Applied Science
advertisement

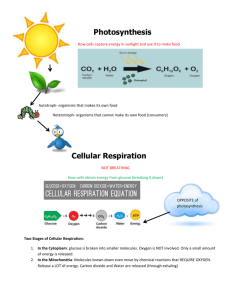
Unit 14 The Healthy Body You need to know, understand and be able to demonstrate How basic homeostatic mechanisms maintain a healthy body The human body is organised into cells, tissues and organ systems. They interrelate with each other to enable the body to function. Cellular, tissue or organ activity can be monitored to provide information about how effectively any particular individual is able to perform under different conditions. You should know: the function of the component parts which make up the cardiovascular system – how these parts function individually and how the system functions as a whole. You should be aware of common defects of the heart and apply your knowledge of the structure of the heart to these defects; the function of the component parts which make up the pulmonary system – how these parts function individually and how the system functions as a whole; about homeostatic mechanisms and how they function as detection/correction systems – for example in the control of blood sugar concentration or the concentration of carbon dioxide in the blood; the role of hormones in body function; the source, role and regulation of antidiuretic hormone (ADH) secreted by the hypothalamus and how it regulates blood volume and changes blood pressure; the source, role and regulation of insulin and glucagon in regulation of blood glucose concentration; the source, role and control of thyroxine; the homeostatic mechanisms involved in regulation of sodium – for example the source, role and control of aldosterone; that blood is an aqueous electrolyte mixture containing sodium ions and chloride ions; why sodium ions and chloride ions are important to the healthy functioning of the body; how these ions are obtained by the body and how they can be lost from the body; the consequences of sodium chloride (salt) deficiency in the short term and the long term; circumstances in which certain people may be at risk of losing too much salt; why excess salt in the diet might create health problems. Cellular respiration This is the process that enables every living cell to obtain energy for its activities. Biochemists can analyse the rates of cellular respiration in samples of tissues; this is usually done in a specialised laboratory. Sport physiologists can determine whether an individual is respiring aerobically or anaerobically using non-invasive methods (indirect calorimetry) – for example the collection of exhaled gases and analysis of these in a gas analyser. This information can be used to calculate the basal metabolic rate (BMR) of an athlete at rest. The same method can be used to calculate metabolic rates while exercising. The information about metabolic rate can be used to ensure that energy expenditure meets energy inputs. The BMR can also be determined by whole body (direct) calorimetry. You should know: the balanced symbol equation for aerobic respiration; that during cellular respiration adenosine triphosphate (ATP) is produced by phosphorylation by the addition of a phosphate group to a molecule of adenosine diphosphate (ADP); that ATP can be used to release energy for cell activity; that the first part of the breakdown of glucose takes place in the cytoplasm of the cell. Following this, aerobic respiration takes place in structures called mitochondria; that cells can metabolise carbohydrates, fats and proteins to make ATP. You should be able to: describe, in outline, the stages in the respiration of glucose that result in the production of ATP. These stages are known as glycolysis, the Krebs cycle (the citric acid cycle or tricarboxylic acid cycle or the TCA cycle) and the electron transport system; state and compare the amount of ATP that can be produced from aerobic and anaerobic pathways; understand where fat (lipids) and protein can enter glycolysis, the Krebs cycle and the electron transport system; define what is meant by BMR and explain how it can be determined in a laboratory by direct or indirect methods; explain the differences in BMR for males and females, and for different age groups of both genders using secondary data; explain methods of monitoring the respiratory system (breathing rate and volumes). How to monitor concentrations of substances in the blood Cells in the body can only function properly in a suitable environment. This environment is provided by the tissue fluid which bathes the cells. Since tissue fluid is derived from blood, the levels of various substances in the blood are critical. Blood pH the normal pH range for blood (7.35–7.45) and why pH values for arterial and venous blood are different; how blood is buffered to maintain pH within safe limits; some of the causes and effects of blood becoming too acidic or too alkaline; the diseases or conditions in which acidic or alkaline blood conditions can arise – for example diabetic acidosis. Oxygen saturation The majority of oxygen is carried by the molecule haemoglobin. When haemoglobin carries eight oxygen atoms (i.e. Four O2 molecules) it is said to be fully saturated. Doctors, nurses and physiotherapists monitor the oxygen saturation levels of patients with respiratory diseases, or when people are in intensive care. Reduced oxygen levels will interfere with the ability of cells to respire properly and a consequence of this is that cells may die. You should know: how oxygen is transported on haemoglobin, and the effect of blood pH and temperature on oxygen transport – for example the Bohr effect on the oxygen dissociation curve; oxygen saturation is written as SaO2%; a machine called a pulse oximeter is used to measure oxygen saturation. It is a non-invasive method; the normal range of oxygen saturation levels is 95–99%; people with diseases such as emphysema or cystic fibrosis may have reduced oxygen saturation levels. Blood glucose Brain cells depend on direct supplies of glucose from the blood, so brain cells are starved of energy if glucose levels fall too low. Excess glucose is normally removed from the blood and converted to glycogen or fat for storage. Our body constantly monitors our blood glucose level internally. However, in certain situations it is necessary for individuals to manage directly their own blood glucose level – for example people with diabetes. Diabetics need to be very careful in relation to their diet and their use of insulin. They need to monitor their blood glucose concentration regularly and ensure that this stays within safe limits. You should know: about the body‟s normal system for regulating blood glucose levels – for example the cells and organs involved; how blood glucose is regulated by the antagonistic action of insulin and glucagon with particular reference to diabetes; about situations in which blood glucose levels need to be monitored; the normal range of values for blood glucose concentration (fasting glucose level is 3.5–7.5 mmol/litre); why the presence of glucose in the urine can be an indicator that regulatory mechanisms are not working properly; how a simple glucose test can be carried out on urine samples in a healthcare setting – for example dipstick tests; how a glucose tolerance test can be used to monitor how glucose is handled in the blood, and how it can be used to assist diagnosis of diabetes. How a healthy diet helps to maintain a healthy body Dieticians work in the health service or with professional sports teams – for example cycling teams, football teams and athletes. In the health service, dieticians may advise people who are very obese, or have diabetes, on the best way to achieve better health through their diet. Sports teams employ dieticians whose job it is to ensure that team members receive adequate and appropriate nutrition to achieve maximum sporting performance. You should know: the principles of the composition of a healthy diet for an average person – including the proportions of different food groups; the energy needs for different groups of individuals –including babies, infants, teenagers, pregnant women, adults and the elderly; the nutritional needs for different individuals – including babies, infants, teenagers, pregnant women, adults and the elderly; how and why a diet may need to be modified to suit the needs of specialist groups – for example diabetics, the obese and elite athletes. Monitoring the levels of cholesterol, vitamins and minerals in the body Hospitals have specialist doctors, nurses and dieticians who advise individuals about the risks of cardiovascular or bone problems and the need for suitable levels of micronutrients – such as cholesterol and calcium – in their blood and how the levels can be managed. The testing of these micronutrients is usually carried out by biochemists in medical analytical laboratories using specialised equipment. Nutritional advice is given to help maintain health or reduce the likelihood of health problems developing in the future. Several companies produce low-fat spreads which may impact on blood cholesterol, and may be used as part of a healthy diet and lifestyle to help reduce the intake of saturated fats. Some spreads and yoghurts are also manufactured which can actually reduce the levels of cholesterol in the blood. Many breakfast cereals are supplemented with vitamins and minerals. You should know: the source, regulation and use of the following blood components: cholesterol, vitamins B, C, D and E and the minerals iron, sodium and calcium; the normal levels of total cholesterol in the blood (fasting total cholesterol should be 4.0–6.5 mmol/litre); how the level of cholesterol can be measured in a healthcare setting – for example the dipstick test and cholesterol meter; the health effects of continually high or low cholesterol; the normal levels of vitamin B, C, D and E in the blood and how these are detected; the effects of deficiencies of vitamin B, C, D and E in terms of disease, and ways that these deficiencies can be addressed; the effects of excess vitamin B, D and E; the normal levels of iron, sodium and calcium in the blood and how these are detected – for example iron levels can be determined indirectly by looking at haematocrit (packed cell volume) or by detecting haemoglobin levels in the blood; the effects of deficiencies of iron, sodium and calcium in terms of disease and the ways these deficiencies may be addressed. The structure and function of the digestive system The ability of the body to absorb nutrients in an available form depends on healthy functioning of the digestive system. Dentists and dental hygienists help people to maintain good dental health by advising on cleaning routines for teeth and gums. Radiographers can image the contents and structures of the digestive system using radio-opaque materials. Surgeons can look inside the digestive tract using endoscopes. It is important for these healthcare workers to know what the normal structure and function of the digestive system looks like in order to be able to diagnose disease. You should know: the function of teeth, the tongue and saliva; about chemical and mechanical digestion in the mouth; how the mouth keeps itself clean and how good dental hygiene can be maintained; the structure and mechanical action of the different regions of the digestive system; the role of acid, mucus and enzymes in the stomach; the role of enzymes in the digestion of proteins, carbohydrates and fats; how enzymes regulate and facilitate digestion of the components of foods, and that they are specific in their action and in the conditions under which they can operate; about the digestion of fats and the control of pH in the small intestine by the action of bile and bile salts; about the control of the sequence of digestive activity from ingestion to egestion by hormones – for example gastrin; how the structure of the gut is designed to meet its function of absorption; how the intestine monitors and controls the levels of fluid in it to facilitate digestion and prevent excessive water loss; about the role of the digestive system in water intake and balance.