Auckland DHB audit summary
advertisement

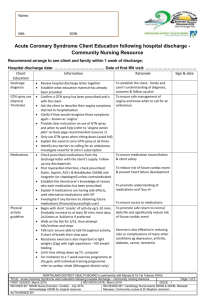
Auckland District Health Board Current Status: 29 April 2014 The following summary has been accepted by the Ministry of Health as being an accurate reflection of the Certification Audit conducted against the Health and Disability Services Standards (NZS8134.1:2008; NZS8134.2:2008 and NZS8134.3:2008) on the audit date(s) specified. General overview Auckland District Health Board (ADHB) is responsible for providing health services to the 450,000 people living in its district, along with tertiary services to the greater Auckland and Northland region and a range of national services to New Zealanders. Approximately 50% of the patients using ADHB services come from other district health boards (DHBs). ADHB provides adult medical, cancer and blood, adult community and long term conditions, cardiology, surgical, perioperative, women's health, children's health, mental health and clinical support services. The mental health service was not included in this audit. Audit Results as at 29 April2014 Consumer Rights The Health and Disability Commissioner’s Code of Health and Disability Services Consumers’ Rights (the Code) is displayed throughout the organisation in English and Te Reo Maori on posters. There are multiple languages brochures available containing rights information and how to access advocacy services. Patients are informed of their rights, to ask questions, give informed consent and make a complaint and opportunity to provide feedback on the quality of service through the ADHB website forum. Staff have education on informed consent, advocacy, the complaints process, privacy and confidentiality and spoke of how they incorporate the Code into every day practice. Privacy is protected and care is provided in a manner which is responsive to, and respectful of, the cultural and spiritual needs of patients and their families. Patients and their families are not subjected to discrimination. Patients spoken with stated their rights are upheld, staff give respectful service and they are made aware of the Code and advocacy support. They stated that they have good communication with staff throughout the patient’s hospital stay. Paediatric and maternity patients are supported to have an advocate present. Of note is the new initiative to support partners to stay overnight in the Tamaki Ward. Links with families and communities are supported. In the medical services area, family involvement is welcomed where this is desired by the patient and, at multidisciplinary meetings. Improvement is required to ensure patients are provided with information and opportunities for discussion about any resuscitation decisions. Patients’ carers in the paediatric wards report that their consent is gained where this is appropriate to do so, although verbal consent is not always recorded, and this also requires some improvement. There is a complaints management process that meets the requirements of the standard. This is known to staff in the clinical areas. There is a complaints data base managed by the consumer liaison team leader. This records the timeframes and the actions taken against each complaint. Complaints are reported through to each of the service directorates on a monthly and quarterly basis. If areas of concern or negative trends are identified these are also reported to the quality manager. Organisational Management ADHB has a vision of ‘healthy communities, quality care’, and has articulated the direction and goals for the Annual Plan. ADHB is one of four DHBs in the Northern region which have a range of shared activities, including a Northern Regional Health Plan - 2012, which describes how the DHBs can work together to meet future demand. ADHB also works closely with Waitemata DHB including having two shared executive level roles focussed on the achievement of improved health outcomes and the funding allocation to achieve this goal. During 2014 ADHB is embarking on an extensive strategic planning process to refresh the vision, mission and values and strategic goals. This process will include involvement of the wider community, service users and staff. In 2013 ADHB underwent a senior management restructure with the provider directorates now having a ‘single point of accountability’. A clinical director works in partnership with senior clinical leaders supported by management, patient effectiveness and human resource team members. The management operating system is becoming well embedded and is leading to tangible improvements in service quality and productivity. The DHB uses the Annual Plan as the quality and risk plan with a focus on the patient experience. A commitment to this is seen through the on-line patient experience survey introduced in 2012. This survey has a database of over 12,000 responses providing a wealth of information to guide quality improvement activity. There is an established structure and system for the management of quality and risk which includes reporting to the senior management team, the Clinical Board and the Hospital Advisory Committee. ADHB is a signatory to the ‘Open for better care programme’ of the Health Quality & Safety Commission (HQSC) and is monitoring priority areas such as falls prevention, medications management, hand hygiene, surgical safety, hospital acquired infections and pressure injuries. Adherence to the document control system, and ensuring policies and procedures are current are areas requiring improvement as is having sufficient resource available to facilitate the timely response to adverse event investigation, monitoring and resolution. Staffing levels are adequate for the clinical professions and the ‘releasing time to care’ programme is resulting in an increase in nursing direct patient contact time. The implementation of an acuity system has been accepted as a priority plans are well underway for rollout commencing during 2014. The human resources system handles approximately 10,000 staff with a turnover of less than 10%. There is excellent service specific orientation to the different specialties. Medical staff credentialing is up to date. Areas requiring improvement relate to the system for management of the personnel files, and for monitoring completion of induction, staff training and annual performance appraisals. Patient records are scanned into an electronic record within 48 hours of discharge making information available, however improvement is needed with the management of the hardcopy file during the inpatient period to support ready access to information, to ensure no loose pages are lost from the file and to protect privacy. Continuum of Service Delivery Assessment commences in the emergency department (adult or child) or the adult assessment and planning unit (APU) using a structured assessment format which follows the patient through to discharge. A variety of assessment tools are available for use which are designed to identify the needs of the patient and inform the plan of care. Assessment continues throughout the admission. Areas requiring improvement have been identified for midwifery assessment, and the utilisation and completion of assessment templates within the child and women’s health service. Care planning is individualised and well documented with some inpatient areas utilising care pathways. Care needs are communicated through shift handover processes and documented in progress notes. There is timely access to all services and it is demonstrated that planned interventions are implemented and are linked to the assessment processes, and referrals are actioned. Multidisciplinary teams contribute to the planning and coordination of care, with improvement required in the paediatric service. Patients and family members report that staff discuss care planning and goals with them, however improvements are required in relation to the documentation of individualised patient’s goals. Ongoing evaluation of patient responses to the care provided occurs and is documented in the progress notes by all members of the health care team, at least every eight hours, and is of a high standard in most instances. An ‘early warning score’ is being used to identify if the patient’s condition changes and this is communicated in a timely manner and changes to care are efficiently and promptly implemented. Improvements are required with the completion of the paediatric early warning score, the monitoring of individual patient’s fluid intake and the completion of the surgical safety checklist. Discharge planning commences early in the hospital stay, with timely referrals made as required. Discharge from inpatient services occurs when all aspects of the discharge plan are in place and there is a team view that the patient is adequately prepared for discharge. Patients and family members report being actively involved in their discharge planning. Discharge documentation is available to support the planning process and is generally well documented, however an area for improvement has been identified within the child and women’s service. Medication management is guided by policies, procedures and guidelines which are seen to be in line with good practice and known to staff through orientation to their area of work. Two medication safety committees (children and adult) oversee the medication processes including managing medication reconciliation. A number of areas are identified as requiring improvement related to medication management and documentation. Examples are prescribing practices, safe pro re nata (PRN) prescribing and management of when patients bring their own controlled drug into hospital. The food services have undertaken Hazard Analysis and Critical Control Point (HACCP) with few recommendations. The menu is on a two week cycle with multiple variations (200), these are overseen by dietitians. Special diets and requirements are managed by service dietitians and processes are in place to inform the kitchen staff. Safe and Appropriate Environment All buildings have a current building warrant of fitness. Seismic status for all the buildings is known with some buildings closed pending strengthening. There is an effective maintenance information system with staff spoken with stating that response to maintenance requests is good. Areas requiring improvement include some of the carpet and seating in public areas; and shower wall panelling that needs repair in certain clinical areas. Biomedical equipment records indicate a high degree of compliance with monitoring. The high risk life support equipment monitoring is an area for improvement as is the monitoring of hot water temperature at the patient point of contact. Auckland DHB (ADHB) has policies on waste management systems that are comprehensive and include personal protective equipment (PPE). An external contracted company manages waste. The availability of PPE in the maternity and paediatric areas needs improvement. A tour of the facility to review compliance with environmental standards identified areas requiring improvement related to hand washing facilities on one dock way, storage of chemicals in a few areas, medical and cytotoxic waste storage and HAZCHEM signage for the underground diesel tank is missing. The cleaning service for all buildings is now in-house and satisfaction with the new arrangements is reported by clinical area staff. The laundry service is provided off site by an external contracted company. Audit of the provider occurs on an annual basis with no issues raised by staff in the clinical areas. ADHB has comprehensive emergency and incident management systems in place including plan documents that specify roles and responsibilities and readily available flip charts for rapid response guidance. Current fire evacuation approval and six monthly fire drills evident. Security systems include restricting entrance points at night and responses to breaches of security or aggressive behaviour. The security system in the maternity service requires improvement. Restraint Minimisation and Safe Practice A restraint minimisation group meets quarterly and receives reports on restraint and enabler use. There is no consumer member on the committee and this is being looked at. Audits occur monthly with results analysed and trends identified by the clinical effectiveness co-ordinator for review by the committee. The restraint minimisation policy is under review. Following incidents where patients fell over the bedrails while in use as a restraint or enabler a project has been undertaken to review all aspects of bedrail use. This has resulted in an improved decision making process to both identify if bedrails are the most appropriate way to manage the patient’s risks and to monitor their safe use. The generic forms pertaining to restraint are on the intranet. These capture the assessment, review and monitoring of restraint use. Neuroservices have documentation specific to the patient needs in their service. Three patient’s charts, where restraint has been used are reviewed, two in the neuroservices area and one in a medical ward. It is identified that the forms do not fully meet the requirements of the standard and the documentation for the patient in the medical ward lacks detail in assessment and evaluation. These are areas for improvement. Infection Prevention and Control There are mature infection prevention and control processes in place and evidence that these are imbedded within the organisation. Responsibilities are defined with clear lines of accountability to senior management. A team of well qualified infection prevention and control practitioners lead a programme developed and signed off by the Infection Prevention and Control Committee. Education of staff is planned to meet the needs of the organisation and this is completed at orientation, on an ongoing basis, such as the hand hygiene work, and online education is also available. There are a number of projects underway, and one looking at a new process for the management of multidrug resistant organism – extended spectrum beta lactamase (ESBL) patients - is in the pilot project phase and this is tracked as a systems tracer as part of the audit process. There is evidence of education and planning of the process and follow up management by the infection control co-ordinator for the area. Surveillance is undertaken and reported nationally, regionally and in-house. Antimicrobial stewardship is undertaken and monitored.