“A Cup of Holiday Cheer?” Pre-hospital Alcohol
advertisement

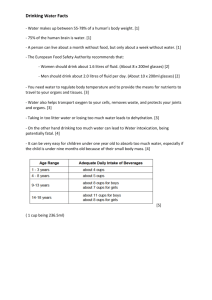
“A Cup of Holiday Cheer?” Pre-hospital Alcohol Emergencies Presence Regional EMS December 2015 Objectives Discuss the effects of ethyl alcohol on the human body Describe delirium tremens, signs and symptoms, complications and management Outline physiological concerns specific to children ingesting ethyl alcohol. List other emergency situations that might be masked by alcohol intoxication Using a variety of scenarios discuss the assessment and management of alcohol related emergencies Alcohol and EMS Patients The common alcohol encountered in patient interactions is Ethanol Alcohol is the most common substance of abuse in the US and worldwide 75% of Americans have at least one alcoholic drink per year. Between 15% and 40% of EMS patients have detectable levels of alcohol in their blood. Alcohol and the Holiday Season In American society, drinking alcohol is a tradition during the Holiday Season. Actions of Alcohol on the Body At low doses: excitatory and stimulating effects with depressing of inhibitions Aggressive behavior Inappropriate behavior At higher doses: sedative effect, depresses the central nervous system Dulls sense of awareness Slows reflexes, lack of coordination Reduces reaction time Stupor and coma Physiology Alcohol is completely absorbed from the GI tract in 30-120 minutes. Food in the GI tract slows absorption time Concentrations in the brain rapidly approach blood alcohol levels Alcohol is broken down and eliminated (metabolized) by the liver Intoxication occurs when alcohol enters the bloodstream faster than the liver can break it down Alcohol causes peripheral vasodilation Flushing of skin Feeling warm Increased loss of body heat Alcohol potentiates other drugs (prescription and non-prescription) Physiology cont. Alcohol inhibits the hormone responsible for conservation of water in the kidney (vasopressin) Increased urination Dehydration Alcohol ingestion can cause vomiting Dehydration Chance of aspiration Blood Alcohol Concentrations EMS providers have no way to determine blood alcohol levels in the pre-hospital setting. Can sometimes estimate based on assessment and patient behavior Patients with long term alcohol use will not have signs and symptoms until blood alcohol levels are much higher Blood Alcohol Concentrations 0.02 – 0.05 gm/dl diminished fine motor coordination 0.05-- 0.10 gm/dl impaired judgment and coordination 0.08 gm/dl LEAGALLY INTOXICATED IN ILLINOIS 0.10 – 0.15 gm/dl difficulty with gait and balance 0.15 – 0.25 gm/dl lethargy, unable to sit upright without assistance 0.25 – 0.30 gm/dl 0.30 – 0.40 gm/dl coma in the non-habitual drinker respiratory depression Scenarios Alcohol (ethanol) ingestion can cause a variety of pre-hospital emergencies. For each scenario, determine: what is important about the scene size up initial assessment (Mental status, Airway, Breathing, Circulation) SAMPLE history head to toe exam management of the patient (BLS & ALS) Scenario 1 It is 2100 hours on New Year’s Eve You are called to a family home for an unconscious male. You are lead by an anxious middle aged woman to the basement family room. You find 4 young men standing around Tony, an 18 year old male lying on the floor face down in vomit and blood. The woman is Tony’s mother, she just got home from going out to dinner and found her son like this. Initial Assessment Level of Consciousness: Arouses to pain only Airway: occluded with vomit Breathing: labored and slow Circulation: pulse 90 at carotid strong, radial pulse weaker, skin warm and sweaty Chief Complaint: Altered level of consciousness What do you do now?? What is Tony in immediate danger of? SAMPLE Allergies– none Medications – none but vitamins Past Medical History – none healthy young senior in high school Last Meal – some chips and snacks since 7 pm Events – to celebrate New Year’s Eve Tony had a bottle of vodka. He has been drinking a shot with orange juice for each of his birthdays. He got to shot 10 and passed out flat on his face. Head to Toe Vomit on face and mouth, continues to vomit frequently requiring suction Approximately 1 inch gash over right eyebrow that is bleeding Pupils equal and slow to react Chest sounds are congested on right side Abdomen soft but Tony groans to palpation. No injuries noted on arms and legs. Tony has been incontinent of urine. Vital Signs BP 100/70 Pulse 90 Respirations 6 Oxygen saturation 90% on room air Blood Glucose 80 How do you manage Tony? What are your concerns? Management?? BLS Keep airway open with suctioning Assist ventilations with BVM and high flow oxygen Control bleeding of laceration Monitor level of consciousness for potential head injury Determine how to extricate from basement Consider spinal motion restriction Transport/ call for intercept ALS Continue BLS Monitor airway and breathing – lung congestion could mean aspiration Begin IV fluids for rehydration Monitor blood glucose -- acute intoxication can cause blood sugar to drop Consider Zofran 4 mg for vomiting control Continue to monitor neurological status for head injury Rule Out: Other reasons Tony may have an altered level of consciousness Head injury Seizure Sepsis Drug overdose Hypoglycemia Stroke Hypoxia Hypothermia Hyperthermia Binge Drinking National Institute on Alcohol Abuse and Alcoholism: consuming alcohol to reach a blood alcohol level of 0.08 gm/dl in < 2 hours One in six adults binge drinks 4 times a month with an average of 8 drinks Although binge drinking is more common among young adults (18-24 years) drinkers 65 years and older binge more often (5-6 times a month) Binge drinking is more common in high income households In addition to acute alcohol poisoning, binge drinking is associated with: unintentional injuries Motor vehicle crashes Drowning Burns Falls intentional injuries Domestic violence Sexual assault Firearms injures medical emergencies Poor control of diabetes Liver disease Hypertension– cardiovascular disease and stroke Scenario 2 You respond to a residence where a 3-year-old girl has been found unconscious. The parents tell you that the child, Ellie was fine when put to bed at eight the night before. They awoke this morning to find Ellie “asleep” on the living room floor, they are unable to arouse her. You note partially filled cocktail glasses on the coffee table and an open bottle of bourbon on its side on the floor. Some of the glasses have cherries in them. The parents admit that they were too tired to clean up after a party last night. What could be going on? What happened to this Ellie? How sick is she? General Assessment: PAT Appearance Unresponsive, lying sprawled in a pool of red vomit with cherry stems Work of Breathing Normal Circulation to Skin Normal What is your general impression? General Impression and Management Priorities General impression: Ellie is Sick Brain dysfunction; likely a metabolic/toxic cause What else could cause this? Seizure Infection Head trauma Other toxic ingestion What do you need to know to manage Ellie? Initial Assessment: ABCDEs Airway — open, vomit in mouth – lips and tongue are red and vomit contains bits of cherry and cherry stems Breathing — RR 16; symmetric chest rise; clear lungs; SaO2 94% Circulation — HR 90; skin moist; capillary refill 2 seconds; BP 80/60 Disability — AVPU = P; pupils sluggish but equal; decreased tone Exposure — breath and clothes smell of alcohol; no signs of trauma Chief complaint – Altered level of consciousness What is the most likely toxin? Sedative Sleepy Central nervous system depression Decreased respirations, heart rate and BP Suggested by open containers of alcohol and smell of alcohol on child’s breath and clothing Eating the sweet cherries out of the leftover drinks could contain enough alcohol to incapacitate a small child Management Priorities The patient is in impending respiratory failure because of alcohol ingestion. BLS: Consider airway adjunct. (OPA) Prepare for bag-mask ventilation. Arrange for transport. ALS: Check blood glucose Treat documented hypoglycemia. Establish IV access. Fluid bolus of 20 ml/kg or 10 ml/pound for dehydration Perform electronic monitoring. Consider intubation for airway protection if ALOC and absent gag reflex. Case Progression Blood glucose is 30 mg/%. IV started on scene. 10% Dextrose 1-2 ml/pound (2-4 ml/kg) IV administered. Patient becomes somewhat more responsive, but she remains sleepy. If problem was hypoglycemia alone she should wake up quickly. She is depressed because of the sedative effects of alcohol. There is no antidote for alcohol Key Concept: Hypoglycemia Hypoglycemia is common complication of alcohol ingestion in young children. If the patient is awake, ask the caregiver to give oral glucose (soda or juice). If patient is not alert or the gag reflex is depressed, give 10% Dextrose IV. Key Concept: Risk Assessment of Poisoning Determine: The substance ingested. Toxicity Dose ingested: mg toxin ingested per/kg body weight. Time since exposure. Call: Poison center (1-800-222-1222) or medical oversight to help with risk assessment. Key Concept: Ingestions by Toddlers Toddlers frequently ingest household products: solvents, cosmetics, plants, and cleaning liquids. Most ingestions in this age group involve single toxins. Few ingestions require charcoal or any specific treatment. Case Progression En route: patient remains stable, with progressive improvement in the level of consciousness. ED Course In the ED: repeat blood glucose 58. IV glucose infusion started, electrolytes, blood gas, and blood alcohol level sent. Social work consult obtained to evaluate home safety. Diagnosis: alcohol ingestion; hypoglycemia Outcome: social work call to children’s protective services (CPS) reveals an open case, with a past report of child neglect. Child is discharged the following day in the care of the maternal grandmother, pending CPS investigation. Toddlers are highly susceptible to the metabolic effects of alcohol, particularly hypoglycemia. Accidental ingestions peak in the 2- to 3-year age group. Prevention of poisoning in the home requires constant vigilance by caregivers and multiple rounds of “childproofing!” Scenario 3 You are dispatched at 2230 hours to a local tavern for an altercation On arrival you find 32 year old Dale sitting at the bar with a bloody towel to his face. What issues do you need to consider in this scene as you are approaching Dale? Dale states he got “sucker punched” in the nose. Police are on the way. The person who hit Dale has left the bar. Initial Assessment Mental Status: Dale is awake with slow measured speech Airway: mouth is clear, but nose is grossly deformed and swollen with blood coming from both nostrils Breathing: Unlabored at about 20/minute Circulation: Face flushed, skin warm and sweaty. Radial pulse strong and regular at 92/minute Chief Complaint: “I think that #&^* broke my nose” SAMPLE Signs/Symptoms: pain and swelling of the nose Allergies: none Medications: none Past Medical History: none Last Meal: supper at about 6:30 p.m. and has been at the tavern since about 8 p.m. He says he has had about 4 beers and 1 “Jack and coke”. (confirmed by bartender) Events: Dale got into an argument with another patron and Dale got punched in the face. Bystanders state he did not lose consciousness Head to Toe Pupils equal and react Alert to person, place, time and events Nose is swollen and deformed with bleeding from both nostrils No other injuries found: chest, abdomen, arms, legs BP 150/96 Pulse 92/minute Respirations 20/minute Oxygen saturation 94% room air Refusal?? Dale says he doesn’t want to go to the hospital. He just wants to get in his truck and go home? Can he do that? Autonomy All patients have the right of autonomy or the right to make decisions about their care. A patient does not lose their right to autonomy simply because they have been drinking alcohol. The challenge is to determine if the patient is competent to make these decisions. EMS providers are familiar with the signs of alcohol intoxication: Diminished fine motor coordination Decreased social inhibitions As alcohol intoxication increases Impaired judgement Impaired coordination, difficulty walking Agitation and combativeness Altered mental state Slurred speech Warm flushed skin Quick Confusion Scale A tool will soon be available to help providers determine how confused someone is due to alcohol. Adapted from: Huff JS, Farace E, Brady WJ, et al. The quick confusion scale in the ED: Comparison with the mini-mental state examination. Am J Emerg Med 2001;19:461-464 The Quick Confusion Scale Item Scoring System # Correct X weight = What year is it now? 0 or 1 (score 1 if correct and 0 if incorrect) 2 = What month is it? 0 or 1 2 = Total Present memory phrase: “Repeat this phrase after me and remember it: John Brown 42 Market Street, New York.” About what time is it? 0 or 1 2 = Count backward from 20 to 1. 0, 1, or 2 1 = Say the months in reverse. 0, 1, or 2 1 = Repeat the memory phrase. (each underlined portion correct is worth 1 point) 0, 1, 2, 3, 4 or 5 1 = Final score is the sum of the totals: = Explanation of Scoring for Quick Confusion Scale The highest number in category indicates correct response; decreased scoring indicates increased number of errors What year is it now? Score 1 if answered correctly, 0 if incorrect. What month is it? Score 1 if answered correctly, 0 if incorrect. About what time is it? Answer considered correct if within one hour: score 1 if correct, 0 if incorrect Count backward from 20 to 1. Score 2 if correctly performed; score 1 if one error, score 0 if two or more errors Say the months in reverse. Score 2 if correctly performed; score 1 if one error, score 0 if two or more errors Repeat the memory phrase: John Brown 42 Market Street, New York.” Each underlined portion correctly recalled is worth 1 point in scoring; score 5 if correctly performed; each error drops score by one. Final Score is sum of the weighted totals; items one, two, and three are multiplied by 2 and summed with the other item scores to yield the final score. Max score = 15. Score 11 likely cognitive impairment; score 7 = substantial impairment. Irons MJ, Farace E, Brady WJ, Huff JS: Mental status screening of emergency department patients: Normative study of the Quick Confusion Scale. Acad Emerg Med 2002; 9:989-994. What About Refusal? Complete the refusal form. Explain the benefits of medical treatment and the risk of refusing treatment Strongly encourage Dale to seek treatment If he continues to refuse, contact Medical Control. Involve local law enforcement to insure Dale is safe. Dale scores 12 on the confusion scale (he cannot repeat all of the memory phrase) Dale’s speech is progressively more slurred He was drinking when you arrived at the tavern Local law enforcement help you encourage Dale to seek treatment. Scenario 4 It is December 26 at 1330 hours. Bill has just arrived to visit his 88 year old mother Emma. Bill is from out of town and has not seen his mother since August. When she answered the door her gait was not steady. Bill helped her to her recliner and thought her speech was slurred and she was “dopey” so he called 911 thinking she has had a stroke. Scene Size Up Emma lives in a well kept house in an older neighborhood. The house is clean and tidy but full of “collectables” and books. Emma is sitting in a recliner in the living room. The table next to her has an empty glass and a wastebasket full of papers and other trash is next to the chair. Initial Assessment Mental Status: Emma is awake but slow to respond, with slightly slurred speech Airway: Open and clear Breathing: Respirations easy and deep at 16/minute. Breath smells of peppermint Oxygen saturation 93% room air Circulation: pulse is irregular at 88/minute, skin is warm and dry Chief Complaint: “I’m fine Sweetie, just a little tired.” SAMPLE Signs/symptoms: unsteady gait and slurred speech Allergies: morphine Medications: Vasotec 5 mg twice a day, potassium 20 meq daily, Lipitor 30 mg daily, Micronase 5 mg daily, Aspirin 81 mg daily Past Medical History: hypertension, high cholesterol and Type II diabetes Last meal: Unknown for sure. Emma said she had lunch at 11:00 am Events: Unknown Head to Toe Exam Pupils hard to evaluate due to cataracts. Mouth has green/blue discoloration of the tongue, lips and tongue are dry. Chest has some congestion Abdomen soft Multiple bruises on bilateral lower arms and shins Ankles have bilateral edema Blood Sugar 280 FAST Assessment Face – both sides move equally Arms – both arms raise equally Speech – slurred, Emma giggles when she has trouble speaking Time – Bill has not seen his mother since August and has not talked to her on the phone for 2 days. Your partner looks in the waste basket and finds 2 large bottles of blue mouthwash that are empty. Emma tells you that she will admit she has been drinking more since her friend Betty died this fall because it makes her feel “happy”. She ran out of Tequila and the weather was bad, so she has been drinking mouthwash because it was in the house and it tastes better. Mouthwash??? Ethanol is not only found in alcoholic beverages but is a main ingredient in mouthwash, over the counter cold medications (Nyquil™) and perfume. Individuals who want to hide their ethanol intake or who are unable to obtain alcohol may drink other forms of ethanol. Household ethanol is also a danger for accidental pediatric overdose. Medical Side Effects of Ethanol Poor control of diabetes Hypertension Liver disease Stroke Cardiovascular disease What are your concerns about Emma? How do you want to manage her care? Management BLS care Monitor airway and breathing Oxygen by cannula to an O2 Saturation of 94% ALS care IV access and fluid bolus (monitor lungs) EKG monitoring for dysrhythmias Her monitor shows What is this? What else does Bill need to consider regarding his mother? Bill needs to seek help to find other ways for his mother to deal with the loss of her friend other than drinking. Scenario 5 Dispatched at 0730 hours For a middle aged woman who is “out of her mind” Scene Size Up Upscale neighborhood Well kept house Small barking dog is held by husband who answers the door. General Impression Disheveled middle aged woman, Edie, sitting on kitchen floor Hitting the floor with her slipper Appears very anxious and frightened Initial Assessment Mental Status: awake but is distracted and does not follow commands Airway: open with very dry mucus membranes Breathing: 28, deep and rapid Circulation: skin pale, cool and moist Radial pulse fast, weak and thready Chief Complaint: “There are too many bugs” Focused History Allergies: codeine Medications: Alprazolam 1 mg BID Inderal for blood pressure Synthroid 150 mg Ambien at nighttime for sleep Past History Hypothyroidism “bad nerves” Social drinker (averages 2 bottles of Chardonnay or other wine every evening) Last Meal 24 hours ago Events: Edie wanted to surprise her son for Christmas, so she quit drinking 2 days ago. She started feeling ill yesterday with feeling weak and no appetite. This morning Edie is shaky and confused. She says she sees black bugs all over the kitchen (no one else can see them). She feels them crawling all over her skin and she is trying to rub them off. Focused Physical VS: BP 100/60, P 120, R 28 Pulse Ox: 94% on room air EtCO2 34 Blood Sugar: 70 Has trembling of arms Rubs on arms and legs trying to brush off bugs Red raw abrasions on both arms Poor skin turgor, and dry mucus membranes Very poor attention span. Does not listen to you. Edie’s husband says “she’s lost it and has gone crazy” Cardiac Rhythm What is this? Long Term Alcohol Abuse General Alcoholic Profile Drinks early in the day, alone, or secretly. Binges, blackouts, GI problems, chronic flushing of face and palms. Cigarette burns, tremulousness, and odor of alcohol. Alcohol Abuse Consequences of Chronic Alcohol Ingestion Poor nutrition Alcohol hepatitis Liver cirrhosis, pancreatitis Sensory loss in hands/feet Loss of balance and coordination Upper GI hemorrhage Hypoglycemia Falls (fractures and subdural hematoma) Alcohol Withdrawal Syndrome Alcohol (ethanol) withdrawal syndrome can begin as early as 6 hours after the fall of blood alcohol levels and usually peaks between 24 and 36 hours. It can take up to 5 days after the termination of drinking to resolve. Delirium Tremens (DTs) is a life threatening manifestation of ethanol withdrawal characterized by tremors, hallucinations and hypovolemic shock. DTs appear in 48-96 hours and can persist up to 7 days. Withdrawal Syndrome DTs Signs & Symptoms Coarse tremor of hands, tongue, eyelids Nausea, vomiting, general weakness, anxiety Tachycardia, sweating, Hallucinations – frightening or threatening visual (seen) auditory (heard) and/or tactile (felt) Signs and Symptoms cont. Increased sympathetic tone -- seizures Orthostatic hypotension (BP drops when patient stands up) OR hypertension Dehydration – hypovolemic shock Irritability or depressed mood, poor sleep DTs are a serious medical emergency!! Alcohol Abuse BLS Treatment Establish and maintain the airway. Determine if other drugs are involved. Prevent self harm. Be alert for seizures Do not “buy into” the hallucinations • Do not say that you see the hallucinations too • Do not tell Edie that there are no bugs there • Acknowledge that Edie is afraid and that she sees bugs but that you can’t see them. Treatment cont. ALS Establish IV access. • • • • Replace fluids at 20 ml/kg for dehydration 25g D50W if hypoglycemic or 1-2 ml/pound (in 50 ml boluses) of D10W if hypoglycemic Versed 0.1 mg/kg for shaking or seizures Transport, maintaining a sympathetic attitude, and reassure the patient. Review Answer the following questions as a group. If doing this CE individually, please e-mail your answers to: shelley.peelman@presencehealth.org Use “December 2015 CE” in subject box. You will receive an e-mail confirmation. Print this confirmation for your records, and document the CE in your PREMSS CE record book. IDPH site code # 067100E1215 1. How does alcohol (ethanol) effect the body? a. b. c. d. Hallucinogen Stimulant Sedative Opiate 2. How does a person usually respond to low doses of alcohol? a. b. 3. How does a person usually respond to higher doses of alcohol? a. b. c. 4. Why do people get warm when they drink? 5. Why do people wake up very thirsty after drinking alcohol? 6. Name some other emergency conditions that might be masked by alcohol intoxication? a. b. c. 7. What specific medical problem occurs when children drink alcohol? 8. True/False Patients with alcohol on their breath lose all their ability to make decisions and must be transported to the hospital. 9. If a person has no access to alcohol, what other household items contain ethanol and can be used to get intoxicated? 10.Why are DTs dangerous? Answers 1. How does alcohol (ethanol) effect the body? a. b. c. d. Hallucinogen Stimulant Sedative Opiate 2. How does a person usually respond to low doses of alcohol? a. depression of inhibitions b. aggressive or inappropriate behavior 3. How does a person usually respond to higher doses of alcohol? a. dulled sense of awareness b. decreased coordination c. decreased reaction time stupor and coma 4. Why do people get warm when they drink? Alcohol ingestion causes peripheral vasodilation which increases sense of being warm and loss of body heat 5. Why do people wake up very thirsty after drinking alcohol? Alcohol is dehydrating and increases removal of water through urination. 6. Name some other emergency conditions that might be masked by alcohol intoxication? a. head injury b. low blood sugar c. infection seizures/ post ictal state hypoxia 7. What specific medical problem occurs when children drink alcohol? hypoglycemia (low blood sugar) 8. True/False Patients with alcohol on their breath lose all their ability to make decisions and must be transported to the hospital. False 9. If a person has no access to alcohol, what other household items contain ethanol and can be used to get intoxicated? mouthwash, perfume, liquid cold medicine 10. Why are DTs dangerous? DTs can lead to seizures, hypotension and hypovolemic shock.