RHEUMATOLOGY

RHEUMATOLOGY
1
• Rheumatoid arthritis
• Fibromyalgia
• Osteoporosis
• Ankylosing spondylosis
• Juvenile Idiopathic arthritis
• Reactive Arthritis
• Gout, Pseudogout
• Misc
2
RHEUMATOID ARTHRITIS
Maryam Nauman
3
• In UK, 26,000 new cases diagnosed per year,
• More than 690,000 cases already living with this condition
ECONOMIC IMPACT
Loss of job, reduced working hours, off sick, reduced family income
Annual impact of RA in Western Europe 42 billion
Euros
RA costs £8 billion/year to UK economy
4
5
37 Year old presents to you with pain in joints very suggestive of Rheumatoid arthritis
1.
Asymmetric arthritis more than 6 weeks duration
2.
Absence of soft tissue swelling
3.
Morning stiffness more of than 1 hour duration for at least 6 weeks duration
4.
Normal X-rays
6
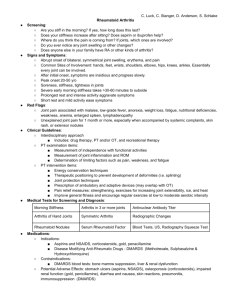
DIAGNOSIS-ACR Criteria
• • AM STIFFNESS (1 h)
• • INFLAMMATORY ARTHRITIS OF ≥ 3 JT AREAS
• • INFLAMM ARTHRITIS OF HAND JTS (wrist MCP PIP)
• • SYMMETRIC ARTHRITIS
• • RHEUMATOID NODULES
• • SERUM RHEUMATOID FACTOR OR ANTI-CCP
• • RADIOGRAPHIC CHANGES TYPICAL OF RA
• FOR ≥ 6 WKS
• Any 4 = rheumatoid arthritis
• Specificity: 40-60%, 95-100%
7
• Classification criteria for RA (score-based algorithm: a score of
≥6/10 is needed for classification of a patient as having definite RA)
Joint involvement 1 large joint- 0, 2-10 large joints-1
1-3 small joints (with or without involvement of large joints) -2
4-10 small joints (with or without involvement of large joints) -3
>10 joints (at least 1 small joint)- 5
Serology (at least 1 test result is needed for classification )
Negative RF and negative ACPA-0
Low-positive RF or low-positive ACPA-2
High-positive RF or high-positive ACPA-3
Acute-phase reactants (at least 1 test result is needed for classification )
• Normal CRP and normal ESR-0
• Abnormal CRP or abnormal ESR-1
Duration of symptoms
• <6 weeks- 0
• ≥6 weeks-1
8
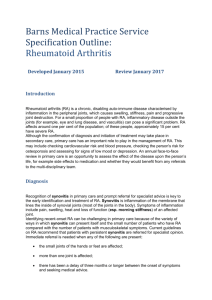
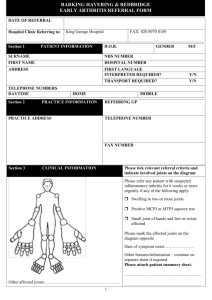
Who would you refer to specialist
• 37 year old female with pain effecting small joints of both hands
• 54 year man old with pain and tenderness in hip joint
• 35 year old female with fever, generalised tiredness and increased CRP and positive RF
9
Referral for specialist opinion
• Any person with suspected persistent synovitis of undetermined cause
REFER URGENTLY IF ANY OF THESE ARE
AFFECTED
• Small joints of hands or feet are affected
• More than one joint is affected
• There has been a delay of 3 months or longer between onset of symptoms and seekin medical advice
10
PHARMACOLOGICAL MANAGEMENT
INVERTED PYRAMID
• NSAIDS, ANALGESICS
• – For pt who may not have RA
• – To ease pain while waiting for the 6 week point for
• spontaneous improvement
• • DMARD
• – In any patient with RA without contraindication
• – Methotrexate, hydroxychloroquine, sulfasalazine
• – leflunomide
• • MORE THAN ONE DMARD: 3>2 = biologic; 2>1
• – If you do not want to give biologic – cost, toxicities
• • BIOLOGIC AGENT PLUS METHOTREXATE
• – For any patient without excellent response to DMARD
11
DMARD
DRUG
SULFASALAZINE
METHOTREXATE
LEFLUNOMIDE
DOSE
Oral 500 mg upto
3g/day
Oral 7.5 g/wk upto
20mg/wk,add folic acid 5mg 3days after each dose
Oral loadin dose
100mg,,maintenanc
10-20 m
SIDE EFFECTS
Nausea, rash, neutropenia, low sperm count, abnormal LFT
Alopecia,rash, N, D, fhepatic fibrosis,leucopenia, mouth ulcer
Diarrhea,rash,hair loss, HTN, nausea, increased liver enzymes
MONITORING
REQUIREMENTS
FBC, LFT at start,
FBC 2 weekly, LFT
4 weekly for 12 wks,
3monthly for yr then
6 monthly
FBC, UE,LFT,CXR baseline. FBC weekly until 6wks afterlast dose increase,then monthly LFT
FBC basline,every 3 weeks for 6 months then every 8 weeks,
ALT baseline and then monthly~6m, monitor BP
12
HYDROXYCHLORO
QUINE
Penicillamineobsolete
Oral 200 mg
Oral 125m/day
Sodium aurothiomalate- now obssolete
I/M 10
AZATHIOPRINE 1.5-3 mg/kg/day
Rash, GI upset, retinl al toxicity
Rash, nausea,loss of taste,pancytopenia, proteinuria
Rashm mouth ulver,proteinuriaa, pancytopenia, nephrotoxicity
Bm supp, GI upset,
,hepatitis
Basleine ophthalmo, then 6 monthly, and annualy
Basline
FBC,UE,urinalysois, then monthly
FBC, urinalysis baseline and before each injection
FBC baslein and monthly
13
ANTI-TNF THERAPY
• @-TNF Inhibitors- active arthritis, have undergone trial of 2
DMARDS inc methotrexate
• Infliximab-IV infusion
• Etanercept- in children also-s/c injections
• Adalimumab-s/c inj
• Anti IL1-Kineret,Ticlizumab, Rituximab, Abataccept orencia
14
15
Fibromyalgia
Nicolas Milhavy
GP ST1 VTS
16
Not well understood despite widespread research in the USA,
Canada and Europe……
Can have a definite trigger or can come on gradually out of the blue
17
Diagnosis
• A history of chronic and widespread pain (CWP)
• ‘Pain and fatiguability with multiple hyperalgesic tender sites
(11/18)’
18
American College of
Rheumatology – Classification
(1990)
1.
Pain in the left and right side of the body, pain above and below the waist and axial skeletal pain (shoulder and buttock included on each side and lower back pain considered lower segment pain) for at least 3 months
19
American College of
Rheumatology – Classification
2. Pain (not tenderness) with digital palpation in 11/18 sites
(1990)
» Occiput – bilaterally
» Low cervical C5-C7
» Trapezius – bilateral
» Supraspinatous – above scapula
» Second rib – bilateral
» Lateral epicondyle – bilateral
» Gluteal – bilateral
» Greater trochanter – bilateral
» Knee - bilateral
20
‘Manchester’ Definition
Pain must be present in 2 separate sections of a body quadrant to be positive
21
Epidemiology
• CWP prevalence is above 10% if American College of Rheumatology definition is used
• CWP prevalence is 5% with ‘Manchester’ definition
• Twice as high in females
• Fibromyalgia
» 0.7-4.8% in comparable studies using ACR criteria
» 90% female, peaks aged 40-50
22
Clinical picture
• Pain – axial and diffuse, felt all over
• Pain worsened by stress, cold and activity, association with
EM stiffness
• Parasthesiae in hands and feet common
• Analgesics and NSAIDs ineffective and may worsen symptoms
• Poor sleep pattern – wake exhausted and poor concentration
• Anxiety and depression scores are high
• Unexplained headaches, urinary frequency and abdominal symptoms are common
• Clinical findings unremarkable
23
Pathogenesis
• A poor, unrefreshing sleep pattern – unable to enter the 4 th phase of sleep (deep refreshing sleep)
• Muscles do not relax and resting muscle tension is raised – this causes aching all over that means the person cannot sleep well the following night – a vicious circle that is difficult to get out of
• Napping in the day worsens symptoms as it means the body cannot enter the restorative phase
• Low levels of NTs in the brain and abnormal processing of sensory stimuli – light touch and movements can cause significant pain that is real with no structural explanation
• Reduced aerobic fitness
• Behavioural affective symptoms
24
• Hypothyroidism
• SLE
• Sjorgren’s
• Psoriatic arthritis
• Inflammatory myopathy
• Hyperparathyroidism
• Osteomalacia
Differential Diagnosis
25
Diagnosis
• Exclude differential
• FBC, ESR, TFTs, U and Es, Calcium, CK, phosphate, ANA, RhF and immunoglobulins
26
Management
• Good explanation
» To patient and the family
» Relieve concerns of sinister causes for pain
» Rationalise with lack of sleep and fitness
• Avoid unnecessary investigation
• Regulate a better and more refreshing sleep pattern
• Increase aerobic exercise or physiotherapy (a graded and sustainable exercise regime)
• Low dose amitriptylline, dothiepin or fluoxetine
• Consider CBT or counselling
• MDT approach with rheumatology and pain clinic
27
• Poor
• 20% are symptom free at 5 years
• Treatment may help with coping strategies
Prognosis
28
Case History
Joblu Khan
29
Case History
Joblu Khan
• 54 year old gentleman
• Difficult patient
– Well read
– Frequent attender
– ‘Hypochondriac’
Mr ARL
• “Osteoporosis”
– “aches and pains all over”
• Recent wrist fracture
Mr ARL
• Winter (December) 2010
• Fall onto outstretched hand (L hand)
• ED
– 999
• # wrist L
– Backslab 6/52
– Finger, elbow and shoulder exercises
– Discharged from ortho recently
• Dr S Hameed (SHO)
Mr ARL
• Consultation
– Risk Stratification
Mr ARL
• Body weight
– ‘chubby’ (BMI 25 to 30)
• Nutritional
– Takeaway and microwave meals
• Lifestyle
– Enjoys walking the dog
• Limited knee pain
– Ex smoker (10 pack year history)
– 2 cans of Guinness most nights
Mr ARL
• Family history
– Mother osteoporosis
• Severe COPD
• PMH
– HTN
– High cholesterol
– Diabetes Mellitus (diet controlled)
– Mild OA L knee
• DH
– Amldoipine
– Simvastatin
– Paracetamol PRN
• Bld tests (random)
– FBC, ESR
– U&Es
– LFTs (ALP 154 (40 – 129))
– Bone
– TSH
– Testosterone
– Random glucose (11.2 mmol/L)
– Cholesterol (4.5 mmol/L)
Mr ARL
• DEXA scan
– T score of – 2.6
• What is the diagnosis?
• Treatment of choice?
• Need to refer?
• Follow up investigations needed?
Mr ARL
Mr ARL
Osteoporosis
• Systemic skeletal disease
• Low bone mass and micro-architectural deterioration
• Increase in bone fragility and susceptibility to facture
• Considerable morbidity and mortality
• Increasing in developing countries
– Increasingly elderly population
• Previous low trauma fractures
– # from fall from standing
– Loss of height/kyphosis (? Vertebral #)
• Age > 60 and female sex
• Recurrent falls
• Glucocorticoid use
• FH of osteoporosis
• Secondary causes
Investigate
• Degree of osteopenia
– DEXA
• Establish current fracture risk
• Establish future fracture risk
• Monitor effect of treatment
• Osteopenia
– Tscore – 1 and – 2.5
• Osteoporosis
– T score <2.5
Diagnostic evaluation
Diagnostic evaluation
• Exclude secondary osteoporosis
– Primary hypoparathyroidism (serum Ca)
– Thyrotoxicosis (TSH)
– Myeloma (ESR, plasma electrophoresis, BJ proteins)
– Osteomalacia (serum Ca, Phosphate, ALP)
– Malabsorption syndrome (FBC)
– Hypogonadism in men (testosterone)
• Anti resorptive drugs
– Etidronate
• Didronel®
– Alendronate
– Risedronate
– Ibandronate
– Raloxifene
• SERM
– HRT
– Testosterone therapy
• Hypogonadism
– Calcitonin
– Calcium and Vit D
• Calcichew D3 forte
Management
Management
• Formation stimulating drugs
– Recombinant fragment of parathyriod hormone
• Specialist centres
– Strontium ranelate
• Treating secondary causes
– Partial recovery
• Preventing falls
– Predisposing causes
• Postural hypotension
– Physiotherapy
– Hip protectors
• Optimize peak bone mass
– Exercise
– Regular and weight bearing
– Dietary calcium
• Reduce rate of bone loss
– HRT
– Exercise
– Calcium intake
– Moderate alcohol intake
– Stop smoking
• Prophylactic treatment
– ? Cost effectiveness
Preventing osteoporosis
• Determine risk
• Preventable
• Treatment effective
• ? Guidelines
• QOF?
Osteoporosis
Case Presentation
Ulfat Younis
50
32 year old Male
Works as a Brick Layer
• Lower Back Pain
– Comes and goes
– Persistent episodes past few years
– Worse at night (wakes from sleep) and at rest
– Better with Exercise
– Stiffness, better through the day
– Associated Lethargy and low mood
– Has had 2 episodes of painful and red eye over last 12 mnths...
– What More Do You Want To Know?
– What is the likely Diagnosis?
51
Ankylosing Spondylosis
•
Ankylosis= Fusion across a joint
•
Spondylosis= Inflammation
• Sacroiliac and Vertebral joints
• Affects Young Males (Age 20-40Yrs), 3-
5x>more common in Men.
• Anterior Uveitis (40%), Other Tendon/Joint involvement
• Unknown Aetiology
• Hereditary Tendency
– HLA-B27 (9/10 with AS are +ve)
52
Diagnosis
• History:
– Persistent, grumbling episodes of Back pain and Index of suspicion.
– Differentiate from ‘Mechanical Back Pain’.
• Investigations:
– Bloods
• Inflammatory Markers in acute phase
– X ray
• Sacroiliitis,‘Bamboo spine’ fusion, Delayed changes
– MRI
• Earlier changes, inflammation of SIJ
53
54
55
Treatment
Ease Pain, reduce stiffness, maintain mobility
Physiotherapy + NSAIDS for flare ups
Immunosuppressant Drugs:
• Biological Therapies
– TNF-Alpha Blockers Monoclonal AB (Etanercept, Infliximab)
– NICE: Adalimumab/Etanercept for severe AS +
• Active spinal disease (assessed 2x 12 weeks apart
• Have tried at least 2 NSAIDs ineffectively
•
Immunomodulators
– Suppression of the immune response (Sulphasalazine)
– ?Effectiveness in AS
56
Prognosis
• Good..intermittent flare ups, mild-moderate severity
• Regular exercise (Low impact)+ Analgesia to control symptoms
• Gradually increasing stiffness with age
• 8/10 remain fully independent with limited disability (despite eventual spinal restriction)
• 1/10 severe form AS...Anti-TNF Rx promising
• Extra-axial:
– Lung Fibrosis Restrictive defects, Parasthesia,
Amyloidosis, AR, Enthesopathy etc..
57
Juvenile Idiopathic Arthritis
Gordon irvine
58
Case Study
• 15 year old boy
• School sports star (captain of rugby)
• Developed swollen fingers and knees
• Lumps on back of wrists
• Otherwise well
• No Fam Hx
59
• Any arthritis-related condition < 18yrs
• 1 in 1000 children in UK
• Most types more common in females
• Most children won’t have lasting impact
JIA
60
• Most common (60%)
• Girls < 5yrs
• Mildest
• 1-4 joint in first 6mths (knee, ankle, wrist)
• Morning stiffness
• Moodiness
• Walking?
• Uveitis (1in 5)
Oligoarthritis
61
Polyarthritis
• 2 nd most common 20% (girls>boys)
• 5 or more joints
• Hands and feet > knees, wrist, elbows, ankles, hips, neck, jaw
• Soreness of tendons of hands
• Unwell +/- fever
62
Systemic Arthritis (Still’s Disease)
• 10% (boys=girls) often aged <5
• Affects body as whole
• Difficult to diagnose
• ? Pericardium
• Fever lasting several weeks and rash
63
• Associated with psoriasis
• Girls 8-9 yrs
• ? Uveitis ? Pre dates psoriasis
Psoriatic Arthritis
64
Enthesitis-related Arthritis
• Usually affects boys > 8yrs
• Arthritis in several joints (sacroiliacs and tendon insertions)
• Eyes often affected
• Associated with HLA-B27
65
What Causes JIA?
• No clear evidence passed down through families.
• Certain illnesses may act as trigger on those with genetic predisposition
66
• Bloods:
– FBC, ESR, CRP, U&E, LFTs, Autoantibodies
• Xrays and USS/MRI
• Eye Tests
Diagnosis
67
Treatment
• Referral
• Drugs (NSAIDs, DMARDS, Steroids, Biologics,
Eye Drops)
• Physiotherapy
• Surgery
68
• Exercise (encourage)
• Diet (Calcium, Vit D and Iron)
• Pain Management
• Others (Complementaries, aids etc)
Self Help
69
Where’s our case?
• 32 yrs old married
• Lived in Boulder, Colorado for 7 years
• Summer: climbing, mountain biking and outdoor guide
• Winter: ski instructor and guide
70
Can’t pee, can’t see, can’t climb a tree!
Kathryn Burnett
71
72
Reactive arthritis
• Sterile inflammatory oligoarticular arthritis occuring 2-4 weeks following a remote infection
• Usually following urogenital or enteric infection
• Most patients aged 20-40
• Asymmetrical lower extremity oligoarthritis
73
74
Prognosis
• 25-50% of patients will have further acute episodes of arthritis
• 15% proceed to chronic arthritis (more likely if HLA B27 positive) requiring referal to rheumatology for consideration of DMARDs
• Most patients symptoms resolve within 3-12months
75
Remember
• STI screen for young person presenting with oligoarthritis even if no urogenital symptoms.
76
GOUT & PSEUDOGOUT
Jennifer Thornhill
77
A. Colchicine
B. Intra-articular steroid injection
C. IM steroid
D. Methotrexate
E. Oral steroids
F. Physiotherapy
G. Probenecid
H. Referral for surgery
I.
Rest
J.
Splinting
Answers
78
• De Qervain’s tenosynovitis not responding to rest and a wrist support
• Early morning stiffness and pain in shoulders with raised ESR
• Acutely swollen first MTP joint
• Acute onset lumbar backakce when lifting with right sided sciatica
• Pt with fibromyalgia complains of multiple tender points in her shoulders; examination reveals normal range of movement but numerous trigger points within the muscles.
79
Case
• 42 year old male police officer
• Acutely swollen, hot right knee
• Feels tight, limping slightly
• No history injury
• PMH: prev ACL repair, previous patellar dislocation, high cholesterol, gout (toe and thumb – once a year for 8 years)
• SH: drinks 15 pints per week.
80
Examination
• Moderate effusion to knee
• Warm to touch
• No erythema
• Ligaments stable
• Recent exacerbation gout in right thumb – improved with indometacin. Been taking last 3d for knee – no improvement.
81
Differentials
• Infection
– cellulitis
– septic bursitis
– aseptic arthritis
• Rheumatoid arthritis
– polyarticular gout that affects the fingers may be mistaken for rheumatoid arthritis
– if there are elbow tophi these may be mistaken for rheumatoid nodules
• Bunion
• Chondrocalcinosis - pseudogout
• Seronegative arthritis
82
Investigations
• Serum urate (optimal time 2w after attack)
• Leucocytosis and raised ESR/CRP during attack
• Assess other CV risk factors – fasting lipid, BP, glucose
• Aspiration and polarised light microscopy of synovial fluid
• Radiology
83
• Correct exacerbating factors
– Consider stopping or reducing diuretics
– Reconsider aspirin
– Reduce alcohol intake
– Reduce intake of purine rich foods
• NSAIDs –
– 1 st line = indometacin, diclofenac, naproxen
– Azapropazone
– Etoricoxib 120mg daily
Treatment
84
Treatment alternatives
• Colchicine
– in patients with peptic ulcer disease / heart failure / CIs to NSAIDs /
HTN
– can be combined with anticoagulation
– does not cause fluid retention
– Dose is 1 mg, then 500 mcg every 2-3 hours until the pain resolves, or the patient develops diarrhoea, or a total dose of 6mg has been taken. Treatment with colchicine should not be repeated within 3 days.
– Common side effects are diarrhoea and gastric irritation.
• Steroids – tapering oral dose / IM injection / intra-articular
(large joint)
85
If not subsiding in 12-24h, reconsider diagnosis
86
Gout
• Disorder of purine metabolism
• Characterized by acute, recurrent attacks of synovitis due to urate crystal deposition
• Leads to cartilage degeneration
• Most common in men (20:1) and in post-menopausal women
87
• Primary (95%) – inherited discorder that causes overproduction/underexcretion. Underlying biochem defect unknown
• Secondary
– Increased formation uric acid
– Reduced excretion
– Drugs/toxins
– Misc
88
The great toe demonstrates extensive juxta-articular erosions with soft tissue swelling and little osteoporosis
89
Chronic gout
• Frequent recurrence of acute attacks of gout, the presence of tophi, or signs of chronic gouty arthritis may call for the initiation of longterm (‘interval’) treatment
• 2 choices:
– xanthine-oxidase inhibitors
– uricosuric drug – sulfinpyrazone, probenecid, benzbromarone
90
Allopurinol
• Xanthane oxidase inhibitor
• Reduces synthesis of uric acid
• Can precipitate an attack - give NSAID/colchicine concomitantly for first 3 months
• Do not commence during acute attack – can prolong. Start 1-2 weeks later.
• Can cause rashes
91
Febuxostat
• Licensed for the treatment of chronic hyperuricaemia where urate deposition has already occurred
• 80mg once daily
• for patients who are intolerant of allopurinol or for whom allopurinol is contra-indicated
92
Age
Sites affected
Clinical features
Radiological features
Crystal deposition
Treatment
Gout vs. pseudogout
Pseudogout Gout
Patients tend to be over
40
Small joints
Elderly
Severe joint pain & swelling
Soft tissue swelling (not seen until 6-12 yrs after initial attack)
Uric acid
Large joints (most commonly the knee)
Moderate joint pain & swelling
Chondrocalcinosis calcification of articular cartilage menisci
Calcium pyrophosphate
Rest, NSAIDs,
?allopurinol
Rest NSAIDs, joint aspiration
93
• hyperparathyroidism
• haemochromotosis
• diabetes mellitus
• Wilson's disease
• ochronosis
• hypophosphataemia
• oxalosis
• osteoarthritis
• gout
• dialysis
• long-term steroid therapy
• acromegaly
Pseudogout associations
94
MISC
Sukhvans Sandhu
95
Case 1
• A 26 yr old woman c/o painful blue discolouration of her fingers on exposure to cold temperatures.
• She recalls having such episodes as a child but noted that they became more frequent when she moved to the coast.
• On recent outdoor walks she has felt increasing pain in her fingers and watched as they turned white, then blue, and finally became red and swollen.
• Once her hands were warm again they returned to normal. On examination nil significant .
96
Raynauds
•
Pathogenesis : Exaggerated vasoconstriction of arteries and arterioles [usually hand and feet]
• Causes : Mostly idiopathic, cold, emotions
97
• Symptoms:-
– Pain within the affected extremities
– Discolouration [white, blue, red]
– Sensation of cold and numbness
• Prevalence
– More common in women than men
Raynauds cont.
98
Primary Raynauds
• Primary Raynauds disease:-
– Reflects exaggeration of central and local vasomotor responses to cold or emotional stresses.
– Course of Raynauds is usually benign, however when long-standing can result in:-
• Atrophy of the skin, subcutaneous tissue and muscles
• Ulceration and ischaemic gangrene [rare]
99
Secondary Raynauds
• Secondary Raynauds
– Refers to a vascular insufficiency of the extremitites secondary to arterial disease:-
• Connective tissue disorders: SLE, sceleroderma [Specificsystemic sclerosis- CREST]
• Obstructive disorders: Atherosclerosis, Buerger disease
• Drugs: b-blockers, sulfasalazine
• Occupation: jobs involving vibration
• Raynauds may be the first manifestation of such conditions so be ready to consider.
100
Treatment
• General care:-
– Avoid triggers e.g. cold, vibration, emotional stress
– Keep hands and feet warm- mittens, insulated foot wear.
– Quit smoking
– Avoid caffeine
• Drug therapy
– Medicines that dilate blood vessels
– Calcium channel antagonists [Nifedipine or diltizem] – headache, flushing, ankle oedema
– Fluoxetine [SSRI] reduce frequency if associated with emotional trigger.
• Surgical – may require sympathectomy; botox
101
• The most common cause of Raynaud's Phenomenon is?
A. Idiopathic
B. Rheumatoid arthritis
C. Scleroderma
D. Systemic Lupus Erythematosus
E. Through the use of vibrating tools or machinery
102
• Raynaud's disease is a recognised feature of:-
A. Cervical rib
B. Scleroderma
C. Buergers disease
D. Diabetes mellitus
E. SLE
103
Case 2
• A 45yr old woman presents with bilateral painful and deformed
DIP joints. She also states that over the past few weeks that her eyes appear red. Further examination reveals discolourisation and onycholysis of the nails.
104
Psoriatic arthritis
• Is a type of inflammatory arthritis
• Affects around 10-30% of people suffering from the skin condition psoriasis
• Seronegative spondyloarthropathy
• App 80% of patients with psoriatic arthritis will have psoriatic nail lesions
• Can occur at any age
• Occurs app 10yrs after the first signs of psoriasis
• Men and women equally affected
105
Psoriatic arthritis cont.
• Presentation:-
– Causes joint, ligament inflammation
– Sausage-like swelling of digits [dactylitis]
– Joint stiffness [worst in morning; resting]
– Skin rash of psoriasis
– Pitting of nail
106
Types of psoriatic arthritis
• Asymmetric : 70% of cases.
• Symmetric : 25% of cases. Affects joints on the same side of the body simultaneously.
• Arthritis mutilans : <5% of cases. Severe deforming and destructive artritis
• Spondylitis : Characterised by stiffness of the neck or spine.
• DIP predominant : 5% of cases. Inflammation and stiffness in the DIP joints.
107
Treatment
• Underlying process of psoriatic arthritis is inflammation control inflammation
– First line: NSAIDs [ibuprofen, diclofenac]
– Joint injections [corticosteroids]
– Second line: If NSAID and/or steroids not working need immunosupressants:-
• Methotrexate, Leflunomide
Adv: immunosupressant treatment [covers arthropathy and psoriasis].
Severe cases: a-TNF agents e.g. inflixamab [reserved for the most severe cases.
108
• Psoriatic arthropathy is associated with which ONE of the following features:-
• A. A preceding history of skin lesion in the majority of patients
• B. Non involvement of the DIP joints
• C. Subcutaneous nodules
• D. Gallstone in the majority of patients
• E. The development of some evidence of joint involvement in the majority of patients with psoriasis
109
• In psoriatic arthropathy:-
• A. HLA B27 is associated with spondylitis.
• B. Arthritis mutilans is the most common pattern
• C. Onychopathy (nail pitting, ridging or onycholysis) is frequently associated with disease of the adjacent DIP joint.
• D. The severity and extent of synovitis is proportional to the extent of the psoriasis.
• E. Sulfasalazine might improve both psoriasis and arthritis.
110
THANKS
111