EU - BEANISH LAUNCHING CEREMONY DAR ES SALAAM

HIS implementation in
Ethiopia: case studies from AAHB
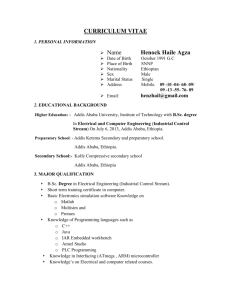
Woinshet Abdella
PhD Student
Department of Informatcs
University of Oslo
CONTENTS
Background
• Ethiopia / Health Care System
HISP Ethiopia
DHIS Implementation in Addis &
Oromia
Challenges
Ethiopia
Population - 72+ million
Area – 1.1 million km 2
Decentralized administrative structure
• 9 regional states & two city administrations
580 weredas (districts)
Regional sates are autonomous
Poor literacy, education, health status
Health Care System
MOH, Regional health bureaus, Zonal health departments, Wereda/Sub-city health offices, Health Facilities
Under developed
Health service coverage – 61%
MMR – 871/100,000, U5MR – 140/1000
High Infectious & communicable diseases
HIS is primarily manual & under developed
HISP-Ethiopia
Project Initiation
• Through a collaboration of the
Department of Information Science,
Addis Ababa University (AAU) and the
University of Oslo in February 2003.
Partners
• AAU; regional health bureaus of
Ethiopia; global HISP
HISP-Ethiopia
Objective
• Introducing computer based HMIS in
Ethiopia in view of supporting local analysis and use of data
HISP-Ethiopia
HISP Members
• 4 PhD students / 7 Masters students
(one Norwegian)
• 5 DHIS facilitators hired by HISP
Research Sites for HISP Ethiopia
• Addis Ababa, Oromia, Tigray, Amhara,
Benishangul-Gumuz
DHIS implementation is being carried out
• Addis & Oromia – since Jan 04
• Others – since June 04
Different stages of implementation
Case Studies from Addis
Research Objective
• key research objective is to broadly understand the challenges and opportunities with respect to the integration of existing paper-based HIS with computerbased systems in Ethiopia.
Theoretical Perspective
• ANT
Research Approach & context
• PAR
AR intervention:
HIS implementation Intervention into health organizations
(AAHB & OHB)
One DHIS facilitator for each region
Research Approach & context
Research Site
• Addis Ababa health bureau (AAHB) ,
• 10 sub-cities (districts)
• 500 public & private health facilities,
• located in Addis Ababa city
Administration (Province).
• Addis Ababa is the capital city of
Ethiopia (540 km2 )
• Population is 3 millions.
Research Approach & context
Researcher Role.
• The role assumed was an involved researcher through action research.
• Qualitative data collection method was employed including
photography, observations, interviews, discussions, meetings, workshops, training, action experiments, document analysis, telephone calls, visit related institutions, informal lunch/tea meetings.
Research Approach & context
Research subjects
• managers and planners at different levels of the health structure, the health workers responsible in data collections and analysis.
DHIS Implementation in Addis
Negotiate research access (KK)
Situation analysis (Mar 03 – Aug 03)
• Visits to Health bureaus & HFs
Initiating the Design / implementation process with
AAHB/OHB (Dec 03) (Bureau)
EPR was just introduced then
Prototype system was developed and populated with 9 months own data
DHIS Implementation in Addis
Ababa
Demonstration of the prototype DHIS
Addis (Jan 04)
• The experiences gained revealed the problems with the existing HMIS
Data duplication, fragmentation, …
• Local requirement (Morbidity/Mortality data handling) identified that DHIS does not support efficiently
Developing minimum health data set
& health indicators was proposed
DHIS Implementation in Addis
Ababa
Major decisions
• The proposal for standardizing data set/health indicators accepted
• Adapting DHIS based on new dataset and reporting requirement
• Adding module to accommodate M/M data handling
• Implementing DHIS to ALL Sub-cities.
Team formed
The research team was composed of
Bureau level ,
• Bureau head;
• health service head (leader of the project on the part of the bureau), team leader, and senior expert;
• family health head, team leader and expert;
• Disease Prevention and Control head; IDSR team leader, TB /
Leprosy and HIV/Aids program team leader and senior expert;
• IEC expert;
• Network administrator;
Sub-city Level
• two family health experts
Facility Level
• two health facility managers;
And the researcher.
DHIS Implementation in Addis
Ababa
Two Parallel activities performed
• Standardized data set, health indicators, data collection & reporting instruments & procedures (data flow, …) development
Draft prepared by the group presented for workshops, comments incorporated, the draft was further developed in a series of long meetings,
• Development of Morbidity & Mortality module
Iterative / incremental (involved one major revision)
DHIS Implementation in Addis
Ababa
Use of DHIS as a prototyping tool
to better understand user requirements for producing an improved & useful system – which potentially increases data use
The standardized data set is implemented in all facilities
DHIS adapted, the new module incorporated
• ( Input Form , DHIS Data Flow , Data Entry (next slide), Pivot
Table Report , Standard Report )
Monthly Routine
Data Entry/Edit
Form
Monthly Morbidity and Mortality Data
Entry/Edit Form
DHIS Implementation in Addis
DHIS is implemented
• All districts (10 sub-cities) and AAHB initially
• Scaled to health facility levels
18/23-Health centers & 5/5-Hospitals (when resource / situation allowed )
Training (DHIS/computer basics) was given to sub-city/bureau/HF health staff / managers / data clerk / DHIS facilitators (with own data)
Technical support is being provided by the facilitator
Participatory design
July 2005, Workshop for evaluating one year experience of the use DHIS
Observations …
DHIS Software is well-tested & supports
• Data aggregation; data sharing; health structure implementation; easily adaptable for new needs, which is inevitable; rapid set-up of
DHIS application for a new setting
Complaints from different actors (use of
MS Access in DHIS – DHIS 2 is a response)
DHIS Implementation in Oromia
Collection/reporting instruments and software prepared for Addis is shared by
Oromia & other regions
Followed similar approach
• Some of the differences
The process was slower when compared to Addis
The minimum data set prepared for Oromia not yet adopted by the region
DHIS implementation status
• Some Weredas of East Shewa zone (based on computer availability)
• Is being rolled out to the remaining zones (at the zone level only)
CHALLENGES
Improving data quality, data analysis and use
Reduce / Improve dataset
Achieving partnership with MOH
Scaling & Sustainability
Over burdened health worker
Limited resource
Negotiating with multiple actors
Parallel systems