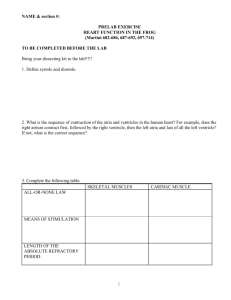
section 2
advertisement

LIU Chuan Yong 刘传勇 Institute of Physiology Medical School of SDU Tel 88381175 (lab) 88382098 (office) Email: liucy@sdu.edu.cn Website: www.physiology.sdu.edu.cn 1 Section 2 Electrophysiology of the Heart 2 CARDIAC ELECTROPHYSIOLOGY 3 Two kinds of cardiac cells 1, The working cells. Special property: contractility 4 2, Special conduction system including the Sinoatrial node, Atrioventricular node, Atrioventricular bundle (bundle of His), and Purkinje system. Special property: automaticity 5 I. Transmembrane Potentials of Myocardial Cells 6 ACTION POTENTIALS FROM DIFFERENT AREAS OF THE HEART Fast and Slow Response ATRIUM VENTRICLE 0 mv mv 0 -90mv -90mv SA NODE mv 0 -80mv 7 time ELECTROPHYSIOLOGY OF THE FAST VENTRICULAR MUSCLE +20 AMP 1 2 0 0 3 Cardiac Cell 4 -90 0 300 t (msec) 8 General description Phase 0: rapid depolarization, 1-2ms Resting potential: -90mv Action Potential +20 Phase 1: early rapid repoarization, 10 ms 1 2 Phase 2: plateau, slow repolarization, the potential is around 0 mv. 100 – 150ms 0 0 3 4 -90 0 300 t (msec) Phase 3, late rapid repolarization. 100 – 150 ms Phase 4 resting potentials 9 Ion Channels in Working Muscle Essentially same in atrial and ventricular muscle Best understood in ventricular cells 10 Ion Channels in Ventricular Cells Voltage-gated Na+ channels Inward rectifier K+ channels L-type Ca2+ channels Several Voltage-gated K+ channels 11 Cardiac + Na Channels Almost identical to nerve Na+ channels (structurally and functionally) very fast opening (as in nerve) has inactivation state (as in nerve) NOT Tetrodotoxin sensitive Expressed only in non nodal tissue Responsible for initiating and propagating the action potential in non nodal cells 12 +20 1 2 0 0 3 4 -90 0 300 t (msec) 13 Inward Rectifier (Ik1) Structure Note: No “voltage sensor” P-Region Extracellular Fluid M1 M2 membrane Inside H2N HO2C 14 Inward Rectifier Channels Current 0 Ek -120 -100 -80 -60 -40 -20 Vm (mV) 0 20 40 60 15 Inward Rectification K+ K+ Mg2+ Mg2+ K+ K+ K+ K+ -80 -30 mV mV K+ 16 Intracellular Solution Extracellular solution K+ K+ Inward Rectifier Channels Current 0 Ek -120 -100 -80 -60 -40 -20 Vm (mV) 0 20 40 60 17 Role for Inward Rectifier Expressed primarily in non nodal tissues Sets resting potential in atrial and ventricular muscle Contributes to the late phase of action potential repolarization in non nodal cells 18 +20 1 2 0 0 3 4 -90 0 300 t (msec) 19 Inactivating K channels (ITO) “Ultra-rapid” K channels (IKur) “Rapid” K channels (IKr) “Slow” K channels (IKs) Cardiac Voltagegated K Channels All structurally similar to nerve K+ channels ITO is an inactivating K+ channel- rapid repolarization to the plateau IKur functions like nerve K+ channel- fights with Ca to maintain plateau IKr, IKs structurally and functionally complex 20 Cardiac 2+ Ca Channels L-type Structurally rather similar to Na+ channels Some functional similarity to Na+ channels depolarization opens Ca2+ channels Functionally different than Na+ channels slower to open very slow, rather incomplete inactivation generates much less current flow 21 Role of Cardiac Ca2+ Channels Nodal cells initiate and propagate action potentials- SLOW Non nodal cells controls action potential duration contraction 22 Ca2+CHANNEL BLOCKERS AND THE CARDIAC CELL ACTION POTENTIAL CONTROL FORCE 30 10 DILTIAZEM 地尔硫卓 10 µMol/L 30 µMol/L 10 CONTROL 30 23 TIME Ion Channels in Atrial Cells Same as for ventricular cells Less pronounced plateau due to different balance of voltage-gated Ca2+ and K channels ATRIUM -90mv 0 mv mv 0 VENTRICLE -90mv 24 OVERVIEW OF SPECIFIC EVENTS IN THE VENTRICULAR ACTION POTENTIAL 25 Activation & Fast Inactivation 26 PHASE 0 OF THE FAST FIBER ACTION POTENTIAL Na+ Na+ m A -90mv B h -65mv m m h Na+ Na+ m C 0mv Chemical Gradient Electrical Gradient m D h +20mv h Na+ m E +30mv h 27 Ion Channels in Ventricular Muscle Ventricular muscle membrane potential (mV) Inactivating K channels (ITO) “Ultra-rapid” K channels (IKur) “Rapid” K channels (IKr) 0 Voltage-gated Na Channels “Slow” K channels (IKs) Voltage-gated Ca Channels -50 IK1 200 msec 28 Ion Channels in Ventricular Muscle Current Na Current Ca Current IK1 ITO IKur IKr IKs 29 2. Transmembrane Potential of Rhythmic Cells 30 Ion Channels in Purkinje Fibers At phase 4, the membrane potential does not maintain at a level, but depolarizes automatically – the automaticity (Phase 0 – 3) Same as for ventricular cells (Phase 4) Plus a very small amount of If (pacemaker) channels 31 Activated by negative potential (at about -60 mv during Phase 3) 32 + Not particularly selective: allows both Na and K+ The SA node cell Maximal repolarization (diastole) potential, – 70mv Low amplitude and long duration of phase 0. not so sharp as ventricle cell and Purkinje cell. No phase 1 and 2 Comparatively fast spontaneous depolarization at phase 4 A, Cardiac ventricular cell 33 B, Sinoatrial node cell SA node membrane potential (mV) SA Node Action Potential Voltage-gated Ca channels 0 Voltage-gated K channels No inward-rectifier K channels -50 If or pacemaker channels 200 msec 34 SA Node Cells Current Ca Current K currents If (pacemaker current) 35 CAUSES OF THE PACEMAKER POTENTIAL if iCa K+ iK Na+ Ca++ OUT IN 36 LOOKING AT THE PACEMAKER CURRENTS voltage iK if ionic currents iCa 37 AV node membrane potential (mV) AV Node Action Potentials 0 SA node -50 Similar to SA node Latent pacemaker Slow, Ca+2-dependent upstroke Slow conduction (delay) K+-dependent repolarization AV node 200 msec 38 Fast and slow response, rhythmic and non-rhythmic cardiac cells Fast response, non –rhythmic cells: working cells Fast response, rhythmic cells: cells in special conduction system of A-V bundle and Purkinje network. Slow response, non-rhythmic cells: cells in nodal area Slow response rhythmic cells: S-Anode, atrionodal area (AN), nodal –His (NH)cells 39 II Electrical Properties of Cardiac Cells Excitability, Conductivity and Automaticity 40 1. Excitability of Cardiac Muscle 41 (1) Refractory Period Absolute Refractory Period – regardless of the strength of a stimulus, the cell cannot be depolarized. Transmembrane Potential Relative Refractory Period – stronger than normal stimulus can induce depolarization. +25 0 -25 -50 RRP 1 2 0 3 ARP 4 -75 -100 -125 0 0.1 0.2 Time (msec) 0.3 42 Refractory Period Absolute Refractory Period (ARC): Cardiac muscle cell completely insensitive to further stimulation Relative Refractory Period (RRC): Cell exhibits reduced sensitivity to additional stimulation 43 Na+ Channel Conformations Closed Open Inactivated Outside IFM Inside IFM IFM Non-conducting conformation(s) Conducting conformation Another Non-conducting conformation (at negative potentials) (shortly after more depolarized potentials) (a while after more 44 depolarized potentials) Refractory Period The plateau phase of the cardiac cell AP increases the duration of the AP to 300 msec, The refractory period of cardiac cells is long (250 msec). compared to 1-5 msec in neurons and skeletal muscle fibers. 45 Refractory Period Long refractory period prevents tetanic contractions systole and diastole occur alternately. very important for pumping blood to arteries. 46 Comparison of refractory period and summation in cardiac and skeletal muscle fibers 47 Supranormal period: Occurs early in phase 4 and is usually accompanied by negative after-potentials as some potassium channels close. The membrane potential is about 80 mv - -90 mv, near threshold potential Absolute S.N. Rel 48 49 Skeletal Vs. Cardiac muscle contraction Impulse generation: Intrinsic in cardiac muscle, extrinsic in skeletal muscle Plateau phase: Present in cardiac muscle, absent in skeletal muscle Refractory period: long in cardiac muscle, shorter in skeletal muscle Summation: Impossible in cardiac muscle, possible in skeletal muscle 50 2) Premature excitation, premature contraction and compensatory pause 51 Extra-stimulus premature excitation premature contraction compensatory pause 52 2. Automaticity (Autorhythmicity) 53 Automaticity (Autorhythmicity) Some tissues or cells have the ability to produce spontaneous rhythmic excitation without external stimulus. Different intrinsic rhythm of rhythmic cells Purkinje fiber, 15 – 40 /min Atrioventricular node 40 – 60 /min Sinoatrial node 90 – 100 /min normal pacemaker latent pacemaker ectopic pacemaker 54 Automaticity (Autorhythmicity) The mechanism that SA node controls the hearts rhythm (acts as pacemaker) rather than the AV node and Purkinje fiber The capture effect Overdrive suppression 55 (3) Factors determining automaticity Depolarization rate of phase 4 Threshold potential The maximal repolarization potential 56 3. Conductivity 57 (1) Pathways and characteristics of conduction in heart 58 Conducting System of Heart 59 THE CONDUCTION SYSTEM OF THE HEART 60 Flow of Cardiac Electrical Activity (Action Potentials) SA node Pacing (sets heart rate) Atrial Muscle 0.4m/s AV node 0.02 m/s Delay Purkinje System 4m/s Rapid, uniform spread Ventricular Muscle 1m/s 61 characteristics of conduction in heart Delay in transmission at the A-V node (150 –200 ms) – sequence of the atrial and ventricular contraction – physiological importance Rapid transmission of impulses in the Purkinje system – synchronize contraction of entire ventricles – physiological importance 62 (2) Factors determining conductivity Anatomical factors Physiological factors 63 Anatomical factors Gap junction between working cells functional atrial and ventricular syncytium 64 65 Multi-cellular Organization = Gap Junction Channel 66 Anatomical factors Gap junction between working cells and functional atrial and ventricular syncytium Diameter of the cardiac cell – conductive resistance – conductivity 67 Physiological factors A. Slope of depolarization and amplitude of phase 0 Fast and slow response cells B. Excitability of the adjacent unexcited membrane 68 III. Neural and humoral control of the cardiac function 1. Vagus nerve and acetylcholine (Ach) Vagus nerve : release Ach from postganglionic fiber M receptor on cardiac cells K+ channel permeability increase but Ca2+ channel permeability decrease 69 ACh on Atrial Action Potential ( ) K+ Conductance (Efflux) 0 mv - 90mv Time 70 1) K+ channel permeability increase resting potential (maximal diastole potential) more negative excitability decrease 71 Ion Channels in Ventricular Muscle Ventricular muscle membrane potential (mV) Inactivating K channels (ITO) “Ultra-rapid” K channels (IKur) “Rapid” K channels (IKr) 0 Voltage-gated Na Channels “Slow” K channels (IKs) Voltage-gated Ca Channels -50 IK1 200 msec 72 2) On SA node cells, K+ channel permeability increase the depolarization velocity at phase 4 decrease + maximal diastole potential more negative automaticity decrease heart rate decrease Negative chronotropic action 73 SA node membrane potential (mV) SA Node Action Potential Voltage-gated Ca+2 channels Voltage-gated K+ channels 0 -50 If or pacemaker channels 200 msec 74 CAUSES OF THE PACEMAKER POTENTIAL if iCa K+ iK Na+ Ca++ OUT IN 75 3) Ca2+ channel permeability decrease myocardial contractility decrease negative inotropic action 76 Role of Cardiac Ca2+ Channels • Nodal cells • initiate and propagate action potentials- SLOW • Non nodal cells • controls action potential duration • contraction 77 4) Ca2+ channel permeability decrease depolarization rate of slow response cells decrease conductivity of these cell decrease negative dromotropic action 78 SA node membrane potential (mV) SA Node Action Potential Voltage-gated Ca+2 channels Voltage-gated K+ channels 0 No inward-rectifier K+ channels -50 If or pacemaker channels 200 msec 79 2. Effects of Sympathetic Nerve and catecholamine catecholamine on the Properties of Cardiac Muscle Sympathetic nerve release norepinephrine from the postganglionic endings; epinephrine and norepinephrine released from the adrenal glands binding with β1 receptor on cardiac cells increase the Ca2+ channel permeability 80 Ca2+ channel permeability increase: Increase the spontaneous depolarization rate at phase 4 automaticity of SA node cell rise heart rate increase Positive chronotropic action 81 Ca2+ channel permeability increase: Increase the depolarization rate (slope) and amplitude at phase 0 increase the conductivity of slow response cells Positive dromotropic action Increase the Ca2+ concentration in plasma during excitation myocardial contractility increase positive inotropic action 82 83 Effect of autonomic nerve activity on the heart Region affected Sympathetic Nerve Parasympathetic Nerve SA node Increased rate of diastole Decreased rate of diastole depolarization ; increased depolarization ; Decreased cardiac rate cardiac rate AV node Increase conduction rate Decreased conduction rate Atrial muscle Increase strength of contraction Decreased strength of contraction Ventricular muscle Increased strength of contraction No significant effect 84 IV The Normal Electrocardiogram (ECG) Concept: The record of potential fluctuations of myocardial fibers at the surface of the body 85 1 The Basic Mechanism 86 The Heart is a pump has electrical activity (action potentials) generates electrical current that can be measured on the skin surface (the ECG) 87 Currents and Voltages At rest, Vm is constant No current flowing Inside of cell is at constant potential Outside of cell is at constant potential A piece of cardiac muscle inside -----------------------------++++++++++++++++++ outside - + 0 mV 88 Currents and Voltages A piece of cardiac muscle During AP upstroke, Vm is NOT constant Current IS flowing Inside of cell is NOT at constant potential Outside of cell is NOT at constant potential An action potential propagating toward the positive ECG lead produces a positive signal AP inside ++++-----------------------------++++++++++++++ outside current - + Some positive potential 89 More Currents and Voltages During Repolarization A piece of cardiac muscle A piece of totally depolarized cardiac muscle inside ------------+++++++++++ inside +++++++++++++++++++ +++++++------------------outside ------------------------------outside Vm not changing No current No ECG signal current Repolarization spreading toward the positive ECG lead produces a negative response Some negative potential - + 90 The ECG Can record a reflection of cardiac electrical activity on the skin- EKG The magnitude and polarity of the signal depends on what the heart is doing electrically depolarizing repolarizing whatever the position and orientation of the recording 91 electrodes Cardiac Anatomy Superior vena cava Pulmonary veins Sinoatrial (SA)A node Atrial muscle Atrioventricular (AV) node Left atrium Mitral valve Internodal conducting tissue Tricuspid valve Ventricluar muscle Inferior vena cava Purkinje fibers Descending aorta 92 Flow of Cardiac Electrical Activity SA node Internodal conducting fibers Atrial muscle Atrial muscle AV node (slow) Purkinje fiber conducting system Ventricular muscle 93 Conduction in the Heart 0.12-0.2 s approx. 0.44 s Superior vena cava SA node Pulmonary veins SA node Atrial muscle Atria AV node Ventricle Left atrium Mitral valve Specialized conducting tissue Tricuspid valve Purkinje AV node Ventricluar muscle Inferior vena cava Purkinje fibers 94 Descending aorta 2. The Normal ECG Right Arm “Lead II” approx. 0.44 s 0.12-0.2 s QT PR Left Leg Atrial muscle depolarization R T P Q S Ventricular muscle depolarization Ventricular muscle repolarization 95 Action Potentials in the Heart 0.12-0.2 s approx. 0.44 s PR QT Superior vena cava ECG Pulmonary artery SA Atria AV Pulmonary veins Ventricle AV node SA node Left atrium Atrial muscle Mitral valve Specialized conducting tissue Tricuspid valve Purkinje Aortic artery Ventricluar muscle Inferior vena cava Interventricular septum Purkinje fibers Descending aorta 96 97 Start of ECG Cycle 98 Early P Wave 99 Later in P Wave 100 Early QRS 101 Later in QRS 102 S-T Segment 103 Early T Wave 104 Later in T-Wave 105 Back to where we started 106 3. Uses of the ECG Heart Rate Conduction in the heart Cardiac arrhythmia Direction of the cardiac vector Damage to the heart muscle Provides NO information about pumping or mechanical events in the heart. 107