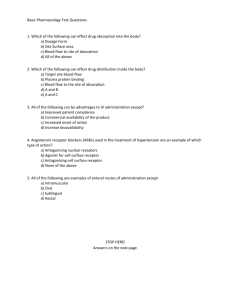
General principles, Administration of drugs, Drug Metabolism
advertisement
I. General principles of Pharmacology A. Pharmacology and its major areas • Pharmacology is the study of drugs. It takes into account their composition, uses, characteristics/propert ies, and effects. The subdivisions in pharmacology include: • 1. pharmacy: the science of preparing and dispensing medication • 2. toxicology: the study of the harmful effects of medications on living tissue • 3. neuropharmacology: the study of the effects of medication on nervous system and behavior functioning • 4. pharmacotherapeutics: the study of the use of drugs in treating disease • 5. pharmacokinetics: the study of the processes involving the absorption, distribution, metabolism and excretion of medications. • It is the study of what the body does to a drug. • 6. pharmacodynamics: the study of the actions of medications on living tissues. • It is the study of the biochemical and physiological effects of drugs, the mechanisms of drug action, and the relationship between drug concentration and effect. • Pharmacodynamics is the study of what a drug does to the body. Example: Clomiphene citrate • This drug induces ovulation B. Terminology related to effects of drugs • 1. therapeutic effect/indication: the intended effect of the drug; the uses of a drug • 2. contraindication: when the drug should not be used (see Warnings on label) example: celecoxib (Celebrex) • indication: relief of signs and symptoms of osteoarthritis; relief of signs and symptoms of rheumatoid arthritis example: celecoxib (Celebrex) • contraindicated in: hypersensitivity; history of allergic-type reactions to sulfonamides; history of asthma, urticaria (hives), or allergictype reactions to aspirin or other NSAIDs • 3. undesirable effects: These are effects of the drug, other than the therapeutic effect. • Undesirable effects may be further classified as side effects, adverse effects, toxic effects, or allergic reactions. • a. side effects: nuisance effects (dry mouth, altered taste, flatulence) • b. adverse effects: effects that may be harmful (diarrhea, vomiting) or effects that with prolonged treatment of the drug, may affect the function of vital organs such as the liver or kidneys • c. toxic effects: extremely harmful, life-threatening • A drug may cause all 3 undesirable effects: • example: rosuvastatin (Crestor) • side effects: headache and insomnia • • as well as constipation, flatulence, heartburn, altered taste, dyspepsia, and nausea • adverse effects: dizziness, diarrhea, druginduced hepatitis, elevated liver enzymes, pancreatitis • • toxic effects: rhabdomyolysis (release of muscle cell contents into the plasma) • From rosuvastatin • d. allergic reactions: this type of side effect has a different underlying cause compared to the previous types, it is due to the systemic release of histamine. • A hypersensitive person’s immune system identifies a foreign substance (antigen) and initiates a response (antibody). • The combination of antibody-antigen stimulates the histamine release. • This results in a range of symptoms, from mild (itching, swelling, redness, sneezing) to severe or life-threatening (bronchospasm, edema, shock, and death). • The severest symptoms are collectively referred to as anaphylaxis or anaphylactic shock. • 4. drug idiosyncrasy: Idiosyncrasy refers to a type of reaction that is not doserelated or allergic. • It occurs in a small percentage of patients given a drug. It is an individual’s unique response and may be related to genetics. • One example is cholinesterase deficiency, a condition where the effects of anesthetic agent, suxamethonium, are prolonged well beyond the usual few minutes, because the individual lacks the enzyme that normally limits its effects to a short time. • The patient’s muscles are paralyzed for longer than normal so assistance with breathing must be given for much longer than usual. • 5. LD50 • Before a drug receives approval for human use it must undergo several years of animal testing and evaluation. • One of the first tests that is performed is the lethal dose 50, (LD50) which is the dose that will kill 50% of the animals tested. • The results of this test are used to predict the safety of a drug. • Example: Tetrahydrocannibinol or THC • LD50 between approximately 50-86 g for a 68 kg (150 lb) person. • This would be equivalent to 1-1.8 kg of cannabis with a 5% THC content taken orally. • Example: batrachotoxins • These are extremely potent alkaloids found in certain species of frogs (poison dart frog) and beetles (Melyridae beetles) • The lethal dose of this alkaloid in humans is estimated to be 1 to 2 µg/kg. • For a 68 kg (150 pound) person this would be approximately equal to the weight of two grains of salt • Example: botulinum toxin • It is generally accepted as the most toxic substance known, with a median lethal dose of about 1 ng/kg, which means that a few hundred grams could theoretically kill every human on earth. C. Drug names • 3 basic types: chemical, generic, and trade • 1. chemical name: Each drug has only one chemical name, which is assigned using the nomenclature established by IUPAC and is based on the chemical structure. • Its name is usually long, very complicated, and impossible to remember. • 2. generic name: this is assigned by the U.S. Adopted Names Council, and is easier to remember. • 3. trade name: this is assigned by the pharmaceutical company which developed and markets the drug. This name is capitalized. • 4-Chloro-N-(2-furylmethyl)-5sulfamoylanthranilic acid • furosemide • Lasix • alpha'-[[(1,1-Dimethyl)amino]methyl]-4hydroxy-1,3-benzenedimethanol • albuterol • Proventil D. Drug classifications • A drug may be classified either by its therapeutic usefulness or how it works pharmacologically. • The pharmacological method generally addresses its mechanism of action and requires an understanding of biochemistry and physiology. Drug Pharmacological Therapeutic gentamicin Prevacid Atrovent Albuterol Propranolol Lotensin Diltiazem aminoglycoside proton pump inhibitor anticholinergic adrenergic beta blocker ACE inhibitor Ca2+ channel blocker anti-infective antiulcer agent bronchodilator bronchodilator antihypertensive antihypertensive antianginal Corgard beta blocker antianginal • Different drugs (i.e. Propranolol and Corgard) may have the same pharmacological actions but be prescribed for different therapeutic uses. • Different drugs (i.e. Atrovent and Albuterol) may have the same therapeutic use but different pharmacological actions. E. Enteral administration of drugs • Enteral refers to administration of a drug through a mucous membrane of the gastrointestinal tract (mouth to anus). • They include: oral, sublingual and rectal. 1. oral route • Administering a drug by mouth, in the form of tablets, capsules and liquids. • Advantages: it is generally the safest, most economical and most convenient route. • Disadvantages: • a). some drugs cause irritation of the gastric mucosa leading to nausea and vomiting • b). variable rates of absorption • c). effect may be too slow for emergencies • d). unable to use in unconscious patients • e). 1st pass metabolism: The majority of drugs absorbed from the GI tract enter the portal circulation. • They are transported to the liver before entering the general circulation. In the liver they may be metabolized, which might limit their efficacy. 2. sublingual • Administering a drug under the tongue. • Advantages: • this route avoids most of the disadvantages of oral administration, especially 1st pass metabolism • Disadvantages: • a. possible unpleasant taste • b. not all drugs can be administered by this route. • Examples of drugs administered sublingually: • nitrostat a compressed nitroglycerin tablet (a vasodilating agent) • buprenorphine, administered to opioid addicts (heroin, morphine) to ease the symptoms of withdrawal without producing euphoria (like methadone does). 3. rectal • Drugs administered rectally are usually in the form of suppositories, although some drugs may be in the form of liquids (enema). • Advantages: • a. may be used in unconscious or vomiting patients • b. it avoids 1st pass metabolism • Disadvantage: • irritation and inconvenience • Patient’s dislike this route of drug administration more than other routes. • Examples of drugs administered rectally: • Canasa, used to treat ulcerative colitis • compazine, an antiemetic • dilaudid, a hydrogenated ketone of morphine F. Parenteral administration of drugs • Parenteral means not in or through the digestive system. • The major routes are intravenous, intramuscular and subcutaneous. 1. intravenous • A needle is inserted directly into a vein and a solution containing the drug is given either in a single dose or by a continuous infusion. • Advantages: • a. drug tends to take effect more quickly as compared to other routes • b. more accurate in terms of dosage • c. can be used in an unconscious or vomiting patient • Disadvantages: • a. requires sterile preparations and aseptic procedures • b. generally patients cannot administer it to themselves • c. it is more difficult to administer • d. One of the greatest disadvantages relates to the speed of its pharmacologic action, an overdose can not be withdrawn nor absorption stopped. • Examples of drugs administered IV: • dopamine, to improve blood pressure, cardiac output in treatment of shock unresponsive to fluid replacement • heparin, in the treatment of various thromboembolic disorders 2. subcutaneous • Here a needle is inserted into fatty tissue beneath the skin. • The drug is injected then moves into either the capillaries or the lymphatic vessels and enters the bloodstream. • This route is used for many protein drugs which would be degraded in the digestive tract if given orally. • Examples of drugs administered subcutaneous: • Insulin, in the treatment of type 1 diabetes • Goserelin, used to treat hormone-sensitive cancers of the prostate and breast as well as certain benign disorders (endometriosis, uterine fibroids). • All live injected vaccines (MMR, varicella, and yellow fever) are recommended to be given subcutaneously. 3. intramuscular • The intramuscular route is preferred over the subcutaneous when larger volumes of the drug are needed. • A longer needle is required since the muscle lies below the skin and fatty tissues. • Drugs are injected into muscle in the upper arm, thigh, or buttocks. • Tetanus, diphtheria, and acellular pertussis booster vaccine (Tdap) to protect against infections caused by tetanus (lockjaw), diphtheria, and pertussis (whooping cough). • Streptomycin, in combination with other agents in the management of active TB • Haloperidol in the treatment of acute and chronic psychotic disorders including schizophrenia, manic states or drug induced psychoses G. Skin and mucuous membrane administration of drugs • The major routes here are topical, transdermal and respiratory tract 1. topical • This route of administration usually involves applying drugs to the skin or membranous linings of the ear, eye, or nose. • These drugs tend to produce a local effect. • Examples include: • Antibiotic creams to treat skin infections: Neosporin and Polysporin • Hand sanitizers • Calamine lotion for itching of poison ivy, • benzocaine to relieve sunburn pain. 2. transdermal absorption • Here absorption from the skin produces a systemic rather than local effect. • Examples: Fentanyl patches for pain therapy • hormone replacement therapy (for menopausal symptoms) 3. Respiratory tract • The respiratory tract provides an extensive absorbing surface and blood supply. • There is good absorption for sprays, aerosols and gases. • The size of the particles is of great importance. • Generally particles greater then 10 microns are deposited in nasal passages, less than 2 microns penetrate deeper (for significant penetration to the alveoli, 2 microns or less). • a. intranasal: Once absorbed the drug enters the bloodstream. • Advantage: • Drugs taken by this route generally work quickly. • Disadvantage: • They may be irritating to the nasal passages • Examples include calcitonin (for osteoporosis), neosynephrine (for congestion) • b. inhalation: Once absorbed into the lungs it enters the bloodstream. • Example: dihydroergotamine (migraines), corticosteroids (allergies, asthma) • inhaled cyclosporine, the first drug ever to show a decline in the incidence of chronic rejection which is the leading cause of death following a lung transplant H. Pharmacokinetics • Pharmacokinetics is what the body does to a drug. • It involves 4 processes: absorption, distribution, metabolism, and excretion 1. Dissolution/absorption • Absorption is the movement of the drug from the site of administration into the bloodstream (or lymphatic system) • Drugs given orally dissolve in body fluids (saliva, gastric juice) and are absorbed through the tissues of the stomach and small intestines into the blood vessels Medications administered orally • a. food in the stomach • One of the factors which affects drug dissolution is the presence of food in the stomach. • The presence of food in the stomach, especially a high fat meal will delay gastric emptying, which could slow down the dissolution of the drug. • In addition, the presence of food stimulates the secretion of both enzymes and HCl • (the protein drug insulin cannot be administered orally because enzymes “digest it”) • Nutrients in food may compete with drugs for carrier molecules (Levodopa for Parkinson’s is transported using the same carriers as the amino acids leucine and isoleucine, so it should be taken on an empty stomach). • Phytochemicals in fiber (i.e phytates) may bind to medications and decrease their absorption • Tricyclic antidepressants (i.e. Elavil) and digoxin shouldn’t be consumed with high fiber foods containing wheat bran. • Other drugs, known to cause gastric distress, such as Erythromycin and Augmentin should be taken with food to alleviate the GI distress. • b. pH • Another factor which plays a role in drug dissolution is pH. • Dissolution of ketoconazole, used to treat Candida infections is impaired if the medium of the stomach is not acidic enough. • c. Interactions between medications and dietary supplements • vitamins and/or minerals interactions with medications may either increase or decrease absorption. • Iron supplements are better absorbed if taken with citrus juices. • Certain drugs are chelated to minerals, for example, Ca2+ supplements will chelate tetracycline and levothyroxine making these drugs unabsorbable. • d. disease states • Diseases that change the surface area for nutrient absorption will also affect drug absorption (Crohn’s disease). medications administered rectally or vaginally • Following rectal or vaginal administration, a suppository melts and releases the drug to the mucous membranes. • The rate of absorption with rectal administration is rather slow and variable. medications administered topically • Topical drugs are not absorbed to any great extent, their therapeutic action is exerted locally at the site of administration. medications administered through the respiratory tract • Following administration of drugs by inhalation, the vaporized liquid is absorbed thru the mucous membranes lining the alveoli and into adjacent capillaries • Some drugs administered this way produce a systemic effect (general anesthetic gases) others, a topical effect medications administered intravenously • Only IV injections bypass the step of absorption as the drug is administered directly into the blood stream. • Subcutaneous and intramuscular injections of liquid drugs are absorbed from body tissues into adjacent blood vessels • So, with the exception of the IV (or intraarterial) route, drugs must pass thru mucous membranes before gaining access to the bloodstream. • These membranes consist of a layer of epithelial cells that are closely connected together. • Molecules must traverse at least 2 cell membranes (apical side and basal side) • These membranes are composed of lipid and protein, forming a semipermeable barrier Crossing membranes • The mechanisms by which drugs cross membranes are the same as those for nutrients: • passive diffusion • facilitated diffusion • active transport • Two of the most important chemical properties of medications related to drug absorption include the solubility of the drug in lipid or water and the degree of ionization • Cell membranes are mostly lipid, so the more lipid-soluble a drug is, the faster it will pass through the membrane • With the exception of general anesthetics, most drugs are water soluble and only partially lipid soluble. • Drugs are usually weak acids or weak bases whose absorption is influenced by their degree of ionization in body fluids • Most drugs exist in 2 forms: ionized and not ionized. In general, drugs that are not ionized will be absorbed more readily • If the drug is ionized, absorption will be slower Example: acidic drug • If a drug is mildly acidic, absorption will be enhanced in solutions that are also acidic, because the drug will not be ionized in these solutions. • Aspirin (acetylsalicylic acid) is generally not ionized in the stomach (pH of gastric juice ranges 1-3). So its absorption here is favored. • In the small intestines (pH range 7-8), acidic drugs are mostly ionized, absorption is slower and occurs to a lesser extent Example: basic drug • Basic drugs (streptomycin, morphine) are mostly ionized in the stomach, and are absorbed more slowly and to a lesser extent here. • Basic drugs are not ionized in the intestines and are more readily absorbed here. 2. Distribution of drugs • After absorption, distribution on the drug occurs. It is the movement of the drug to various tissues of the body. • There are a number of factors which determine how much drug reaches any one organ or area of the body: a. plasma protein binding • As a drug enters the bloodstream, some of it binds to circulating plasma proteins. • Acidic drugs commonly bind to albumin, while basic drugs often bind to glycoproteins and lipoproteins. • Many endogenous substances, such as steroids, vitamins, and metal ions are bound to globulins. • Bound drugs are pharmacologically inactive as they are carried thru bloodstream. • As unbound drug moves from blood into body tissues to exert therapeutic effect, some of the bound drug is released from plasma protein to maintain equilibrium. • The ratio of bound to unbound drug varies with the drug, some are highly bound (99%), others are not bound to any significant degree: • caffeine is about 10% bound • Digoxin is about 23% bound • Warfarin is about 99.9% bound • Various disease states can affect drug distribution. Specifically, liver disease may alter the amount of albumin. • This increases the amount of unbound drug, which increases the concentration of active drug within the body. • Low albumin tends to be more common in older patients and may lead to excessive anticoagulation and bleeding in those on Warfarin. b. changes in circulation • Physical activity and an increase in body temperature will increase vasodilation and theoretically increase the distribution of a drug c. body size and composition • Obese individuals may accumulate fat soluble drugs (BZ’s like valium) d. blood-brain barrier • This is an additional lipid barrier that protects the brain by restricting the passage of electrolytes and other H2O soluble substances (dopamine). • Many lipid soluble drugs, such as L-dopa, pass readily into the brain 3. Metabolism • a. 1st pass metabolism • Metabolism is the total of all chemical reactions in the body • It occurs in almost every cell and organ, but the liver is the primary site • Drugs absorbed thru mucous membranes of stomach or intestines are carried to the liver via the portal vein • Here the drug is subjected to metabolism by liver enzymes before it enters into the general circulation (this is called 1st pass metabolism) • The liver may actually metabolize the drug to a less active form before it is distributed to rest of body (including the target organ/tissue) • For some drugs, the 1st pass effect is so extensive that most of the drug dose is immediately metabolized b. biotransformation • Once a drug has produced its intended therapeutic effect it needs to be eliminated from the body. • Biotransformation is the chemical alteration of drugs and other foreign compounds (xenobiotics) in the body • Biotransformation enzyme systems originated in ancient bacteria at least a billion years ago, • due to the hostile environment they had to endure (extremes in temperature, lack of oxygen, corrosive chemicals). • These specialized heme-containing enzymes are called cytochrome P450, or CYP450, so named because they absorb UV light at 450 nm. • As of 7/2007 over 7,000 CYP450’s have been identified. The very large number necessitates a classification system (that is based on similarity in amino acid sequences). • The initial division is into families, designated by the prefix CYP followed by a number, i.e. CYP1, CYP2. There are over 70 of these families, but only 17 of them in humans. • The next division is into subfamilies which are identified using a capital letter, i.e. CYP1A, CYP1B. • The final division is into individual members of each subfamily (called isoforms) which originate from a single gene, i.e. CYP1A1, CYP1A2 All CYP450’s have a number of features in common: • They contain a heme group, therefore their reactions with various substrates are iron catalyzed. • They are associated with membranes, which are primarily lipid in composition. • They can bind oxygen. • They can undergo reactions (reduction) that don’t require oxygen. • CYP450’s are found in all tissues, but the liver and GI tract have the highest concentration which process and eliminate large amounts of both endogenous and exogenous chemicals. • The overall aim of biotransformation is to clear drugs and other chemicals from the organism. Generally, biotransformation occurs in 2 stages: phase I and phase II. • Phase I are oxidative reactions which insert an oxygen molecule to form an alcohol: • hydrocarbon—H + O2 + 2e’s + 2H1+ → • hydrocarbon—OH + H2O • This alcohol may now be water soluble enough so that it is eliminated without further metabolism. If not, it undergoes conjugation with another water soluble group in Phase II. • In Phase II, a molecule destined for elimination, either an endogenous or exogenous substance, is attached to a water soluble group , i.e. sulfates, glucuronic acid, amino acids, acetate, and glutathione c. consequences of Phase I and Phase II reactions • What are the overall consequences of these Phase I and Phase II reactions on exogenous compounds? i. Inactivation of a drug • The active form of a drug is converted to an inactive form. This is necessary so that once it has performed its therapeutic job, it is eliminated • Without this reaction, it is estimated that the barbiturate phenobarbital would circulate for years • This, however, is what happens to a proportion of many drugs during their “1st pass” through the liver. ii. Activation of the compound • Many drugs are biologically inactive until metabolized by a cytochrome P450 • Codeine is activated by a cytochrome P450 to morphine iii. formation of a toxic metabolite • This is obviously, not a desired effect, but nonetheless, it happens. • example: Benzo[a]pyrene is produced in tobacco smoke, in charcoal grilled foods, from burning coal, and in pollution (resulting from various industrial processes). • It is metabolized by a cytochrome P450 to a potent carcinogen which forms guanine adducts on DNA . This may disrupt gene function leading to mutations • example: acetaminophen • There are 3 major routes by which this is metabolized, 2 of the 3 involve Phase II reactions which produce polar, inactive metabolites that are readily excreted • A small amount is metabolized by a cytochrome P450 to a highly reactive metabolite NAPQI (N-acetyl-p-benzoquinone imine). This is usually not a problem when normal doses of acetaminophen are taken. • Large quantities of acetaminophen cause an increase in the production of NAPQI which can cause liver damage • In addition, consumption of alcohol induces a cytochrome P450 , which increases the production of NAPQI. • The extent of liver damage depends on the timing and amount of acetaminophen taken. • 41 year old white female with a diagnosis of Tylenol overdose with liver failure • 35% of cases involving liver failure are caused by acetaminophen poisoning, according to the American Liver Foundation d. Factors which affect drug metabolism: • The cytochrome P-450 system is under genetic control and is highly sensitive to induction (stimulation) or inhibition by many factors (i.e., other drugs, insecticides, herbicides, smoking, caffeine, phytochemicals). i. age • A major factor in the metabolism of drugs is age. The very young and the elderly both have a decreased ability to metabolize drugs due to different levels of liver functioning. Children have smaller livers and less circulation within the liver. ii. genetics • Genetics also plays a role, especially when one considers the phenotypic differences of metabolic enzymes. This has been seen in various proton pump inhibitors which may affect the treatment for H. pylori infections. iii. naturally occurring ingredients in foods Pressor agents • Biologically active amines, or pressor agents are commonly found in many foods. • These pressor agents include tyramine, dopamine, histamine, and phenylethylamine. Foods that contain these agents include: • aged cheeses (bleus, Stiltons, cheddars, gorgonzolas), aged meats (salami, sausages), soy sauce, fermented soy beans or paste, tofu, miso soup, fava beans, snowpea pods, saurkraut, Korean beers and red wines (especially Chianti). • The pressor agents in these foods do not normally present a problem because they are rapidly deaminated by MAO (monoamine oxidase) and diamine oxidases. • One class of antidepressants is known as MAO inhibitors. Patients on these drugs should not eat foods that are high in these pressor agents, as they are not broken down. • Tyramine, in particular, is a vasoconstrictor, and can lead to a hypertensive crisis (increased blood pressure, increased heart rate, headache, stroke, sometimes death). CYP inhibitors • Grapefruit inhibits CYP 3A4 which results in increase in the concentration of many drugs in the circulation, and possible toxicity. • The effects of grapefruit on this enzyme can last up to 72 hours (until the body can make more of the enzyme). • Drugs affected include the statins, some cardiac drugs (antiarrhythmic amiodarone). iv. dietary supplements • St John’s Wort is a supplement used for depression. It is a perennial whose medicinal uses were first recorded in ancient Greece. • Preliminary studies suggest that St. John's wort might work by preventing nerve cells in the brain from reabsorbing the chemical messenger serotonin. • In Europe, St. John's wort is widely prescribed for depression. In the United States, it is one of the most commonly used herbal supplements. • Scientific evidence regarding the effectiveness of St. John's wort for depression is inconsistent. • An analysis of the results of 37 clinical trials concluded that St. John's wort may have only minimal beneficial effects on major depression. • However, the analysis also found that St. John's wort may benefit people with minor depression; these benefits may be similar to those from standard antidepressants. • Research has shown that taking St. John's wort results in an induction of CYP 3A4 which can limit the effectiveness of some prescription medicines, including: • antidepressant medicines, birth control pills, cyclosporine, digoxin, and warfarin. 4. Excretion • Drugs and their metabolites are eliminated from the body by a number of different routes • The kidneys are the major organs of excretion. • A drug that remains bound to albumin is too large to pass thru the glomerular membrane in the nephron and is returned to the general circulation • Unbound drug is small enough to pass through the glomerular membrane. • Once through, distinction is made between water-soluble and fat-soluble drugs • Unbound water-soluble drug is excreted in the urine • Unbound fat-soluble drug is attracted to lipid in membrane of renal tubule wall , is reabsorbed into the renal tubules and returned to the bloodstream. • • Eventually it is metabolized by liver into a water-soluble form • Without the liver’s action, it is difficult for a fat-soluble drug to be excreted by kidneys. • The respiratory system doesn’t generally play a large role in drug excretion. • An exception would be general anesthetic gases which are not totally metabolized and are excreted primarily by lungs • Trace amounts of drugs are excreted in breast milk • May be insignificant compared with total amount excreted by kidneys, but can be enough of a dose to significantly affect a nursing baby • The rate of elimination refers to the amount of drug removed per unit of time from the body by normal physiological processes • It is an indicator of how long a drug will produce its effect • Half life, t1/2, is the length of time required for a drug’s concentration in the plasma to decrease by ½. • The larger the ½ life, the longer it takes to eliminate the drug • Drugs with longer ½ lives may be given less frequently • With renal or hepatic disease, the ½ life of a drug increases • • • • • ½ life of: minutes (nitroglycerin 1- 4 min) several hours (metformin 17.6 hours) days (corticosteroids) years (Fosamax 10 yr) I. Pharmacodynamics A. Introduction • Pharmacodynamics is the mechanism of drug action • The receptor is the part of the cell that interacts with a drug, and by binding with it, initiates a specific biochemical chain of events. • Membrane Receptor embedded in membrane • A drug that is able to activate a receptor and produce an effect is called an agonist. • When present, agonists cause the tissue to respond, resulting in a therapeutic effect. • Some drugs appear to fit a certain receptor, but cannot activate the receptor to produce an effect. • These drugs are known as antagonists or blockers. • They inhibit or block the binding of body chemicals or drugs from activating the receptor (similar to inserting the wrong key into a lock). B. Mechanisms of receptor actions • There are, generally, 3 major mechanisms of receptor interractions. 1. binding to intracellular receptors • A lipid soluble drug diffuses across a cell membrane and binds to an intracellular receptor. • Drugs in this class include steroid hormones, thyroid hormones, and corticosteroids. Example: Corticosteroids • Corticosteroids are taken into a target cell and then enter the nucleus. • Once inside the nucleus, they bind to HRE’s (Hormone Response Elements) and either induce or inhibit the activity of specific genes. • These genes control the synthesis of various proteins, many of which are enzymes. • Corticosteroids are involved in the control of the inflammatory response. • They induce the synthesis of an inhibitory protein called lipocortin. • It is lipocortin that inhibits the activity of the enzyme phospholipase A2 • This enzyme normally causes the release of arachidonic acid from phospholipids in cell membranes. • Arachidonic acid is the precursor of the prostaglandins and leukotrienes, powerful inflammatory agents. • Therefore, corticosteroids have the ability to suppress the inflammatory response. 2. Secondary messengers: Activation of a system on the cytoplasmic side of the membrane • A drug binds to a receptor and triggers a cascade of reactions on the cytoplasmic side of the membrane, leading to chemical changes within the cell. • There are 2 major secondary messenger systems. • The adenylate cyclase system which, through the hydrolysis of ATP, leads to an increase in cAMP. • This results in either the activation or inhibition of a protein kinase, ultimately leading to some specific biochemical activity. • Examples of drugs and endogenous molecules which activate protein kinases include: a number of different growth factors, atrial natriuretic peptide, and insulin. Example: insulin • Examples of drugs which inhibit protein kinases include: gefitinib and erlotinib. • These drugs are tyrosine kinase inhibitors (TKI). • They block cell growth and division and are used in various cancer treatments. • The phosphatidylinositol/Ca2+ system involves the hydrolysis of a membrane phospholipid into a diacylglycerol (DAG) and inositol-1,4,5-triphosphate (IP3). • This leads to the release of intracellular Ca2+ from storage vesicles. • When the intracellular concentration of Ca2+ increases, there is an increase in the activity of various calcium-dependent protein kinases, which again leads to some specific biochemical reaction. • Example: Lithium, in the treatment of manic-depressive disorder. 3. Affect a membrane channel • A drug binds to a receptor which controls a membrane channel. • The drug either mimics or blocks the actions of some endogenous compound. • These endogenous compounds include acetylcholine, serotonin, • GABA and glutamate. Example: • The binding of the neurotransmitter acetylcholine will open channels that allow the passage of Na1+, and initiate either a nerve impulse or muscle contraction. • Dicyclomine is an antispasmodic anticholinergic used sometimes in the treatment of Irritable Bowel Syndrome (IBS) • By preventing the binding of acetylcholine, this antispasmodic medication decreases muscle contractions C. Types of receptors • There are many types of receptors throughout the body. Three types are commonly involved in drug therapy: adrenergic, cholinergic, and histaminic. 1. adrenergic receptors • Adrenergic receptors are part of the sympathetic nervous system. • They are activated by the natural neurotransmitters epinephrine, norepinephrine and dopamine; • as well as by many different drugs (i.e. clonidine, dobutamine, albuterol). • In addition, there are many drugs which are adrenergic receptor antagonists. They block adrenergic receptors (i.e. prazosin, atenolol) 2. Cholinergic receptors • Cholinergic receptors are part of the parasympathetic nervous system and are activated by the natural neurotransmitter acetylcholine; • as well as by many different drugs (i.e. pilocarpine and neostigmine). • In addition, there are many drugs which are cholinergic receptor antagonists. These block cholinergic receptors (i.e. scopolamine, atropine) 3. Histaminic receptors • Histaminic receptors are activated by histamine. • Pharmacologically, this is not a desired effect. • There are a number of antihistamines, both 1st and 2nd generation (i.e. Benadryl, Claritin) .