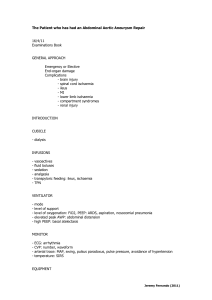
abdominal compartment syndrome
advertisement

ABDOMINAL COMPARTMENT SYNDROME CVICU Rounds Dr. Alan Sobey 1 ABDOMINAL COMPARTMENT SYNDROME • GI complications affect up to 3% of cardiac surgery cases. • Depending on the complication rate the mortality rates can be as high as 64% • Known to occur with massive resuscitation, liver transplantation, elective surgical procedures, “septic abdomens” and with severe burns 2 Abdominal Compartment Syndrome • OUTLINE – – – – – Definition History Measurements Significance Summary 3 Abdominal Compartment Syndrome • Definition: Elevated intra-abdominal pressure (IAP) – Sustained increase in the intra-abdominal pressure over normal: > 12mmHg – Multiple etiologies – NB: not the same as ACS – ACS is a late consequence of increased IAP 4 Abdominal Compartment Syndrome • Definition: Compartment Syndrome – Compartment Syndrome: • An increase in pressure within an enclosed space or cavity that causes physiologic dysfunction of its contents. • Ex: extremities following fracture or revascularization of a limb 5 Abdominal Compartment Syndrome • Definition: ACS – The adverse physiologic effects due to increased intra-abdominal pressure. – Prolonged and unrelieved pressure may lead to respiratory compromise, renal impairment, cardiac failure, shock and death. – Generally it is measured from the intracystic pressure (bladder pressure). 6 Abdominal Compartment Syndrome • HISTORY: – Fietsam et al (1989) first presented the notion of the abdominal compartment syndrome (ACS) to describe the collective effects of increased intra-abdominal pressure (IAP) on the body. – Their description was in the setting of ruptured abdominal aortic aneurysms. 7 Abdominal Compartment Syndrome • HISTORY: – Trauma literature now a major source of information. – In general, the trauma literature has recognized that end organ dysfunction occurs in the presence of a grossly distended and tense abdomen. – Open abdomen concept 8 Abdominal Compartment Syndrome • PATHOPHYSIOLOGY: – Usual intra-abdominal pressure is assumed to be near atmospheric – Sugerman et al: increased with increasing abdominal girth – Kron et al: 3 – 15 mmHg (5-7) 9 Abdominal Compartment Syndrome • PATHOPHYSIOLOGY: – As the volume in the abdomen rises so does the pressure: • the increase in pressure is in proportion to the abdominal wall compliance • Increase in pressure is in proportion to the increase in the intra-abdominal pressure. 10 Abdominal Compartment Syndrome • PATHOPHYSIOLOGY: – Corresponding decrease in hepatic / splanchnic / renal perfusion – presumably due to compression of these vascular beds. – 20% of the rise in the IAP is transmitted to the thoracic cavity: • Increase in juxtacardiac pressure. • Impaired ventricular filling. 11 Abdominal Compartment Syndrome • PATHOPHYSIOLOGY: • Increased left ventricular afterload (with decreased CO and increased PCWP) • Increased work of breathing due to decreased diaphragmatic excursion and impairment of chest wall movement. • Increased intracranial pressure (significant in the head injured trauma patient) 12 Abdominal Compartment Syndrome • CONSEQUENCES: SUMMARY • Decreased cardiac output • Increased work of • Elevated RAP and PCWP breathing • Reduced hepatic perfusion • Elevated airway pressures • Lactic acidosis during mechanical • Splanchnic hypoperfusion ventilation • Raised ICP • Abnormal V/Q matching • Peripheral edema with with hypoxemia tendency to thrombosis 13 Abdominal Compartment Syndrome • ETIOLOGY • Intra-peritoneal or retroperitoneal hemorrhage • Ascites • Bowel obstruction • Post-op edema • Pneumoperitoneum • Laparoscopy 14 Acidosis Hyperthermia transfusion Coagulopathy Sepsis: intra or extra abd Bacteremia pancreatitis Liver dysfunction Mechanical ventilation Pneumonia Abdominal Massive surgery (DCL) resuscitation Gastric or colon dist’n Hemoperitoneum Burns and trauma BMI Abdominal tumors Prone ventilation 15 Abdominal Compartment Syndrome • INDEX OF SUSPICION: Setting – – – – – – – – Ascites Bowel distention: mech obstruction/ileus Bowel edema: resuscitation or ischaemia Retroperitoneal hematoma Hemoperitoneum Coagulopathy Trauma Abdominal packing after damage control surgery 16 Abdominal Compartment Syndrome • DIAGNOSIS: Index of suspicion – When any signs of intra-abdominal hypertension are present: • • • • • • Abdominal distention Refractory oliguria Hypercarbia Refractory hypoxemia Increasing PIPs Refractory hypotension 17 Abdominal Compartment Syndrome • DIAGNOSIS: Measuring the pressure – Insert a Foley catheter and clamp the tube distal to the sample port – Instill 5-1000mL of saline into the bladder so as to leave a continuous column of fluid from the bladder to the sample port on the Foley – Insert a 18g catheter into the sample port and connect to a CVP transducer – Level the transducer at the symphysis pubis Fusco et al J Trauma 2001 18 Abdominal Compartment Syndrome • Measurement: WSACS – – – – Cmpletely supine Relaxed abdominal wall mid-axillary line 25 mL saline into the bladder 19 20 21 Abdominal Compartment Syndrome • DIAGNOSIS; – Most papers suggest several measurements during a 24 hr period: every 4 hrs – Repeat measurements are indicated by the clinical appearance of the abdomen and on the clinical situation (index of suspicion) 22 Abdominal Compartment Syndrome • INTERPRETATION: NORMAL IAP – – – – – 3-15 mmHg Obesity: higher (8 vs. 5 mmHg) Age: no definite trend Surgery: no definite trend Comorbidities: trend to higher IAP with more concurrent illnesses Sanchez et al Am Surg Mar 2001 23 Abdominal Compartment Syndrome • INTERPRETATION: – As the pressure rises over 20cm water there will be some evidence of hypoperfusion – Most will accept surgical decompression if the intraabdominal pressure is over 35 cm. – More recent authors are advocating surgical decompression for IAP of 20-25 mmHg (Cheatham et al) – WSACS: 20mmHg for treatment 24 Abdominal Compartment Syndrome • INTERPRETATION: evidence – Decreased ACS with earlier decompression – Decreased mortality with earlier decompression: ? – More pronounced benefit with increasing age 25 26 Abdominal Compartment Syndrome • Management: – Medical: • • • • • • • Maintain APP (>60mmHg) Sedation / Analgesia NMB Supine positioning NG / Colonic decompression Fluid resuscitation diuretics 27 Abdominal Compartment Syndrome • Surgical: – Percutaneous tube drainage – Abdominal decompression (DCL) 28 Abdominal Compartment Syndrome • TREATMENT: SURGICAL DECOMPRESSION / DAMAGE CONTROL LAPAROTOMY – Surgical decompression involves opening the abdominal wound and packing the wound open or closing it with a plastic dressing (Bogata Bag) – Delayed closure can be done once the edema / bleeding has resolved – Ascites can be drained percutaneously 29 Abdominal Compartment Syndrome • DAMAGE CONTOL LAPAROTOMY: – – – – Stone et al (1982) Penetrating injuries to the abdomen Avoid hypothermia / acidosis / coagulopathy Involves: • Rapid control of bleeding and contamination • Abdominal packing instead of involved procedures • Skin closure only or plastic tent closure (3 L peritoneal / CVVHDF bag) 30 Abdominal Compartment Syndrome • DAMAGE CONTROL LAPAROTOMY – Offner et al (Arch Surg) • Denver Colo • Penetrating and blunt traumas • ACS: – Long hospital stay – Increased multisystem organ failure – Increased ARDS 31 Abdominal Compartment Syndrome • Offner et al – Technique of closure and ARDS/MSOF and ACS ACS MSOF/ARDS Primary closure 80% 90% Skin 24% 36% Bogota bag 18% 47% 32 Abdominal Compartment Syndrome • SUMMARY: – IAP – measureable / preventable / treatable – ACS – end organ dysfunction from untreated or undertreated elevated IAP – Measurement: simple technique with an 18 g needle through the Foley port and a CVP transducer – Damage control – the standard for avoiding or treating elevated IAP or ACS 33 Abdominal Compartment Syndrome • Deompressive laparotomy: Effects • Most studies show a significant decrease in the IAP • IAH persists in the majority of patients (De Waele et al) • MR remained high at 35% • Overall benefit for oxygenation (PaO2/FiO2) and increased urine output 34 Abdominal Compartment Syndrome • Decompressive Laparotomy: Effects • The wound: – Messy – Open - risks for colonization or secondary infection – Delayed closure: how? 35 36 37 Abdominal Compartment Syndrome • Decreased renal output: – Harman et al – Dogs – Increased the intra-abdominal pressure to 40mmHg leading to decreased urine output and cardiac output – Resuscitated the dogs to normal CO yet the renal function remained impaired until the abdomen was decompressed 38 Abdominal Compartment Syndrome • INTRACRANIAL PRESSURE: – Increased 1. Due to increased intrathoracic pressure from the elevated diaphragms 2. Due to decreased cardiac output – Thus, increases cerebral hypoperfusion and worsens brain injury Citero et al CCM 39 Abdominal Compartment Syndrome • Definitions: – IAH: intra-abdominal hypertension • Sustained increase in IAP of 12 mmHg or more over 3 recordings separated by 4hrs each – ACS: abdominal compartment syndrome • Sustained increase in IAP of 20mmHg or more • Single or multiple organ system failure that was not previously present 40 Abdominal Compartment Syndrome • Classification: – Primary: • Due to injury or disease in the abdomen or pelvis • Frequently requires surgery or radiological treatment • Ex: trauma or the septic abdomen 41 Abdominal Compartment Syndrome – Secondary: • ACS due to conditions arising outside of the abdomen • Associated with severe capillary leak requiring resuscitation • Ex: sepsis, burns, retroperitoneal hematoma 42 Abdominal Compartment Syndrome • Recurrent ACS: – Occurs following either prophylactic decompression or therapeutic surgical decompression of either primary or secondary ACS – Ex: temporary closure device is too tight, inadequate fascial opening, recurrs after the fascia was closed. 43 Abdominal Compartment Syndrome • • • • APP: abdominal perfusion pressure APP = MAP - IAP “magic number”: 50-60 Corresponds to the perfusion gradient across the intra-abdominal visera • Evidence???? 44 Abdominal Compartment Syndrome • Diagnosis: Clinical Suspicion • Presentation / Suspect with: – Abdominal distention – Oliguria – Increased ventilatory support 45