What is Meaningful Use?
advertisement

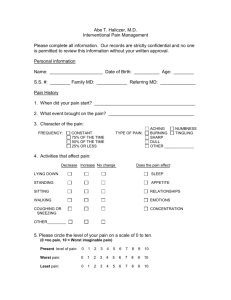
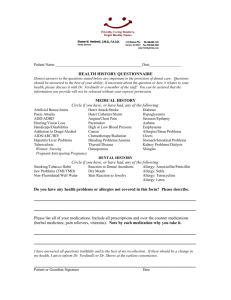
Preparing for Maestro Care This module is designed to provide information for staff regarding interviewing a patient for historical information and to introduce the concept of meaningful use. Please review the module and complete the test at the end. You will receive credit for completion after you complete the module and the test. Objective for This Module: At the end of this section, the participant will be able to update the patient history and understand the importance of meaningful use questions A health history is a systematic collection of subjective data that is stated by the client and objective data which is observed by the nurse There are two phases to history taking: The interview phase The recording phase Ensure a quiet, private and comfortable environment Orient the patient to the structure of the history taking process Communicate priorities for the patient Listen more than talk Be aware of non-verbal communications Remember to utilize effective communication patterns and customer service techniques when interacting with patients Begin by reviewing information about past health history before starting on new health history The interview process will be structured and quick You might begin the interview process by stating, “I am going to review your medical history by naming a list of conditions and asking you to respond ‘yes’ or ‘no’ as to whether any of these are part of your medical history” Make sure to clarify any terms or descriptions that you are unsure of! There are mainly two types of history: Complete health history which is taken on the initial visit to a health care provider Interval history which is taken in following visits The “chief complaint” is also an important part of history collection The chief complaint is the reason for the visit ▪ Examples include: ▪ Chest pain for three days ▪ Swollen ankles for 2 weeks ▪ Fever and headache for 24 hours The history of present illness is important information for the provider This information is relevant to the chief complaint and the client’s problem It includes essential relevant data and self medical treatment Information to include in the history of present illness: Client’s summary and usual health Investigation of symptoms: onset, date, gradual or sudden, duration, frequency, location, quality, and alleviating or aggravating factors Negative information (no bleeding, etc.) Relevant family information (if others have similar symptoms) Disability, or how this affects the patients life The purpose of a past health history is to identify all major past health problems of the client The includes Childhood illness (i.e., history of rheumatic fever) History of accidents and disabling injuries History of hospitalization ( to include date, admitting complaint, discharge diagnosis, follow-up care) History of surgeries including reason for each surgery History of immunizations and allergies Physical examinations and diagnostic tests Examples of important information obtained from family history include: History of communicable disease Heredity factors that are associated with certain disease Strong family history to certain problems General health of family members including parents, siblings, aunts, uncles and other family Cause of death of immediate and extended family The purpose is to record major, current, health-related information Habits such as alcohol, drug or caffeine Medications taken regularly prescribed by the doctor or over-the- counter Exercise patterns Sleep patterns Sexual activity and birth control The psychosocial history includes: How the client and his family cope with disease or stress and how they respond to illness How any psychological or social problem affects the general health of the client A review of systems (ROS) is a collection of information about the past and present of the client’s major systems It is a review of the client’s physical, sociologic and psychological health status and may identify hidden problems Meaningful use is the implementation of an electronic health record in such a way as to improve the quality and safety of the nation’s health. There are five health-enhancing goals: Improve the quality, safety, and efficiency of care while reducing disparities; Engage patients and families in their care; Promote public and population health; Improve care coordination; Promote the privacy and security of patient information. Within our new electronic health record we are meeting meaningful use requirements by incorporating additional assessment parameters or health questions into our interviewing and intake process Examples include: ▪ ▪ ▪ ▪ ▪ ▪ ▪ ▪ ▪ Collecting and documenting height, weight and blood pressure Asking tobacco cessation questions Asking if a patient is taking hypertensive or diabetes medications Asking if patients have had the flu shot or pneumonia vaccine Asking if patients have been screened for colon cancer, had a pap smear or mammogram Following service specific quality measures Verifying and updating allergies Completing a medication review and update Printing a After Visit Summary (AVS) Height and weight are important patient parameters to follow. They can be used to determine the Body Mass Index (BMI) for patients. This meaningful use question will prompt us to obtain or ask for patient height and weight to determine BMI so that an plan can be documented in patients over the age of 18 years of age for elevated BMI results. Tobacco and nicotine use can be addictive Tobacco contains 19 known cancer causing agents Patients will be asked if they smoke so that counseling can be completed if patients are smoking. Patients will now be asked if they are on hypertension medications if they are aged 18 years and over. We will be looking at these patients closely to see if their hypertension is being controlled. Patients will also be asked if they are taking medications for diabetes. We will be looking at patients aged 1875 years who are type 1 or type 2 diabetics to see if their blood pressure is less than 140/90. Patients who are over 50 or high risk will now be asked if they have received the flu shot Patients over 65 years of age or who are high risk will be asked if they have had the pneumonia vaccine All patients over age 50 will be asked if they have been screened for colon cancer All women over age 21 will be asked if they have had a pap smear All woman over the age of 40 will asked if they have had a mammogram Allergy information is very important to document in Maestro Care. An allergy is a hypersensitivity of the immune system Patients should be asked their allergies at each visit Maestro Care also allows for the entry of intolerances. For example, a patient may avoid a certain medication because of stomach upset. It may not be an allergy but an intolerance Service specific quality measures have been determined for each subspecialty and will be asked during the interview. The elements of a patient history are vital information needed to care for our complex patient population The way an interview is structured is imperative to accurate and concise results Meaningful use is another way to improve the quality and safety of our patients Proceed to the quiz on the next slide. PROPERTIES On passing, 'Finish' button: On failing, 'Finish' button: Allow user to leave quiz: User may view slides after quiz: User may attempt quiz: Goes to Next Slide Goes to Next Slide After user has completed quiz At any time Unlimited times Blumenthal, D., & Tavenner, M. (2010). The “meaningful use” regulation for electronic health records. The New England Journal of Medicine, 363, 501-504. Nursing Health Assessments, Chapter 3, Health History You have successfully completed this module. Please proceed to the next module.