Why do we sleep?
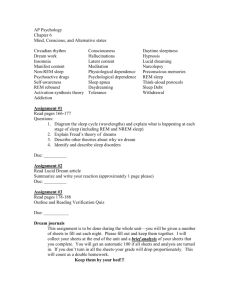
advertisement

dolphins whales sperm whale (off the coast of Chilé) http://www.nature.com/news/2008/080221/ multimedia/news.2008.613.mov 135,000 hours of your life asleep (1/3) How do we study sleep? What do we know about it? What are some sleep disorders What do we know about brain regions and neurotransmitters involved in sleep? typically in a sleep lab…. EEG – electroencephalogram EPSPs of cortical neurons ◦ EMG – electromyelogram looking at muscle tone (usually electrodes on jaw) ◦ EOG – electrooculogram looking at eye movements (electrodes around eye) look at 2 components of the EEG 1. the frequency of the wave (n of peaks/unit time) – tells you about the number of cortical neurons generating EPSPs 2. the amplitude of the wave (height of wave) – – tells us about the n of EPSPs that occur at the same point in time n of neurons firing in synchrony high frequency, low amplitude beta waves start seeing higher amplitude, lower frequency alpha waves 1st sleep stage – still fairly high frequency low amplitude but clear difference from alert and awake state often will deny being asleep 15 min later (if not disturbed) stage 2 – characterized by high frequency low amplitude sleep spindles and high amp low f k complexes role of these wave forms?– 15 min later if not disturbed stage 3 – first of the slow wave sleep stages characterized by delta waves high amplitude, low frequency waves less than 50% delta waves is stage 3; more than 50% stage 4 (15 min later) during SWS, parasympathetic NS activity seems to predominate (hr and bp decrease, respiration decreases, gastric motility increases) person relaxed but still motor activity; normal sleeper changes position every 20 min or so stage 4 deepest stage ? typical 90 min sleep cycles goes from ◦ stage 1 (15 min) to stage 2 (15 min) to stage 3 (15 min) to stage 4 (15 min) to stage 3 (15 min) to stage 2 (15 min) to first bout of REM sleep low amplitude, high frequency desynchronous EEG low amplitude, high frequency desynchronous EEG rapid eye movement (REM) narrative dreams muscle atonia ◦ look at motor cortex – extremely active but descending motor pathways paralyzed ◦ REM without atonia penile erections and vaginal secretions deepest stage? ◦ incorporate things into our dreams ◦ more likely to spontaneously awaken changes in amount of time spent in REM over the night changes in amount of time spent in REM over the night maturational changes in pattern ◦ species with underdeveloped CNS – spend more time in REM changes in amount of time spent in REM over the night maturational changes in pattern ◦ species with underdeveloped CNS – spend more time in REM ◦ human newborns ~ 50% sleep time in REM ◦ human premies ~ 80% sleep time in REM evolutionary theory ◦ predictions…… restoration and repair Sleep more if: ◦ No predators ◦ Safe place for sleeping ◦ Dangerous to yourself in the dark Sleep less if: ◦ Fear of predation ◦ Food of low nutritional value evolutionary theory restoration and repair ◦ marathon runner studies 1. Insomnia 1. Insomnia - primary cause - sleep medications 1. Insomnia - primary cause - sleep medications - develop tolerance; REM rebound short-acting benzodiazepenes ◦ triazolam (Halcion®) short-acting benzodiazepenes ◦ triazolam (Halcion®) problems with BZ tolerance REM suppression (and REM rebound) WD Zolpidem- (Ambien) ◦ ◦ ◦ ◦ non hypnotic sedative Also a muscle relaxant and anticonvulsant Still works on GABA A receptors Works quickly (15 min) and with a short ½ life (how quickly it clears out of the body releases hormone melatonin at night Ramelteon (Rozerem) ◦ ◦ ◦ ◦ First in a new class of sleep medications non BZ non sedative melatonin agonist 1. Insomnia - primary cause - sleep medications - develop tolerance; REM rebound - we are often poor estimators of how much sleep we get -sleep apnea – difficulty sleeping and breathing at the same time -two types - 1. CNS mediated – very rare - 2. obstructive sleep apnea- main cause weight loss, reducing alcohol consumption (or other muscle relaxants), elevated sleeping, CPAP machine – continuous postive airway pressure surgical procedures to remove or tighten tissue SIDS – sudden infant death syndrome ◦ possible link Nocturnal myoclonus – twitching of the body, usually the legs, during sleep – most are not aware of why they don’t feel rested (now called periodic limb movement disorder); involuntary Restless legs – sufferers complain of legs being uncomfortable that prevents sleep- can occur when awake or asleep Txt can include DA agonists; anticonvulsants Copyright © 2006 by Allyn and Bacon ~ 250,000 people in US ◦ symptoms: uncontrollable recurring sleep during daytime (usually during mundane tasks) ◦ subcategories cataplexy hypnagogic hallucinations REM sleep behavior disorder often (not always) older males often (not always) associated with other neurodegenerative diseases brainstem structures – pons, medulla abnormalities in noradrenergic, cholinergic, and serotonergic systems, seems to exist in the pathogenesis of RBD clonazepam (Klonopin) ◦ anticonvulsant – ◦ benzodiazpene unusual sleep characteristics ◦ short latency to REM ◦ persistent muscle tone ◦ excessive muscle twitching Treatment for narcolepsy ◦ stimulants; caffeine, ◦ GHB – gamma hydroxy butyrate** genetics of narcolepsy ◦ people with family history + are 50X more likely to have disorder than families without history + ◦ animal species Non-REM sleep disorders ◦ Enuresis ◦ Sleep walking locus coerulus- in hindbrain (NE transmitter) ◦ important for arousal What does it do during sleep? locus coerulus- in hindbrain (NE transmitter) ◦ important for arousal What does it do during sleep? ◦ active when awake; inhibited during sleep – particularly REM Acetylcholine – in pons – important for REM onset ◦ AChE poisoning (mustard gas or pesticides) people go into REM immediately after falling asleepvery vivid dreams and nightmares! PGO waves – Increases in tryptophan – increases in 5HT Increases in 5HT – increases in drowsiness (?)