Bonus Document Fall 2015 Exam 2 OMSII
advertisement

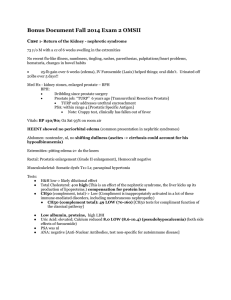
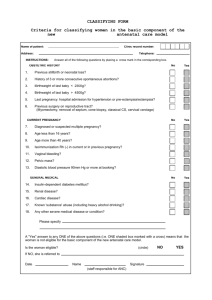
Bonus Document Fall 2015 Exam 2 OMSII A past bonus for this 2nd exam once asked: What would a microscopic analysis of urine with very high cholesterol and no other abnormalities (no proteinuria, etc) look like? Student Resources 2016 and 2017 both feel that this is a “bitch question” we haven’t been able to find literature to support that there would be any classic finding. So we would assume their UA should be normal. However, a standard work up should be run on their urine to look for glucose or evidence of renal damage from co-morbidities. If you find “fatty casts” in the urine, are pathognomonic for Nephrotic syndrome. Additionally, Hyperlipidemia may be found in these patients as the liver will spit out lipids in an attempt to maintain some osmotic balance in the blood. Case 1- Alex Noles Case No 124 --Return of the Kidney - nephrotic syndrome 73 y/o M with a cc of 6 weeks swelling in the extremities- hospitalized – found proteinuria ● 25-lb gain over 6 weeks (edema), IV Furosemide (Lasix) helped things; oral didn't. Urinated off 20lbs over 5 days!! Med Hx - kidney stones, enlarged prostate – BPH BPH: ● Dribbling since prostate surgery ● Prostate job: “TURP” 6 years ago [Transurethral Resection Prostate] ● TURP only addresses urethral encroachment PSA: within range 4 [Prostatic Specific Antigen] ● Note: Crappy test, clinically controversal Vitals: BP 130/80; O2 Sat 93% on room air HEENT showed no periorbital edema [periorbital edema is common presentation in nephritic syndromes] Abdomen: nontender, nl, no shifting dullness (ascites -> cirrhosis could account for his hypoalbinunemia) Extremities: pitting edema 2+ to the knees, Hands 1+ no pitting edema. Rectal: Prostatic enlargement (Grade II enlargement), Hemoccult negative Musculoskeletal: Somatic dysfx OA FrLsR, AA RR, C2 FSRRR T10-L11 NSLRR Tests: ● H&H low-> likely dilutional effect vs Anemia of Chronic disease ● Hyponatremia- likely from hypotonic hyponatremia EKG finding in hypokalemia = T wave inversion and U waves [these are the $ ones] EKG finding in hyperkalemia = Peaked T waves ● ● ● ● ● ● ● BMP , Coags: Nl Total Cholesterol: 400 high (This is an effect of the nephrotic syndrome, the liver kicks up its production of lipoproteins.) compensation for protein loss CH50 (complement, total)-> Low (Complement is inappropriately activated in a lot of these immune-mediated disorders, including membraneous nephropathy) ● CH50 (complement total): 49 LOW (70-160) [CH50 tests for compliment function of the classical pathway] Low albumin, proteins, high LDH Uric Acid: elevated; Calcium reduced 8.0 LOW (8.6-10.4) (pseudohypocalcemia) (both side effects of furosemide) PSA was nl ANA: negative [Anti-Nuclear Antibodies, test non-specific for autoimmune disease] LFT Total protein: 6.0 LOW (6.1-7.7) Albumin: 1.6 LOW (3.8-5.1) LDH: 297 HIGH (71-207) UA Specific gravity: 1.008 Protein: 3+ HIGH Microscopic: occasional granular casts, oval fat bodies 24 hour urine protein: 5.5g(>3.5= you've got that nephrotic syndrome) Serum Protein Electrophoresis: reduced Albumin (he's peeing it out) and elevated Alpha2 (marker of acute or chronic inflammation) Peak 1 Albumin: 1.6 LOW Peak 3 Alpha 2: 0.9 HIGH (secondary to acute or chronic inflammation) (not gonna be a thing, but for you future nephrologists): ● Decreased albumin: nephrotic syndromes, acute inflammation (amino acids being used by the liver to make acutephase reactants) ● Increased alpha 1: Acute, chronic inflammation,; cancer ● Decreased alpha 1: A1-antitrypsin ● Decreased alpha 2: Hemolysis ● Increased beta globulins: problem in breaking down fats (familial hypercholesterolemia), estrogen ● Decreased beta globulins: Low LDL, malnutritions ● Increased gamma globulin (G,A,M in that order): multiple myeloma if monoclonal and other cancers, acute/chronic inflammation if polyclonal, autoimmune, liver dz PA and lateral films showed hilar adenopathy and poor inspiration. but no edema/obstruction. Renal Echogram was normal. Each kidney was 12.6 cm (nl) Repeat CBC showed BUN elevated at 26 and Creatinine 1.4 >Editorial comment: this is an interesting BUN/Creatinine ratio that would be more typically in the range of a pre or postrenal azotemia Renal Biopsy (the money test here) showed mild mesangial changes in the glomeruli w/ thick basement membranes. Interstitium was normal. Immunofluorescence showed +IgG and C3-> granular, diffuse basement membranes -> PRIMARY MEMBRANEOUS GLOMERULONEPHRITIS Mild mesangial changes in the glomeruli with thick basement membranes IgG: +++ HIGH—Fine granular diffuse glomerular basement membranes C3: +++ HIGH—Fine granular diffuse basement membranes [Fibrogen, light chains] What the heck might these other tests mean? (Not exhaustive by any means, just examples) ● IgM-might clue you into fsgs, mixed cryoglobinemia ● IgA-IgA nephropathy (Berger's dz- most common nephritic syndrome in the world) ● C1Q-MPG1 ● Fibrinogen – Crescentic glomerulonephritis (eg Goodpastures, Wegener's) ● Light Chains: Multiple myeloma (dat bence-jones protein) Tx'd with 5 mg thiazide (metolazone) and 40 mg po furosemide, lisinopril CASE 1 Explanations : Immune suppression treatment (prednisone and cyclophosphamide) discussed but pt wasn't into it. Same thing with lipid lowering drugs, can’t really afford his pills [what a fantastic world] Metolazone – thiazide like diuretic Acts on distal convoluted tubule. Inhibits the sodium chloride symporter. Furosemide – Loop diuretic. Acts on Thick ascending limb Inhibits NKCC2. Can cause hypomagnesium and Hypokalemia. Pt was instructed to avoid NSAIDs-> inappropriate constriction of the afferent arteriole because you're interfering with prostaglandins *why give metolazone and furosemide? The use of Metolazone and Furosemide together even at low doses metolazone significantly potentiates the diuretic effects of furosemide and therefore simplifies the treatment of fluid retention. Sometimes furosemide dose has to be lowered after metolazone is started, to avoid an excessive negative fluid balance. Protein in urine: Multistix Neg Trace 1+ (30 mg/dL) 2+ (100 mg/dL) Criterion Neg 15 mg/dL 30 mg/dL 100 mg/dL 3+ (300 mg/dL) ≥500 mg/dL 4+ (>2000 mg/dL) ≥500 mg/dL Albumin Alpha 1 Alpha 2 Beta 1.6 LOW 0.2 Normal 0.9 High 0.6 Normal 43.7% 5.5% 24.3% 16.3% Gamma 0.4 Normal 10.2% IgM, IgA, CLQ HDL Hemoglobin Globulin (iron and other carrying) antibodies ***Creatinine clearance calculations*** Calculation information: This formula is applicable only if the serum creatinine is stable. Est. Creatinine Clearance = [[140 - age(yr)]*weight(kg)]/[72*serum Cr(mg/dL)] (multiply by 0.85 for women). http://www.mcw.edu/calculators/creatinine.htm Case 2 -Fried his kidneys by bottoming out his pressure - ATN 75 y/o m with a past med hx of hypertension presents w/ hypotension, following a respiratory illness, possible drug rxx? >Two weeks before visit, pt had a dry cough, fever (103-104), URI >Cephalexin was tried and didn't help, abx and htn meds were discontinued >Pt woke up with SOB/fever->unrelieved by positional changes >Denies chest pain/tightness/edema ● ● ● ● ● ● ● ● ● ● ● ● Hospital records showed: Severe HTN/Hypertensive Emergency (210/110), P 140, T 104, RR 28 and shallow +WBCs. Elevated CO2 [HTN emergency because there is also evidence of end organ damage] Elevated BUN and Low BUN/Creatinine Ratio CPK elevated at 469 but CK MM (specific for muscle) CK MB/Troponin (Heart) CK BB (Brain) all normal ➔ muscle is getting broken down , he's not having a heart attack. We call this rhabdomyolysis Chest X-Ray was taken which showed Pulmonary edema Later showed consolidation in the superior segment of the right lower lobe suggestive of lobar pneumonia ECG showed sinus tach, LVH, nonspecific ST/T wave changes Pt given acetaminophen and furosemide and IV Nitroglycerin (NTG), at which point BP completely bottomed out fell precipitously to 50/palp [So low that diastolic cannot be heard, only palpated]. Given two liters of intravenous normal saline. Endotracheally intubated General: End tidal CO2 readings of 35-40mm Hg after intubation Mildly agitated and bucking the ventilator [pts breathing is out of sync with the ventilator] Dopamine given to get his BP back up: Low dose dopamine was started as a continuous infusion with return of his systolic blood pressure to 100-110 systolic. Dopamine activates different receptors at different doses. ○ Low dose dopamine--renal perfusion: dopamine receptors in kidney ○ Medium dose: beta receptors ○ High dose: alpha receptors Monitor I/Os, pulses, temp Physical exam: the abnormals ● ● ● Rhonchi and rales Signs of consolidation-be familiar with tests like egophany, whispered pectoriloquy, etc Fundoscopy showed AV-nicking and copper wiring (is this ever going to be an extra credit question??); pigment crescent variation which looked totally freaky but is a normal variant Hematology: ● ● ● ● ● Hgb, platelets, Hct low WBC Elevated (leukocytosis) Neutrophilic Lymphocytopenia BUN and BUN/Creatinine ratio abnl ABG showed a mild alkalosis, possibly attributable to hyperventilation pH: 7.48 HIGH Sputum culture showed gram+ diplococci w/ PMNs-> Strep Pneumo (empiric treatment w/ ceftriaxone w/azithromycin; later switched to Penicillin G when sensitivities came back) Received vigorous fluid resuscitation and his dopamine was continued (2ug/k/min) with no detriment to his BP. Weaned off the ventilator over 12 hours. After extubation, his blood pressure was 107/73 his heart was 103, resp was 25 maintained on 4L of O2. Urine output averaged 20cc.hr. Bolus injection of furosemide 80mg did not increase flow of urine. Urine output remained shitty despite furosemide and all the rib raising/MFR he coulda asked for. Modified thoracic pump was initiated after the patient was removed from ventilator. Chapman’s points were treated q6h. (TART was found in T10-12; L1 with palpable tenderness at 11/1 o clock.) UAs were normal at first, but on day 3 of the hospital stay he got 1-5 WBC/hpf "high powered field"; 10-15 RBCs, and Renal Tubular Epithelial Cells (means the problem is intrinsic to the kidney, if we got casts they might look granular or "muddy brown") ● The presence of “muddy brown casts” of epithelial cells are pathognomonic for ATN. The necrotic tubular cells combine with blood and become brown casts seen in the urine. Urine chemistry showed elevated Urine Osmolality at 1400 and Increased FEna at 5%. (Note: A low BUN/Creatinine ratio ie <10 and an increased FeNA are two ways to distinguish a prerenal azotemia from ATN) Developed acute tubular necrosis (ATN) secondary to his hypotensive episode. The hematologists thought that thrombocytopenia and purpura-hemolytic uremic syndrome (TTP-HUS) was a possibility that plasma exchange was indicated. They believe that he had anemia secondary to sepsis or renal failure. Kidney biopsy was Nl->putative diagnosis of Acute Tubular Necrosis because of his hypotensive episode ● Other diagnostic possibility was TTP (classic pentad of fever, CNS signs, microangiopathic hemolytic anemia, thrombocytopenia and renal failure), but pt was showing no evidence of hemolysis (no increased urine urobilinogen, the blood values were normalizing, etc) Sent home on diuretics, potassium supplement. Case 3 – Sally Walker Case 149 ;Get the “ENDOCRINE PANEL” [Not a real test]- Pituitarydependent Cushing's syndrome [Cushing Disease] 21 y/o F with a "hormonal situation" ● moon face/buffalo hump/striae ● ● ● ● ● ● ● ● Denies ● ● ● ● Supraclavicular and dorsal fat pads increase hirsuitism (facial hair/male distributions) Developmental delay Hx of a tumor (astrocytoma) in the hypothalamic/pituitary area Periods "less regular than before" Cold intolerance Acne (well…depends on which part of the case you read.) Growth failure (cortisol is not nice to bones) HTN/edema weight changes changes in urine/stool Diabetes Physical Exam: Gen: buffalo hump. Skin: showed plethora, a redness in the face due to increased blood flow. In cases of excess cortisol, this is because the epidermis is thinned so the blood vessels are relatively closer to the surface. Abdomen: Central/truncal obesity, striae.. Extremities: No muscle atrophy-> you might expect this in cases of excess cortisol TEST: CBC ● Neutrophilic leukocytopenia - glucocorticoids reduce adhesion/margination, so the bone marrow keeps producing them ● Eosinophilia is associated with Cushing’s disease , not seen in this patient. Lipid profile ● Elevated TG's, otherwise unremarkable. In full-blown Cushing's, we'd expect disturbances. We attributed this to her working at McDonald's, because 'Murica. "Endocrine" Panel: ● ● ● Prolactin: normal Serum B-hCG: NEGATIVE TSH: normal Elevated serum cortisol = 19.9 (range 2-10) (they mentioned it being measured at 4pm because cortisol is secreted in a diurnal pattern, with levels highest in the AM and falling from there) ○ The next reading of her cortisol at 8am was actually normal Elevated DHEA-S ○ This is an androgen specific to the adrenal cortex Dexamethasone suppression test Dexamethasone is synthetic (super potent) cortisol. In a normal pt, administration of a low dose around midnight will lead to low levels of cortisol in the AM. Failure to suppress a low dose does not distinguish the etiology of the dz. High dose dexamethasone tests are used for that-> high dose dexamethasone will suppress pituitary sources of ACTH (Cushing's disease); ectopic sources of ACTH like a small cell lung cancer or adrenal adenomas will not be suppressed on high-dose dexamethasone. Dexa 0.5mg q. 6h administered for two days Low dose dexamethasone showed nl serum cortisol levels but increased cortisol in the urine; ACTH levels were nl ● A two-day dexamethasone test was administered (.5 mg/q6h for 2 days), which showed nl urine cortisol Ruling out ectopic and adrenal sources of cortisol/ACTH: We didn't get imaging w/ contrast because the pt was a wimp, but the adrenals looked nl. Chest CT was clear. ● Pituitary MRI: T1 weighted (grey matter is gray, white matter is white, fat is white and water is dark) showed an enlarged fourth ventricle that was irregular. That and a partially empty sella were attributed to her past surgery. Pituitary gland was compressed into the floor of the sella. Sella is filled with CSF. [Empty sella syndrome can be caused by radiation] [T1 MRI is best modality for brain anatomy, MRI contrast doesn’t have a large effect on T1 ] In the two months it took us to do all of this crap, the Pt has florid (obvious) Cushing's syndrome and a peptic ulcer. Note: Corticosteroids inhibit the production/action of prostaglandins, which are protective in the stomach mucosa. Hence a pt on steroids or w/ Cushings would be more prone to these Ddx: Pituitary-dependent Cushing's syndrome (later confirmed by immunohistochemistry that she had a microadenoma (2mm) that was secreting ACTH) ● Microadenomas are <10 mm ● Cushings disease when cortisol hypersecretion is due to pituitary excessive secretion of ACTH. We did not catheterize her inferior petrosal sinus (what we might do to see which side is secreting ACTH ectopically); it was better to just cut the pituitary out (transphenoidal hypophysectomy; recall the sella is in the sphenoid bone) Tx'd before the surgery: ketoconazole (used for antifungal and ACTH suppression, inhibits p450 enzymes) and famotidine (H2 blocker for peptic ulcer sx) until her surgery. After she was de-pituitarized, we tx'd: prednisone (synthetic cortisol), Levothyroxine (Synthroid), and DDVAP (Desmopressin; synthetic ADH for volume regulation. Also stimulates release of von Willebrand factor from endothelial cells by acting on the V2 receptor.) Addison’s disease: Failure of adrenal corticies to produce adrenocortical hormones. It is most frequently caused by primary atrophy of adrenal cortex by autoimmunity against the cortex cells. Mineralocorticoid deficiency: lack of aldosterone – causes less sodium reabsorption, water is lost in urine, hyponatremia, hyperkalemia, mild acidosis, blood volume drops Glucocorticoid deficiency: cannot maintain significant quantities of blood glucose between meals because there is lack of control of gluconeogenesis Melanin Pigmentation: dark melanin pigmentation of the mucous membranes and skin. This is caused by excess ACTH secretion trying to compensate for lack of adrenalcorticoids. Addisonian Crisis: output of glucocorticoids does not increase during stress. A person is likely to have an acute need for excessive amounts of glucocorticoids. Stress dosing with meds. Case 4-Did you take that diabetes run in path yet? We really want you to take that. – Diabetic complications neuropathy, micro/macrovascular disease, nephropathy 29 y/o suuuuuuper compliant diabetic (type I) M with a sudden loss of vision in the L eye *2 days; ● ● ● ● ● ROS/PE: ● ● ● Loss of sensation in LE – typical stocking part of the "glove and stocking" pattern Unsteady gait – from peripheral neuropathy Retinopathy – had a vitreous hemorrhage in the right (tx'd w/ panretinal photo-coagulation) ○ "OD"-vision in right eye; "OS"-vision in left eye; "OU" vision in both eyes Family Hx DM type 1 (for boards, know HLA DR3/4) Meds-Glargine (long acting/basal)+Lispro (short acting/at meals); doesn't follow an 1800 calorie ADA diet No polydipsia/urea HTN 230/130 (Macrovascular complications/MI is the most common cause of death in diabetics); Pulse 120 - regular, w/ hyperdynamic precordium (you can see the heart beating out of his chest, Kali-Ma style)-> attributed to his LVH ○ Malignant HTN systolic greater than or equal to 180, Diastolic greater than or equal to 120. ○ Hypertensive Urgency >180/120 w/o evidence of end-organ damage and Hypertensive EMERGENCY w/ evidence S4 -"Tennessee"; atria filling against a noncompliant ventricle ("atrial kick") ○ Pt did not have an S3 "Kentucky", which can be a nl sound in a young person, which happens during diastolic filling in patients >40 S3 = heart failure From Wikipedia: ● The fourth heart sound or S4 is a rare extra heart sound that occurs immediately before the normal two "lub-dub" heart sounds (S1 and S2). It occurs just after atrial contraction and immediately before the systolic S1 and is caused by the atria contracting forcefully in an effort to overcome an abnormally stiff or hypertrophic ventricle. ● The third heart sound or S3 is a rare extra heart sound that occurs soon after the normal two "lub-dub" heart sounds (S1 and S2). The S3 is associated with heart failure. It occurs at the beginning of diastole, approximately 0.12 to 0.18 seconds after S2.[1] This produces a rhythm classically compared to the cadence of the word "Kentucky" with the final syllable ("-ky") representing S3. One may also use the phrase "SLOSH’-ing-in" to help with the cadence (SLOSH S1, -ing S2, -in S3), as well as the pathology of the S3 sound.,[2] or any other number of local variants. ● S3 may be normal in people under 40 years of age and some trained athletes but should disappear before middle age. Reemergence of this sound late in life is abnormal[3] and may indicate serious problems like heart failure. The sound of S3 is lower in pitch than the normal sounds, usually faint, and best heard with the bell of the stethoscope. ● ● ● CBC: 1+ Edema B/L but hair in the pretibial regions [hair on top toes - checks arterial sufficiency in distal circulation (Lack of hair would worry you for circulation/microvascular problems)] Neurological: Decreased vision bilaterally. Motor strength 4+. Decreased pinprick up to the mid-calf bilaterally. Slightly decreased proprioception of the large toes bilaterally. Vibration sense was absent at the ankles. [Diabetic peripheral neuropathy] MSK: TART palpated in upper cervical area and in the thoraco lumbar junction. Small tender areas just above the umbilicus (at 11:00 and 1:00) and posteriorly B/L adjacent to the spinous process L1. [Chapman’s points kidneys] ● Fundoscopy showed retinal hemorrhage in the R eye and tractional retinal detachment in the L eye, "rippley" effect. [Folding on fundoscopic exam may clue you in to detached retina]-> Past Bonus o What does a retinal detachment look like on fundoscopy - ● Cloudy vitreous B/L. There were vitreous hemorrhages bilaterally ● ● ● Normochromic, normocytic anemia, low RBC [Kidney disease -> low EPO] Elevated WBC, platelets Neutrophilic lymphocytopenia Blood Chem: ● Na down, K+ elevated ○ Clinical: administer K+ when administering glucose to a pt in DKA, because insulin drives K+ into cells and the pts will become hypokalemic when you treat him ○ Clinical clue to diagnosing DKA: THERE NEEDS TO BE AN ANION GAP ● Elevated BUN/Creatinine ● ● Criteria for diagnosis of DM ○ Random glucose >200 with symptoms ○ fasting glucose >126 ○ Oral glucose tolerance test >200 @ 2 hours HbA1c -> 12 (Normal 4-5.9, good DM control <7) ○ Indicator of blood glucose control over the last 120 days Oh and the eye stuff: Vitreous hemorrhage and hypertensive emergency Ophthalmologist recommended surgery [To be performed 48 hours post maintained BP] B/L severe proliferative retinopathy with dense vitreous hemorrhage. In left eye probably retinal detachment superiorly Underwent vitrectomy membranectomy, laser photocoagulation. Kidney stuff: ● Granular casts, hyaline casts ○ Granular=intrarenal dysfx ○ Hyaline casts=protein, nonspecific indicator ● Oval fat bodies, Lipid casts-> Nephrotic syndrome (You may expect Kimmelstiel-Wilson bodies on kidney bx) Proteinuria, Hematuria, Glucose 3+ [~1000 mg/dl plasma concentration estimate] ○ No ketones ECG: L atrial/ventricular enlargement ● (U waves/flattened T waves a sign of hypokalemia) [Past bonus!] Renal US showed ● Increased renal parenchymal echogenicity b/l; nonspecific (no hydronephrosis) HTN tx'd with nifedipine (Calcium channel blocker), clonidine (Alpha 2 agonist), furosemide (loop) Optho consulted for Surgery- vitrectomy, membranectomy, and laser photocoagulation was planned Enalapril was begun, got super hyperkalemic (> 6.0), so it was stopped You generally put diabetics on ACE inhibitors to dilate the efferent arteriole, reducing GFR and the high filtration pressures diabetics tend to have Repeat EKG preop - K was 7- (hallmark- Peak T Waves); given Sodium polysterne sulfonate (Absorbs K in the GI track) , Required a kidney/pancreas transplant, went on prednisone, cyclosporine, azathioprine (all for immunosuppression) ● ● Pancreatic duct emptied into urinary bladder-you can use this for a UA for pancreatic f(x) [Monitors rejection] Patients go into surgery diabetic and can leave the OR no longer diabetic Case 5 -You got diabetes! Everybody gots diabetes! – Preeclampsia ● Triad of preeclampsia = maternal hypertension, proteinuria, and edema 20 y/o Type I diabetic (13 year history) F; 34 weeks pregnant seeking prenatal care. ● Swollen ankles* 1 month Pitting Edema 1+ Barely detectable impression when finger is presssed into skin. 2+ Slight indentation. 15 seconds to rebound 3+ Deeper indentation. 30 seconds to rebound. 4+ > 30 seconds to rebound. http://web.missouri.edu/~proste/tool/cv/pitting_edema.htm ● ● ● ● ● ● ● ● ● +frequency of migraines [Could indicate HTN] Occasional heartburn 30 lb wt gain (25-35 nl for full term) Burning/itching w/ pee (denies +frequency) ○ +white/clumpy discharge-Candida (pseudohyphae) - Cottage cheesy ○ Recurrent yeast infections are a complication of DM Significant hx of HPV (types 6,11 typical for warts; 16/18 are the cervical CA ones) [Know these!] Denies n/v/changes in bowel movements/SOB/changes in stream (color/odor) 2 previous miscarriages-> this makes her a G3P0020 ○ Gravida Para Notation: G=#pregnancies, P= "Florida Power And Light" (Full Term, Preterm, Abortions, Living Children) ○ Uncontrolled DM is a course of miscarriage in early pregnancy 2100 ADA diet Glucose 100-200; "sometimes 250-300" Hospitalizations: Recent tooth infx, "diabetes got out of control" Meds ● ● PE: ● ● Lispro [Humalog] 22 units w/ meals; NPH [aka Humulin] (long-acting insulin-insulin of choice in pregos) ○ Has had to increase dose throughout pregnancy Mylanta: − Aluminium hydroxide – 200mg − Magnesium hydroxide – 200mg − Simethicone – 20mg +BP (140/85) ->Criteria for preeclampsia (>140/90; w/ proteinuria OR low platelets); you might also see hyperreflexia/clonus ∗ Of note: New ACOG guidelines (Nov 2013) have recently changed criteria, grading and treatment for hypertension in pregnancy. Might not yet be in your text books or boards but keep in mind when on rotations. Baby fetal heart tones 130 (110-160 nl) Vagina : ● ● Previous miscarriages (decidual tissues/products of conception) D & C s (Dilation and Curettage) condyloma acuminata - tx'd with podophillin* (a resin). (Editorial: this drug is out of date, contraindicated in diabetics and pregnant ladies) condylomata acuminate o Podophyllin – arrests (or used to) epithelial growth by binding directly to micortubules. ● Prior yeast infx had been treated w/ Nystatin/Monostat for her and her dude. ○ Also showed an ectropion-basically when the endocervical columnar epithelium protrudes into the os and becomes all stratified and squamous. (Caused by pregnancy, estrogen or cervical lacerations by delivery among other things) ● Cheilitis = a sign of nutritional deficiencies (loads of vitamin deficiencies have this sign), contact irritation, infx, or Candida Gingivitis – bleeding gums are common in pregnancy Mouth: ● Tests: ● ● ● ● Pap normal and Thayer Martin (media for gonorrhea) negative Blood type A+ (so we don't have to worry about Rh compatibility, or hemolytic dz of the newborn. For boards, that's a type II hypersensitivity rxn! Only matters if mother is RH negative and father is RH positive/blood type unknown. If it was an issue, we'd administer RHOGAM. Rubella titer 1:24 (ie nl) (ToRCHHS infections: Toxo, Rubella, CMV, Herpes, HIV, Syphilis. Rubella and CMV are two causes of "blueberry baby") Blood sugar showed proteinuria and shitty diet control Blood Chem ● Hypokalemic,Ca, Mg -> dilutional (hypervolemic state in pregnancy) ● Low creatinine -> increased GFR (nl in pregnancy) ○ +Renal blood flow (by 80%!!) ● Fasting glucose 115 ● K+ 3.7 LOW (Normal for pregnancy) ● Creatinine: 0.5 LOW (Normal for pregnancy) ● Fasting glucose: 115 HIGH ● Mg: 1.2 LOW (Normal for pregnancy)[Changes relate to blood sugar levels and preeclampsia among other things] CBC ● ● WBC: 13.5 HIGH (Normal for pregnancy) Platelets: 250 NORMAL [if abnormal consider Preeclampsia or HEELP] ● ● ● ● ● Protein: 2+ HIGH Glucose: 1+ HIGH WBCs: 5 HIGH Leukocyte esterase: positive Nitrite: positive ● ● +WBC, leukocyte esterase, nitrite, bacteria-> She's got a UTI proteinuria, glucosuria -> DM UA ● Pt was admitted and swabbed for Group B Strep - (normally ordered at ~36 weeks, but we were thinking about inducing her) and UTI tx'd (later determined to be E Coli) with ampicillin ● ● ● ● ● ● ● HbA1c was 12.7 (eek Goal should be < 7.0 or better yet <6.5 ) [Tells history of blood glucose control for 120 days – the life span of RBCs, unless there is a hemolytic condition] Renal tests - proteinuria WNL, but reducing creatinine clearance -> fetus squishes renal arteries, reducing GFR very late in pregnancy Fetal non stress test (put baby on the heart monitor, chill out for 20 minutes)= 5 accelerations (>2 recommended, so that's good) Growth @ 35 weeks measured biparietal diameter=nl (concern w/ babies to DM mothers, can be huge, called macrosomia) Amniocentesis showed Lethicin/Sphingomyelin ratio 2.1; Phosphatidylglycerol low (determinants of fetal lung development) [Seems likely Bonus] Fetal head was Ballottable - baby's head is down and pressing on the head allows for motion out of the pelvis. Cervix was unripe What is an noninvasive test to acutely assess fetal well-being in high risk pregnancy? – [Nonstress test http://www.webmd.com/baby/checking-fetus-in-high-risk-pregnancy ] Pt returned at 36 weeks, was induced (via oxytocin) and eventually delivered a macrosomic (growthpromoting effects of insulin) baby. (Had to do a C section eventually) ● If you were to peek at their islets of langerhans, you'd see diffuse hyperplasia because the baby's pancreas works overtime to deal w/ mom's hyperglycemia; hence hypoglycemia in the infant after delivery) ● Infant became hypoglycemic 2 hours after birth ● Treated with IV dextrose for 48 hours APGAR (appearance, pulse, reflex, activity, respirations) was decent-7 and 9. Case 6 – Resisting Censored Dead Baby Joke - Ectopic Pregnancy 26 y/o G3P1011** F w/ a CC of abdominal pain and heavy (non-clotting, bright red, no tissue) bleeding. FDLNMP 7 weeks ago "might be pregnant" ** (....teeeeechnically G2P1011 since we hadn't done the BhcG yet....) Gravida 3 [2, we did not have a confirmed pregnancy at this time] Para 1011 TPAL: Term Preterm Abortion Live birth Had a miscarriage one year ago—four months [S/P SAB @ 16wks – 1yr ago] Bleeding has soaked through two pads ↳ Denies n/v/fevers, chills, night sweats, SOB, chest pain, dysuria, constipation, diarrhea Recently tx’d w/ Bactrim for UTI [Trimethoprim Sulfamethoxazole = Bactrim] ▪ Bactrim is contraindicated in pregnancy. (Category D) Medication o Category A- A-OK to use in pregnancy o Category B- Animal studies show no adverse effects. o Category C- NO animal studies to support adverse effects o Category D- + human teratogenicity. Use if only need to. MAY HAVE BENEFIT TO USE o Category X- + Humans or animal teratogenicity. NO BENEFIT TO USE. Musculoskeletal: TART in the upper cervical and lower thoracic areas: OA F RRSL Abdomen: Mid-lower abdominal/suprapubic tenderness w/ involuntary abdominal guarding. Nl bowel sounds, soft and distended. [Should have performed tests for appendicitis] Pelvic exam: Bright red blood at the introitus/perineum. Speculum exam-pink mucosal membrane w/ blood clots/blood-> cervix was bleeding. Cervix closed. No cervical motion tenderness->"chandelier sign" (suggests PID or ectopic pregnancy); Uterus consistent w/ gestational age of 6 weeks. Right adnexal tenderness. [Past bonus was Cervical Motion Tenderness = chandelier’s sign (think of the Song, “Im gonna swing from the chandelier… Pain is so severe that she jumps to the chandelier) This is not an OMM TECHNIQUE ] CBC/Blood chem nl ● If she were super pregnant, we might expect Hct to be low because of her hypervolemic state. Estrogen and +Aldosterone would play a role here B-hcg + ● Serum hCG: 14 IU/ml [Peaks around 90,000 around 8-11 weeks gestation] ● Things to consider w/+ hcG-> Normal pregnancy, ectopic pregnancy, hydatidiform mole (w/ hella elevated b-hcG); can be a tumor marker for Germ cell tumors: (seminomas, dysgerminoma) or choriocarcinomas ○ B-hcG test is specific for the B subunit (because it shares its alpha subunit w/ TSH, FSH, and LH) ● B-hcG rises ~day 8, peaks ~weeks 10-12, falls down but not undetectable by weeks 16-20 US: ● ● Eccentric shaped gestational sac without evidence of a fetal pole. 'Pseudo sac' in the uterus (caused by the prego hormones' effect on uterine lining). Complex heterogeneous mass that looks consistent with a 7 week+ fetus. Fetal tissues were in the right adnexa w/o surrounding myometrial tissue->ectopic (most common location-> ampulla of the uterine tube) Intervention: ● Thiopental and fentanyl; succinylcholine was used for muscle relaxation and endotracheal intubation was performed. ● Nitrous oxide, oxygen, isoflurane. ● laparoscopic removal of the tissues; adhesions were noted [PID can lead to Ectopic pregnancy]. ● Right fallopian tube was noted to be dilated and an unruptured apullary ectopic pregnancy was noted ● 20-25 cc of dark old blood noted in the rectouterine pouch aka Pouch of Douglas [most dependent portion of female pelvis, where fluid pools when sitting or standing] ● ● ● ● Dilute vasopressin was injected within the mesosalpinx and ectopic pregnancy was removed. Rt ovary stuck to right pelvic side wall. Rt fallopian tube somewhat blunted. Left fallopian tube stuck to abdominal wall. Adhesions were released. B-hCG followed to zero [persistent elevation in retained products of conception or Hydatidiform Mole] Because the patient was Rh+, RHOGAM (Rho D immune globulin) was not a consideration here General US considerations: Normal nongravid uterus would show an 'endometrial stripe' (darkness of the endometrium on US, tells us how thick the endometrium is) Physiological changes during pregnancy Hormonal: levels of progesterone and estrogen rise continuously, increased B-hCG—maintains progesterone secretion, increased prolactin levels Physical: weight gain (25-35lbs) Breast size: increases (1-2 cup sizes) Cardiovascular: plasma and blood volume increase 40-50% to accommodate for the fetus— increase in plasma volume due to increased aldosterone; increase in heart rate, stroke volume and cardiac output; vasodilation due to excess progesterone Hematology: increased blood volume but not increased RBC so Hct low because of dilution factor Edema in feet Renal: GFR increases by 50%--as a result: decreased creatinine, and BUN and glucosuria may be seen GI: nausea and vomiting due to excess B-hCG MSK: lumbar lordosis Case 7-We get it, sex kills you. Squamous cell carcinoma of the cervix- Stage III 33 y/o F w/ a CC of infertility *4 years ● Periods irregular − Menarche at age 12 − FDLNMP 10 days ago sometimes 2-3 months between periods = Could indicate anovulation No Miscarriages or abortions = G0 P0 Denies hx STDs but had untreated "pelvic pain" in high school. Early age of first intercourse (14yo). Multiple past sexual partners (~5) = Could be PID − ● ● ● Denies pain/bleeding w/ intercourse = Pain with intercourse is called dyspareunia ● Denies galactorrhea = (galactorrhea + amenorrhea = possible prolactinoma). No hirsutism or weight gain = (Signs endocrine dysfunction) Denies family hx of infertility, mom had ovarian CA Adequate attempts at fertilization ● ● ● ● ● − Have intercourse 2-3 times a week, use variety of positions = Infertility can be diagnosed following one year of trying Husband has not been tested (denies hx hernia repair, mumps, trauma or chilling in hot tubs) = [Infertility is male based 40-50%] Last pap exam 3 years ago − Has never had an abnormal pap PE: Abnormal findings: ● Right adnexal tenderness ● Inflammation at squamocolumnar junction = Transition zone between endocervix and exocervix = Where sample during PAPs because that's where cells are most susceptible to HPV ● Retroverted uterus (normal uterus=anteverted, anteflexed). No condyloma acuminata (warts, usually HPV 6 and 11) noted. [Condyloma lata are a sign of secondary syphilis] Tests: ▪ "STI Panel": ● HIV (Elisa as a screening/Western to confirm) ● Chlamydia (NAAT-nucleic acid amplification test) ▪ ▪ ▪ ● RPR (Syphilis) ● Gonococcal culture Ovulatory Biphasic basal body temp: progesterone is responsible for the ++ in body temp and respiration during ovulation (effect on hypothalamus) [Temperature following ovulation increases 0.5 degress] Post-coital testing-looking for hostile cervical mucous or anti-sperm antibodies Semen analysis: all within range = >10 motile sperm were present 6 hours post-intercourse Pap smear: Pap smear showed dysplastic cells w/ smaller, pyknotic, irregular nuclei-> ddx of LSIL (Squamous intraepithelial lesion) Pyknosis = irreversible condensation of chromatin in the nucleus of a cell undergoing necrosis or apoptois. Karyorrhexis = fragmentation of the nucleus (Cervical Intraepithelial Neoplasia I-> 1/3 of the thickness of the epithelium, caused by HPV; CINII=2/3 and CIN III=to the basement membrane) Grading of paps. Pt referred colposcopy, which would have explored this further, patient failed to follow up despite 3 letters delivered via certified mail. [Covers our asses for liability] She returned two years later w/ fatigue, intermenstrual bleeding, fullness in the pelvis and postcoital bleeding. (70% women will clear CIN I or keep it), CBC shows Microcytic Anemia [MCV <80] Pelvic exam showed a blood stained introitus with a cauliflower lesion replacing cervix. Lesion/Cervix was 6cm in diameter and fixed to the anterior pubic ramus [That is about the size of a clementine]. Cervical biopsy: full thickness of epithelium has been replaced by immature undifferentiated cells with enlarged mildly hyperchromatic cells proliferating in a disorderly fashion. ● Area of induration (induration = sclerosis or hardness) extended from anterior vaginal wall-> lower 1/3 vagina. Tumor extended into the left parametria, but not to the side wall. Tumor was stage III because of involvement of the distal vagina ▪ Somatic Dysfunction: ● Cervix is innervated from S2-4 ● Uterus is innervated from T10-L1 ● Her Pelvic diaphragm is tight and restricted in motion. ▪ Punch biopsy of the cervix ↳ showed small cell carcinoma of the cervix. CBC/UA was significant for mild microcytic anemia and RBC in the urine, likely due to the bleeding. She had evidence of Left hydronephrosis (mass effect blocking the ureter) Pt underwent external radiation treatment ○ Sx diarrhea, responding to diphenoxylate (opioid agonist antidiarrheal) ○ Anal discomfort, responded to hydrocortisone Radiation treatment didn't work ○ Tandem and interstitial Syed template implant, 45 hours of radiation tx w/ Cesium The cancer then metastasized to the abdomen and the pt passed away ○ One option she could have had if the cancer hadn't spread as much could have been a pelvic exenteration-removal of the tumor, bladder, and rectum ▪ ▪ ● ● ● Staging of Cervical Cancer: