OB Delivery Complications
advertisement

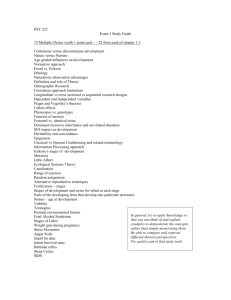
OB Delivery Complications Condell Medical Center EMS System ECRN Packet Module I 2008 Prepared by: Sharon Hopkins, RN, BSN, EMT-P Objectives Upon successful completion of this module, the ECRN should be able to: list physiological changes in pregnancy. identify the stages of labor. describe the assessment of a patient in labor. explain the contents of the OB kit. identify obstetrical emergencies. describe how to care for a prolapsed cord, a breech delivery, & meconium staining. successfully complete the quiz with a score of 80% or better. Physiological Changes in Pregnancy Reproductive system Increase in size of uterus Increased vulnerability to injury During pregnancy uterus contains 16% of the total blood volume Extremely vascular organ during pregnancy Uterus and fetus insulted if blood flow diminished Normal Fetal Positioning Changes in Pregnancy cont’d Respiratory system Increase in oxygen demand & consumption 40% increase in tidal volume Amount of air in or out in one breath Only slight increase in respiratory rate Diaphragm pushed upward decreasing lung capacity Changes in Pregnancy cont’d Cardiovascular system Cardiac output increases Maternal blood volume increases by 45% Heart rate increases by 10 – 15 beats per minute B/P decreases slightly in first 2 trimesters B/P normal in 3rd trimester Supine hypotensive syndrome after 5 months if heavy weight of uterus presses on inferior vena cava (when mother lying on her back) Changes in Pregnancy cont’d Gastrointestinal system Nausea and vomiting common in 1st trimester From hormone levels and changed carbohydrate needs Delayed gastric emptying Watch for vomiting and airway compromise Hands-on physical abdominal assessment difficult due to compression and shifting of abdominal organs Changes in Pregnancy cont’d Urinary system Increase in renal blood flow Urinary frequency is common Urinary bladder displaced more forward and higher increasing vulnerability to injury to the urinary bladder Musculoskeletal system Waddling gait due to loosened pelvic joints Low back pain due to change in center of gravity First Stage of Labor Dilatation Stage Begins with onset of true labor contractions Ends with complete dilatation and thinning of the cervix Cervix dilates from a closed position to 10 cm (approximately 4 inches) Duration usually longer in 1st pregnancy Early contractions mild, last 15 – 20 seconds coming every 10 – 20 minutes End of 1st stage contractions last 60 seconds and are coming every 2 – 3 minutes Second Stage of Labor Begins with complete dilatation of cervix Ends with delivery of fetus Can last 50-60 minutes in 1st deliveries Pain felt in the lower back Mother has the urge to push Bag of waters usually ruptures in this stage if not already ruptured Crowning is evident Definitive sign of imminent delivery Third Stage of Labor Begins immediately after birth of the infant Ends with delivery of placenta Placenta generally delivers within 5 – 20 minutes Signs of placental separation Gush of blood from vagina Change in size, shape, consistency of uterus Umbilical cord length increases Mother has the urge to push Assessment of the Patient in Labor Ask expected due date Gravida – number of pregnancies First time deliveries tend to take longer – 16 – 17 hours Labor tends to shorten with subsequent pregnancies Para – number of live births Is it “gravida and para” or “para and gravida”? Note: “G” comes before “P” in the alphabet; you must be pregnant before you can deliver Assessment of the Patient in Labor Determine how long mother has been in labor Ask how long previous deliveries took Ask if bag of waters is intact or has broken Delivery is quicker once bag of waters has broken Are there any high risk concerns the mother is aware of Assessment of the Patient in Labor Time duration & frequency of contractions Duration is from the beginning of one contraction to the end of that contraction Frequency is how far apart contractions are Measured from the beginning of one contraction to the beginning of the next contraction Contractions lasting 30-60 seconds and coming every 2-3 minutes apart indicate imminent delivery Signs of Imminent Delivery Crowning Bulging perineum Bulging of the fetal head past the vaginal opening during contraction Presenting part pressing on perineum Urge to push Note: High index of suspicion in female with abdominal pain and cramping (esp in a pattern) and denies pregnancy OB Kit Contents Sterile gloves Drape sheet Gauze sponges Disposable towels 2 alcohol preps 2 OB towelettes Bulb syringe Receiving blanket 2 umbilical clamps 2 nylon tie-offs Scalpel or scissors OB pad Plastic bag Twist ties Infant cap 2 wrist ID bands OB Kit Contents Newborn At Delivery Preventing Hypothermia in a Newborn Dry them; Wrap them; Cap them APGAR Assessment – 1 & 5 minutes A – appearance Most visible, least helpful Typical for pink trunk and blue distal extremities P – pulse 100 or above is acceptable 80-100 – stimulation needed <60 – start compressions APGAR cont’d G – grimace (irritability) Includes coughing, sneezing, crying A – activity Active motion, flexing of extremities R – respiratory effort Strong cry Majority of scores are 7–10 indicating a healthy infant requiring routine care Scores 4-6 indicate moderately depressed infant requiring oxygen & stimulation APGAR Score Criteria 1 2 Appearance Blue or pale Pulse Absent Blue hands or feet < 100 Entirely pink >100 Grimace – Absent Grimace Cough, sneeze Activity Limp Active motion Respirations Absent Some extremity flexion Weak cry, hypoventilating reflex irritability 0 Strong cry Inverted Pyramid Drying, warming, positioning Suction, tactile stimulation Oxygen Basic BVM skills Chest Compressions Intubation Advanced Meds skills OB Complications – Supine Hypotensive Syndrome Can occur especially after 5 months gestation Heavy weight of uterus compresses inferior vena cava when mother in the supine position Interferes with blood flow returning back to the heart Intervention Transport women over 5 months pregnant lying or tilted towards their left side Remember: Lay left OB Complications – Seizures Consider causes Hypoglycemia – check glucose levels on all patients with altered level of consciousness Epilepsy – check for ID; protect airway Eclampsia – protect airway Intervention For any prolonged seizure activity, need to consider using BVM to support ventilations and provide oxygenation Transport lying/tilted left if over 5 months gestation Region X SOP for Seizures from Eclampsia Check the blood sugar level on all patients with an altered level of consciousness For active seizure, administer Valium 5 mg IVP slowly over 2 minutes May repeat Valium 5 mg slow IVP Titrate to control seizure activity Maximum total 10 mg Valium, if given, has sedating effect on mother & fetus EMS should verbally inform/remind ED and OB staff of use of Valium in the field OB Complications – Breech Delivery Buttocks or feet present first Approximately 4% of all births Increased risk Maternal trauma Prolapse of cord Cord compression Anoxia to the infant Intervention Advanced medical intervention at the hospital Rapid transport important Breech Presentation Breech Delivery cont’d Intervention As legs deliver, support legs across forearm If cord is accessible, palpate often If able, loosen cord to create slack After torso and shoulders deliver, gently sweep down arms If face down, gently elevate legs & trunk to facilitate delivery of head NEVER PULL INFANT BY LEGS OR TRUNK Breech cont’d If head not delivered within 30 seconds Reach 2 gloved fingers into vagina to locate baby’s mouth Push vaginal wall away from baby’s mouth to form an airway Keep your fingers in place and transport immediately Keep delivered part of baby warm Cover with a blanket If head delivers, anticipate neonatal distress OB complications – Prolapsed Cord Perform a visual exam as soon as possible whenever a mother states her bag of waters has ruptured Elevate the mother’s hips or place knee-chest Have patient breath through the contractions so she doesn’t push Placed gloved hand into vagina and raise presenting part to get pressure off cord Keep cord between fingers to monitor for pulsations Cover cord with moist dressing, keep warm Prolapsed Cord OB Complications – Nuchal Cord Cord wrapped around infant’s neck Increase mother’s O2 to 100% nonrebreather mask Slip fingers around cord and lift over infant’s head Proceed with delivery If unable to reposition cord, place 2 OB clamps, cut cord between clamp, release cord from around neck Proceed with delivery Nuchal Cord (C-section) Meconium Dark green material found in the intestine of the full-term newborn. It can be expelled during periods of fetal distress (ie: hypoxia) If found in the infant airway, could compromise ventilations Meconium Staining Fetus has passed feces into amniotic fluid Occurs between 10-30% all deliveries Not unusual to observe in breech delivery In normal head-down delivery indicates fetal hypoxia Hypoxia increases fetal peristalsis and relaxation of anal sphincter The darker the color/staining, higher the risk of fetal morbidity Meconium Stained Baby Airway needs to be cleared to avoid aspiration of meconium Suction and clear airway before infant needs to take that first breath Meconium Staining If meconium is thin and light in color and the infant is vigorous Most meconium can be cleared away with bulb syringe ALWAYS suction mouth then nose, in that order Suctioning the nose stimulates breathing in the newborn Want to clear the mouth 1st so first breath is as clean as possible Limit suction (2 seconds per Region X SOP) Meconium Staining If infant is not vigorous Respiratory rate decreased Decreased muscle tone Heart rate < 100 Use meconium aspirator to clear airway This will take coordination and best accomplished with 2 persons working as a team Meconium Suctioning Steps include intubation Most efficient when performed as a 2 person team Time is essential May need to perform 2 intubation insertions Use each ETT once Meconium Aspirator Connect small end of meconium aspirator to suction line connecting tube Turn suction down to 80 mmHg Insert endotracheal tube Don’t anticipate visualizing landmarks – they may be obscured by meconium Connect larger end of aspirator to ETT Place thumb over suction control port and slowly withdraw ETT (< 2 seconds) Discard ETT after one use Meconium Aspirator Aspirator can be used a second time on infant with new ETT each time Limit suction to <2 seconds Meconium Aspirator ED Location CMC In peds crash cart On Broselow cart LFH In bins on wire rack shelves Case Study #1 EMS arrives on the scene for OB call Patient is 24 y/o and states she is in labor What assessment questions specific to an imminent delivery need to be asked? What needs to be evaluated during the physical assessment Case Study #1 Assessment questions Gravida? Para? Due date? High risk concerns? Length of previous labors? Bag of waters intact? Ruptured? Duration and frequency of contractions? Case Study #1 Physical exam – position patient to evaluate Crowning Evidence of bulging perineum Involuntary pushing Signs of prolapsed cord Evidence of profuse bleeding Case Study #1 History G2P1 EDC in 1 week No complications anticipated Previous labor 12 hours Bag of waters has ruptured Contractions are 5-6 minutes apart and lasting 20-30 seconds There is no bulging or crowning Does EMS stay & prepare to deliver or transport? Case Study #1 You could most likely begin transport with OB kit reached out in case labor progresses What stage of labor is the patient in? First stage If the patient delivers, how many run reports need to be written? Two – one for the mother, one for the infant What is your role during delivery? Support the presenting part Check for nuchal cord Suction mouth Then nose Head and shoulders delivered Have a firm grip on infant Cheesy covering and moisture make them slippery After shoulders, rest of the body will slip out fast Clamping & cutting the cord After cord is done pulsating, clamp 8″ from infant’s navel with 2 clamps placed 2″ apart Watch for blood leakage from infant’s cord Reinforce with additional clamps as needed 3rd Stage of Labor – Placental stage Watch for excessive bleeding (>500 ml) Prepare to perform fundal massage Need to feel uterus become firm – size of the uterus will depend on the size of the fetus Fundal Massage Newborn dried off, cord clamped & cut What’s his APGAR? Case Study #2 Mother calls EMS because “my baby is coming” Upon EMS arrival, they gained quick rapport Contractions are coming every 2-3 minutes and are 60-90 seconds long The mother states she wants to push and feels her baby is coming right now EMS performed a visual exam Case Study #2 This is what you see. Now what do you do? If cord is wrapped around the neck, try to loosen and slip over the head. If too tight, need to double clamp and cut the cord NOW. Case Study #3 Mother calls EMS and states she is in labor Mother is G3P2 due tomorrow No known complications She has been in labor for 4 hours Contractions are 3 minutes apart EMS established rapport and performed a visual exam EMS determined that delivery is imminent Case Study #3 - This is a breech delivery that is not delivering. How do you handle this? Head should deliver in 30 seconds. If not, reach in to create an airway for the infant. Support body across your forearm. Creating an airway for a breech delivery Reach 2 fingers into the vagina Locate the infant’s face Push the vaginal skin away from the infant’s mouth Transport immediately Give report to the closest facility The crew member CANNOT move their fingers and risk losing the airway The golden sounds to a mother’s and EMS provider’s ears – a newborn’s cry!!! Documentation If the patient delivers, EMS and ED need to write 2 reports – one for the mother & one for the infant Both reports can have time of delivery On run report, OB delivery is credited to the person who delivers (“catches”) Segregate information Mother’s information on mother’s run report Infant’s information on the infant’s run report Documentation - Mother Due date (ie: EDC June 15th) Gravida/para (ie: G3P2) Presence of high risk concerns Bag of waters – Ruptured? Intact Status of contractions Signs of imminent delivery Crowning Bulging Urge to push Time of delivery (when last of baby delivers) & sex Complications during/after delivery (ie: bleeding) If placenta delivered or not Documentation - Infant Time of delivery Appearance of amniotic fluid (ie: clear, meconium staining) APGAR 1 and 5 minutes (ie: APGAR 9/9) Completion of assessment per physical condition boxes on run report Vital signs – B/P not necessary That cord was clamped and cut Time placenta delivered Special interventions required after delivery Wrist Bands Apply a wrist band to both the mother and the newborn Include the same information on both wrist bands Mother’s name Sex of infant Time of delivery Bibliography Bledsoe, B., Porter, R., Cherry, R. Essentials of Paramedic Care. 2nd Edition. Brady. 2007. Limmer, D., O’Keefe, M. Emergency Care 10th Edition. Brady. 2005. Region X SOP’s Effective March 1, 2007