Improving Quality of Hospital Care using Clinical Nurse Leaders
advertisement

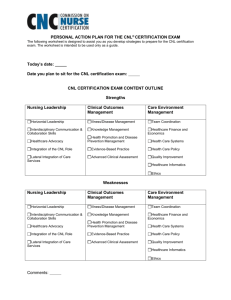
Improving Quality of Hospital Care using Clinical Nurse Leaders Grace Sotomayor, MBA, MSN, RN, FACHE, NEA-BC, CNL Chief Nurse Executive, Carolinas Medical Center Nov 02, 2012 Content • Background • Process • Goals • Current Deployment of CNLs • Results to Goals • Other Results • Questions CHS • >10.5m patient encounters /year in >800 care sites across the Carolinas • 2,800 Physicians and ACPs • Primary Care Network with 3m active patients • 60,000 employees Mission: To create and operate a comprehensive system to provide healthcare and related services, including education and research opportunities, for the benefit of the people it serves. Carolinas Medical Center CMC • 893 beds • Level 1 Trauma Academic teaching facility • Multiple Hallmarks designated units • Multiple TJC DSC designations • Council structure for Nursing Shared Governance since 2003 • Magnet submission entered Aug 01, 2012 CMC Nursing Practice Model 7 CNL • Masters prepared generalist nurse • Preparation Foci: • Practice is at the microsystems level • Client care outcomes are the measure of quality practice • Practice guidelines are based on evidence • Client centered practice is intra and interdisciplinary • Information will maximize self care and client decision making • Nursing assessment is the basis for theory and knowledge development • Good fiscal stewardship is a condition of quality care • Social justice is an essential nursing value • Communication technology will facilitate the continuity and comprehensiveness of care • The CNL must assume guardianship for the nursing profession CNL • Role areas • Clinician • Outcomes Manager • Client Advocate • Educator • Information Manager • Systems Analyst/Risk anticipator • Team Manager • Member of a profession • Lifelong learner • Programs in NC: UNC, Queens University Why CNL? • Linkage between education and outcomes • Performance on Nurse Sensitive Indicators critical for patient quality/safety and reimbursement • Nursing Leadership philosophy • Direct care nurses need to be well educated • Direct care nurses know best how to improve nursing care Implications for Nursing • IOM Report on Future of Nursing Implications for Nursing • IOM Report on Future of Nursing Implications for Nursing • IOM Report on Future of Nursing CNL Role Planning • 3 year Duke Endowment matching grant funds: 36 CNLs for adult Medical Surgical units at CMC • Partnered with Queens University, Charlotte for curriculum development • 38 credits • Created PCL course to jump start process • 2 days: Health Care Reform, Finance, Quality, Change Management, Case Management, CNL Role • PCLs take course at CMC in final year of school • Candidates selected carefully, must want to work in direct care PI Goals By Dec 2012: • Quality • Zero falls with injury • Zero HAPU • Cost • Turnover- annual rate 12% or less in med-surg units • Satisfaction • Inpatient satisfaction: overall Quality of Care 90th%ile • NDNQI RN Job satisfaction >60 Implementation • Information sessions for staff and managers • AACN White Paper on CNL role • Visited USF and Baycare: Morton Plant Mease • Attended annual CNL meetings co-sponsored by VA and AACN • Changed care delivery model on targeted units to be budget neutral • Implemented 8 hr /5 days/week model on day shift as “ Attending Nurse “ in ~ “12 bed hospital” • Partnered with Dartmouth for Micro system learning Budget Neutrality Key Points • Did not want role to be additive exposing it to potential deletion in the future • Work of CNL to be part of the nursing workflow at the bedside • The CNL is a direct care nurse with advanced skills • Assignments restructured by direct care staff on each unit to accommodate the CNL • Transitioned from Action OI as benchmarking vendor to Premier in 2011 14.00 12.00 11.45 10.86 10.77 10.00 10.26 10.14 9.93 10.03 9.71 9.59 9.73 9.08 Budgeted WHPPD 10.47 9.66 9.55 9.39 9.79 9.77 9.69 9T 11T 8.00 6.00 4.00 2.00 0.00 3T 4T 5T 2009 2010 2011 11A Current CNL Deployment Total 22 YTD 2012 • 3T 1 year • 4T 2 months 36 beds ; Full complement of 3 CNLs since August, 2012 • 5T 1 year • APC 2 years 13 beds ; Full complement of 2 CNLs since August, 2010. One CNL working in Women’s meso- system and one in HROB • 9T 1 year 36 beds ; Full complement of 3 CNLs since August, 2011 • 10A 0 36 beds. 3 PCLs • 10T 10 months 36 beds; 1 CNL on evening shift since January 2012; 1 CNL since Aug 2012; remainder 2 PCLs • 11A 1 year 24 beds; 2 CNLs since August, 2011; Full complement of 3 CNLs since August, 2012 • 11T 1 year 36 beds; 1 CNL since August, 2010; Full complement of 3 CNLs since December, 2011 36 beds; Full complement of 3 CNLs since August, 2011 36 beds ; 2 CNLs since December, 2011; Full complement of 3 CNLs since April 2012 CNL Process • Ensure EBP at bedside • Bedside report • Hourly rounding • Pain management • Teaching on the spot • Galvanize the inter professional team • 5P Assessment • Care planning • Physician rounding • Lean huddles • Lead PI • Teaching strategies, clinical care, Throughput • PI team participation e.g IPE, Transitions, ADOD Template for 5P Assessment The 5Ps: Purpose, Patients, Patterns, Processes , Professionals Results Falls/1000 Patient Days Falls/1000 Patient Days All CNL units CNL Only units Goal 7.00 6.00 5.63 5.48 5.76 5.08 4.91 4.99 4.36 5.00 N 4.32 4.22 3.84 4.00 4.08 3.58 3.00 2.19 2.47 2.8 2.00 1.00 0.00 1Q09 2Q09 3Q09 4Q09 1Q10 2Q10 3Q10 1st cohort graduated 4Q10 1Q11 2Q11 3Q11 2nd cohort graduated 4Q11 1Q12 2Q12 3Q12 3rd cohort graduated F a v o r a b l e Falls with Injury/1000 Patient Days 1st cohort graduated 2nd cohort graduated 3rd cohort graduated Hospital Acquired Pressure Ulcers Hospital Acquired Pressure Ulcers RN Turnover - 2009 All CNL Units Goal ≤12% by 2Q12 2009 Goal 30.0% 25.0% 20.0% 15.0% 10.0% 5.0% 0.0% 3T 4T 5T APC 9T 11A 11T 2009 4.7% 27.1% 18.6% 9.1% 15.1% 5.2% 22.3% Goal 12.0% 12.0% 12.0% 12.0% 12.0% 12.0% 12.0% 3 Units at or better than goal RN Turnover - 2010 All CNL Units Goal ≤12% by 2Q12 2010 Goal 30.0% 25.0% 20.0% 15.0% 10.0% 5.0% 0.0% 3T 4T 5T APC 9T 11A 11T 2010 11.7% 14.1% 10.4% 17.3% 11.7% 0.0% 4.8% Goal 12.0% 12.0% 12.0% 12.0% 12.0% 12.0% 12.0% 5 Units at or better than goal RN Turnover - 2011 All CNL Units Goal ≤12% by 2Q12 2011 Goal 30.0% 25.0% 20.0% 15.0% 10.0% 5.0% 0.0% 3T 4T 5T APC 9T 11A 11T 2011 13.0% 11.2% 16.3% 11.0% 10.0% 7.4% 4.5% Goal 12.0% 12.0% 12.0% 12.0% 12.0% 12.0% 12.0% 5 Units at or better than goal RN Turnover – 2QYTD Annualized All CNL Units Goal ≤12% by 2Q12 2QYTD12 Goal 30.0% 25.0% 20.0% 15.0% 10.0% 5.0% 0.0% 3T 4T 5T APC 9T 11A 11T 2QYTD12 12.8% 8.2% 3.8% 8.6% 0.0% 4.6% 4.2% Goal 12.0% 12.0% 12.0% 12.0% 12.0% 12.0% 12.0% 6 Units at or better than goal Patient Satisfaction 1st cohort graduated 2nd cohort graduated 3rd cohort graduated RN Job Satisfaction ( Enjoyment) Other Indicators Baseline Collected Pre-Canopy Implementation Data Source: Unit Admission/Discharge Log | Manually entered by Unit Secretary N=237 N=210 N=217 N=115 N=106 N=55 N=233 N=204 N=151 N=166 N=160 N=148 N=195 N=185 N=85 N=183 N=221 N=56 N=186 N=197 N=56 D/C to Home < 120 min of MD Order Baseline Collected Pre-Canopy Implementation Data Source: Unit Admission/Discharge Log | Manually entered by Unit Secretary N=237 N=210 N=217 N=115 N=106 N=55 N=233 N=204 N=151 N=166 N=160 N=148 N=195 N=185 N=85 N=183 N=221 N=56 N=186 N=197 N=56 D/C to Home before 12:00 Noon Next steps • Complete model on evenings and weekends • Ongoing education for CNLs: value based purchasing; performance improvement; micro system learning • Develop novice to expert competencies • Institute a CNL preceptor program • Institute a CNL Practice Council • Develop the CNL as coach The CNLs – second cohort pinning Questions?