respiratory drugs
advertisement

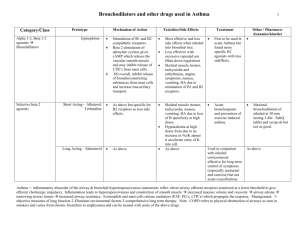
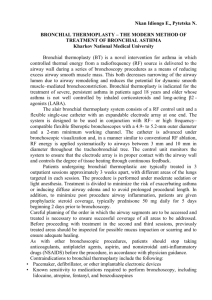
Bronchial Asthma • A disease of the airways that is characterized by hyperresponsiveness of the tracheobronchial tree to a multiplicity of stimuli • Manifested physiologically by a widespread narrowing of the air passages and clinically by paroxysm of dyspnea, cough, and wheezes Pathogenesis A. Exposure to allergen synthesis of IgE binds to mast cells in the airway mucosa Re-exposure to allergen/antigen Ag-Ab interaction on the surface of the mast cell triggers: 1) release of mediators of anaphylaxis: histamine, tryptase, PGD2, leukotriene C4, PAF provoke contraction of the airway smooth muscle 2) Synthesis and release of other mediators or a variety of cytokines: interleukines 4 & 5, granulocyte-macrophage colony stimulating factor, tumor necrosis factor, tissue growth factor from T cells and mast cells attract and activate eosinophils & neutrophils eosinophil cationic proteins, MBP, protease, PAF edema mucus hypersecretion, increase in bronchial reactivity, smooth muscle contraction B. Inhaled irritants afferent pathways in the vagus nerves travel to the CNS efferent pathways from the CNS travel to efferent ganglia postganglionic fibers release acetylcholine binds to muscarinic receptors on airway smooth muscle broncho-constriction C. inhaled materials stimulate afferent receptors to initiate reflex bronchoconstiction or release of tachynins (substance P) directly stimulate smooth muscle contraction Basic Pharmacology I. - Bronchodilators 1. Sympathomimetic Agents Directly relax airway smooth muscle by stimulating adenyl cyclase and increase the formation of cAMP in the airway tissues that results in bronchodilatation - Inhibit release of some bronchoconstricting substances from the mast cells - Increase mucociliary transport a. Beta-2 Selective Agonists - With large substitution on the amino group & in position of the hydroxyl group on the aromatic ring - Given orally, by inhalation and parenterally - For short-acting: (terbutaline, albuterol, metaproterenol, bitolterol, pirbuterol) - bronchodilation maximal in 30 minutes lasting to 4 hours - For long acting:(salmeterol, bambuterol, formeterol) - 12 hours or more - SE: skeletal muscle, tremor, nervousness and weakness b. Non-selective Beta-Agonists: - epinephrine, ephedrine, isoproterenol 2. Methylxanthine drugs a. caffeine b. theophylline c. theobromide • Mechanism of action - inhibit the enzyme phosphodiesterase hydrolyses cyclic nucleotide result in high concentration of IC cAMP smooth muscle relaxation - inhibition of cell surface receptors for adenosine - anti-inflammatory effect : inhibit the late response of antigenic challenge Pharmacodynamics • CNS : mild cortical arousal w/ increased alertness & deferral of fatigue - nervousness; insomnia - in high doses: medullary stimulation and convulsions - primary SE: nervousness and tremor • CVS: have positive inotropic and chronotropic effects - arrhythmia - sinus tachycardia and increased cardiac output - rises the PVR and BP slightly - decrease blood viscosity and may improve blood flow – pentoxifylline • GIT: stimulate secretion of gastric acid and digestive enzymes • Kidneys: weak diuretics • Skeletal muscles: have potent effects in improving contractility and in reversing fatigue of diaphragm in patient with COPD • Smooth muscle: inhibit antigen-induced release of histamine from lung tissue Pharmacokinetics - Well absorbed from the GIT Metabolized in the liver Usual dose: 3-4mg/kg every 6 hours SE: 15mg/L : anorexia, N/V, abdominal discomfort, headache and anxiety 40mg/L: seizures or arrhythmia Anti-Muscarinic Agent • Competitively inhibits the effect of acetylcholine at muscarinic receptors effectively block the contraction of the airway smooth muscle and increase in secretion of mucus • Ipratropium bromide – a quarternary ammonium derivative of atropine • Delivered by inhalation • Slightly less effective than beta agonist • Effective in COPD II. Anti-inflammatory Agents 1. - - Corticosteroids Improving all indices of asthma: severity of symptoms, tests of airway caliber, bronchial reactivity, frequency of exacerbation and quality of life Inhibit production of inflammatory cytokines Reduce bronchial reactivity Increase airway caliber SE: oral candidiasis Preparations: a. oral: prednisone b. IV: methylprednisolone c. aerosol: beclomethasone, flunisolide, budesonide, triamcinolone, fluticasone, mometasone 2. Cromolyn Sodium & Nedocromil - Prevent mast cell degranulation - Taken prophylactically - Used as aerosol - Effectively inhibit both antigen-and exerciseinduced asthma - Also useful in reducing symptoms of allergic rhinoconjunctivitis - SE: throat irritation, cough, mouth dryness, chest tightness and wheezing, reversible dermatitis, myositis, gastroenteritis, pulmonary infiltration with eosinophils and anaphylaxis III. Leukotriene Antagonists • Block the action of leukotrienes by : - inhibition of 5-lipoxygenase, thereby preventing leukotriene synthesis - inhibition of the binding of leukotriene D4 to its receptor on target tissues, thereby preventing its action • Drug categories a. Zileuton – a 5-lipoxygenase inhibitor - 600 mg QID - may cause hepatotoxicity b. Zafirlukast – 20mg BID Montelukast – 10mg OD - are LTD4 antagonist • Taken orally • Have demonstrated an important role fro leukotrienes in aspirin-induced asthma • Their effect on symptoms, airway caliber, bronchial reactivity and airway inflammation are less marked than the effects of inhaled corticosteroids, but they are almost equally effective in reducing the frequency of exacerbations Other Drugs in the Treatment of Asthma 1. Anti-IgE Antibodies - drugs that reduce the amount of IgE to mast cells - inhibits synthesis of IgE by B-lymphocytes - Omalizunab (anti-IgE Mab) 2. Calcium channel Blockers - inhibit airway narrowing induced by variety of stimuli 3. Nitric Oxide Donors - relaxation of smooth muscle and vasculature - very lipophilic drug, can be inhaled as a gas - more useful in pulmonary hypertension Possible Future Therapies • Monoclonal antibodies directed against cytokines • Antagonist of cell adhesion molecules • Protease inhibitors • Immunomodulators Other Respiratory Agents A. Mucolytic Agents 1. Acetylcysteine (mucomyst) - reduce the thickness and stickiness of purulent and non-purulent pulmonary secretions - antidote for paracetamol poisoning 2. Carbocysteine (SCMC) - act by regulating and normalizing the viscosity of secretion from the mucus cell of respiratory tract - decrease the size and number of mucus producing cells 3. Bromhexine - depolymerization of mucopolysaccharides, direct effect on bronchial glands - liberation of lysosomal enzymes producing cells which digest mucopolysaccharide fibers B. Mucokinetic & Secretolytic - increase respiratory tract secretions - enhance pulmonary surfactant production - stimulates cilia activity C. Expectorant 1. Vagal stimulants: glyceryl guiacolate, salt solution 2. Direct stimulants: KISS, bromhexine, SCMC, ambroxol D. Antitussives 1. Narcotic antitussives: heroin, codeine, morphine 2. Non-narcotic antitussive: Dextromethorphan