for Improvement Reliability and Validity Implementation and cost Comprehensive Having Quality Quality Indicators IQLM Indicator List 1. 2. Diabetes monitoring (system) Hyperlipidemia screening (system) • • • • • • • • • • Test Order Accuracy and Appropriateness (pre-analytic) Patient Identification (pre-analytic) Adequacy and Accuracy of Specimen Information (pre-analytic) Blood Culture Contamination (pre-analytic) Accuracy of point-of-care testing (analytic) Cervical cytology/biopsy correlation (analytic) Critical Values Reporting (post-analytic) Turnaround time (post-analytic) Clinician satisfaction (post-analytic) Clinician follow-up (post-analytic) CLMA Survey Pre-examination Phase Indicator List •Ordered test is appropriate for patient care •Patient consent appropriately collected •Test utilization by clinician for best patient care •Physician written order with every specimen •Cost/benefit assessment for laboratory test menu •Patient identification and its accuracy • Preparation of patient for specimen collection •Appropriate specimen container •Timing of specimen collection •Phlebotomy success •Specimen integrity •Specimen quantity •Specimen transportation •Accuracy of specimen identification •Condition for specimen storage CLMA Survey Examination Phase Indicator List • Quality Control • EQA-external quality assessment • Time to first result availability • Specimen contamination • Laboratory injuries or accidents • Competency of testing personnel • Vacancy of technical staff CLMA Survey Post-examination Phase Indicator List • Result reporting accuracy • Adequacy of information for interpretation of laboratory tests • Report delivery turnaround time • Consistency of critical values reporting • Result interpretation by physician • Patient’s satisfaction with laboratory services • Patient’s satisfaction specifically with phlebotomy services • Physician’s satisfaction with laboratory services Contmination Rate: Blood Culture Sets 4.0% Percent 3.0% 2.0% 1.0% 0.0% 1 2 3 4 5 6 7 8 9 10 11 12 13 14 Time Period 2002-2003 2003-2004 2004-2005 Contmination Rate: Blood Culture Sets 4.0% Percent 3.0% Objective: to ensure that blood culture results reflect sepsis. 2.0% Methodology: Count single bottle 1.0% 0.0% 1 2 3 4 5 6 7 8 9 10 11 12 13 14 positives of common skin flora/ total sets Time Period 2002-2003 2003-2004 2004-2005 Limits: Below 2% Interpretation: Meeting accepted limits all the time Limitations Definition may include some true infections and may miss others Presentation: Linear time graph Action plan: Identify and educate blood collector group. If stable for 2 years, then consider dropping from routine Quality Indicators and Timing Use an indicator only as long as it provides you with useful information. Don’t get tied to your indicators Underfill Blood Collections (As a percent of collections per site) 16.0 14.0 12.0 RF2 10.0 RF1 8.0 ER ICU 6.0 Phlebotomists 4.0 2.0 0.0 1 3 5 7 9 11 13 15 17 19 21 23 25 27 29 31 33 35 37 39 Underfill Blood Collections (As a percent of collections per site) Objective: 16.0 14.0 to ensure that blood culture are properly filled. 12.0 RF2 10.0 RF1 8.0 ER ICU 6.0 Phlebotomists Methodology: Count underfilled bottles / total bottles collected 4.0 2.0 0.0 1 3 5 7 9 11 13 15 17 19 21 23 25 27 29 31 33 35 37 39 Limits: Below 2% (?) Interpretation: Wards with inexperienced collectors have problems Limitations Some frail and elder people have very weak veins and may be impossible to collect Presentation: Linear time graph Action plan: Identify and educate blood collector group. Caution about patient outcome indicators Theoretically, outcomes best assess quality, but they are the most difficult to measure – too many confusing variables • Age, underlying conditions, therapy, circumstance – require high volumes of detailed data – need long collection periods David Hsia Medicare Quality Improvement Bad Apples or Bad Systems? JAMA. 2003;289:354-356. FACT: Quality Indicators, Done Well, Will Consume More Time Than You Have •Set Priority •Set Limits •Drop Non-Productive Activity •Target: 10-12 Computer Nonsense Metrics [urine culture] * [glucose] * [INR] X100 [NUPA hr] * [Telephone minutes] Just because a computer can calculate a value, doesn’t mean that it should. The BIG SECRET for Quality Indicator Team Engage the folks who do the work, because they know what they do! Risk management is activity directed towards assessing, mitigating (to an acceptable level) and monitoring of risks to an enterprise. Risk Management helps define PRIORITIES and helps PREVENT ERROR Tough Decisions 1 • A group of 10 laboratories over 300 square miles considers centralizing all tests to a single facility. Improved cost efficiencies Simplified process control Closer oversight Improved utilization management Improved Patient Care Reduced clinical-lab interface Extended pre-examination phase Test delays Impeded Patient care Tough Decision 2 • A laboratory considers laboratory redesign based on LEAN analysis. Improved workflow Improved time efficiencies Solve ergonomic challenges Improved cost efficiencies Improved Patient Care Expensive renovations Construction interruptions Staff retraining Equipment specificity Test menu specificity Impeded Patient care Tough Decision 3 • Laboratory considers implementing a quality management team. Better information for better decisions Better process control Continual Improvement Process Improved Patient Care Staff Reallocation Increased immediate costs Quality Commitment Impeded Patient care Tough Decision 4 • A laboratory proposes the need for an on-site level 3 (increased biosafety level) microbiology laboratory. Improved biosafety Reduced laboratory infections Faster diagnosis Improved Patient Care Construction costs Operating costs Potential Bioterror target Impeded Patient care Risk and Priority and Prevention are Relative Terms • Risk tolerance • Risk transfer PRIORITY • Risk aversion COMFORT • Risk reduction • Risk prevention • Risk avoidance ACTION Risk Management Documents for the Medical Laboratory • ISO 14971:2007 Medical devices -- Application of risk management to medical devices • ISO 20993:2006 Biological evaluation of medical devices -- Guidance on a risk-management process • ISO WD TS22367:2007 Medical laboratories -- Reduction of error through risk management and continual improvement Linking Quality and Risk Managements Introduction to ISO TS 22367 “Risk management framework has been described as being of steps, planning for risk, identifying risk and its impacts, developing risk-handling strategies, and monitoring for risk control. These steps are consistent with management requirements as described in ISO 15189:2003 including identification and control of non-conformities, establishment of preventive and corrective actions, performance of internal audit and management review and continual improvement. It is the objective of this technical report to link these in the context of the medical laboratory.” Linking Prevention and Risk ISO TS 22367 • • • • Assessment of risk of deviations from standard The quality manager should establish and maintain a process for identifying incidents associated with deviations from standards requirements, estimating and evaluating the associated risks to patient care, and controlling these risks and monitoring effectiveness of the control. The process should include a prospective risk assessment method for processes considered as high risk. Assessment of potentially high risk processes may be based upon previous audit, survey, experience, or evidence-based literature on procedures where a failure may lead to significant safety risk to patients. Linking Prevention and Risk ISO TS 22367 (Continued) – The quality manager should identify a team of people to study the selected process. Note 1: The team should have personal knowledge of the process. Note 2: The team should be comprised of people with different levels and types of knowledge. – The team should organize a thorough investigation of the process to include: a) each step of the process b) how each step of the process may fail c) how each failure at each step of the process may affect patient safety d) the rank of severity of each failure mode effect e) the most critical failure mode effects f) potential root causes of the most critical failure mode effects g) procedures to address the potential root causes. – The analysis of this Failure Mode Effects Analysis should form the basis of a Prevention Action Plan. Occurrence – Severity Grid (Qualitative) Remote Rare Common Frequent Insignificant ACCEPTABLE RISK ACCEPTABLE RISK ACCEPTABLE RISK DEBATABLE RISK Mild ACCEPTABLE RISK ACCEPTABLE RISK DEBATABLE RISK UNACCEPTABLE RISK Moderate ACCEPTABLE RISK DEBATABLE RISK DEBATABLE RISK UNACCEPTABLE RISK Severe DEBATABLE RISK UNACCEPTABLE RISK UNACCEPTABLE RISK UNACCEPTABLE RISK Occurrence – Severity Grid (Semi-Qualitative) Insignificant (0.1) Mild (0.2) Moderate (0.8) Severe (0.9) Remote (0.2) Rare (0.4) Common Frequent (0.8) (0.9) ACCEPTABLE RISK ACCEPTABLE RISK ACCEPTABLE RISK DEBATABLE RISK ACCEPTABLE RISK ACCEPTABLE RISK DEBATABLE RISK UNACCEPTABLE RISK ACCEPTABLE RISK DEBATABLE RISK DEBATABLE RISK UNACCEPTABLE RISK DEBATABLE RISK UNACCEPTABLE RISK UNACCEPTABLE RISK UNACCEPTABLE RISK Severity – Occurrence Grid • Numerical Values – Literature Benchmarks – Consensus – Experience • Regardless of source, values should be both verified, and validated to fit the FMEA being performed. HIV Testing Risk Evaluation Canadian versus American Risk Analysis Insignificant (0.1) Mild (0.2) Moderate (0.8) Severe (0.9) Remote (0.2) Rare (0.4) Common Frequent (0.8) (0.9) ACCEPTABLE RISK ACCEPTABLE RISK ACCEPTABLE RISK DEBATABLE RISK ACCEPTABLE RISK ACCEPTABLE RISK DEBATABLE RISK UNACCEPTABLE RISK ACCEPTABLE RISK DEBATABLE RISK DEBATABLE RISK UNACCEPTABLE RISK ? UNACCEPTABLE RISK UNACCEPTABLE RISK UNACCEPTABLE RISK Quality Approaches Look Alike Strategy Event Steps EXAMINE REMEDIATE AND CORRECT CONTROL IDENTIFY EXAMINE DEVELOP STRATEGY MONITOR PLAN IDENTIFY EXAMINE DEVELOP STRATEGY MONITOR DEFINE MEASURE ANALYZE IMPROVE CONTROL Corrective Action Plan PLAN MONITOR Preventive Action Plan PLAN Risk Management Six Sigma Failure Mode Effects Analysis • FMEA is a systematic method of studying failure. • 1940s 1960s 1970s 1990s US Armed Forces Aerospace (Apollo Space program) Ford Motor Company (post-Pinto) semiconductors, food service, plastics, software, and diagnostics equipment. • Documented FMEA is a REQUIREMENT in the automotive, in-vitro diagnostics, and pharmaceutical industries. October 1, 2008 FMEA: Failure Mode Effects Analysis In a process: – where are points that the process is likely to break down? – what is the probable occurrence of the different possible break-downs? – what are the likely severity and consequences of the different possible break-downs? – What is the priority list for addressing the different possible break-downs? FMEA: Failure Mode Effects Analysis • FMEA – Failure Mode Effects Analysis • FMECA – Failure Modes Effects and Criticality Analysis • FTA – Fault Tree Analysis • HACCP – Hazards Analysis and Critical Control Points • PDPC – Process Design Program Chart A Medical Laboratory FMEA Physician Requisition Sample Collection Sample Transport Sample Set-up Sample Analysis A Medical Laboratory FMEA Site Identification Good Sample Physician Requisition Sample Collection Expertise Proper Container Equipment and stains working properly Labelling Sample Transport Workload Time issues Sample Set-up Courier competent and available Proper Packaging Sample Analysis A Medical Laboratory FMEA Site Identification 0.5 Good Sample 0.8 Physician Requisition 0.5 Expertise 0.3 Proper Container 0.6 0.4 0.2 Equipment and stains working properly Sample Labelling Transport 0.9 Workload 0.5 Time issues 0.5 0.5 Sample Collection 1.5 Sample Set-up 1.9 Courier competent 0.2 and available SEVERITY Proper Packaging 0.3 Sample Analysis 1.3 A Medical Laboratory FMEA Site Identification 0.05 Good Sample 0.1 Physician Requisition 0.5 Expertise 0.05 Proper Container 0.1 0.05 0.3 Equipment and stains working properly Sample Labelling Transport 0.1 Workload 0.5 Time issues 0.5 0.8 Sample Collection 0.45 Sample Set-up 0.25 Courier competent 0.4 and available OCCURENCE Proper Packaging 0.4 Sample Analysis 1.05 Pre-Examination Grid Remote 0.2 Rare 0.5 Common 0.8 Frequent >1 Insignificant (0.2) Requisition Transport Mild (0.5) Moderate (0.8) Severe (>1) October 1, 2008 Set-up Collection Analysis A warning about FMEA • If done as a structured “top-down” exercise, many critical break points will be missed. • If done as an unstructured “bottom-up” exercise, the team will get bogged down in minutiae FMEAs should ALWAYS be: ✔Directed ✔Team Efforts ✔Planned ✔Structured The BIG SECRET for The FMEA Team Engage the folks who do the work, because they know what they do!