Opiods in Organ Failure
advertisement

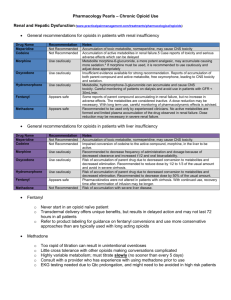
OPIOIDS IN ORGAN FAILURE MELLAR DAVIS, WAEL LASHEEN, DECLAN WALSH END STAGE LIVER DISEASE SICK CELL THEORY REDUCED HEPATOCYTE FUNCTION, SPARED BLOOD FLOW INTACT HEPATOCYTE THEORY WELL FUNCTIONING RESIDUAL HEPATOCYTES, REDUCED NUMBERS IMPAIRED DRUG UPTAKE THEORY LOSS OF FENESTRATION IN SINUSOIDAL ENDOTHELIUM, DEVELOPMENT OF BASAL LAMINA IN SPACE OF DISSE BLOCK IN DIFFUSION 2 FACTORS INFLUENCING DRUG KINETICS IN LIVER DISEASE HIGH VS. LOW EXTRACTION RATIO FIRST PASS CLEARANCE SHUNTING ALBUMIN VS. ALPHA1 ACID GLYCOPROTEIN BINDING TYPE I VS. TYPE II METABOLISM 3 FENTANYL LOW ORAL BIOAVAILABILITY, HIGH FIRST PASS CLEARANCE LIPOPHILIC WITH RAPID CNS PENETRATION SUBJECT TO: PULMONARY SEQUESTRATION PRIOR TO CNS EFFLUX PUMPS LARGE VOLUME OF DISTRIBUTION SEQUESTRATION IN MUSCLE FAT 4 FENTANYL METABOLIZED BY CYP3A4 SINGLE DOSE T ½ IS DUE TO REDISTRIBUTION STEADY STATE CLEARANCE LIMITED BY CYP3A4 ALBUMIN BOUND 5 FENTANYL IN RENAL DISEASE REDUCED CLEARANCE LATE UREMIA INHIBITS CYP3A4 REDUCED ALBUMIN IN NEPHROTIC SYNDROME ? LARGER VOLUME OF DISTRIBUTION T ½ = 0.693 VD/CL Vd CL VIA CYP3A4 6 FENTANYL IN RENAL DISEASE CLINICAL IMPORTANCE DO NOT START WITH A TRANSDERMAL PATCH TRANSDERMAL ABSORPTION MAY BE ALTERED DIALYSIS DOES NOT REMOVE FENTANYL 7 FENTANYL IN LIVER DISEASE REDUCED CLEARANCE IN LIVER DISEASE REDUCED ALBUMIN REDUCED CYP3A4 REDUCED HEPATIC BLOOD FLOW CLINICAL IMPORTANCE DO NOT USE PATCH IN ADVANCED LIVER DISEASE LOW DOSES, WATCH FOR DELAYED TOXICITY 8 HYDROMORPHONE MODERATE BIOAVAILABILITY (50-60%) LOW BINDING TO ALBUMIN (≤ 40%) CROSSES THE CNS SIMILAR TO MORPHINE GLUCURONIDATED TO HYDROM-3 GLUCURONIDE NEUROTOXIN GLUCURONIDE METABOLITE RENALLY CLEARED 9 HYDROMORPHONE IN RENAL DISEASE ACCUMULATION OF HYDROMORPHONE-3GLUCURONIDE INCREASES POTENTIAL FOR NEUROTOXICITY CLINICAL IMPORTANCE BETTER TOLERATED THAN MORPHINE IN RENAL FAILURE NEUROTOXICITY SUBJECT TO DIALYSIS 10 HYDROMORPHONE AND RENAL CLEARANCE GFR ml/min AUC relative to normal >60 1 40-60 2 <30 4 11 HYDROMORPHONE IN LIVER DISEASE GREATER BIOAVAILABILITY DUE TO SHUNTING MINOR INFLUENCE ON PHARMACOKINETICS RELATIVE SPARING OF GLUCURONIDATION ALBUMIN LEVELS HAVE LITTLE INFLUENCE ON UNBOUND DRUG 12 HYDROMORPHONE IN LIVER DISEASE CLINICAL IMPORTANCE INCREASED ORAL BIOAVAILABILITY RELATIVELY SPARED T ½ START WITH LOWER THAN NORMAL DOSES, MAINTAIN INTERVALS AVOID SUSTAINED RELEASE HYDROMORPHONE 13 MORPHINE ORAL BIOAVAILABILITY OF 30% (15-50%) 1/3 ALBUMIN BOUND SUBJECT TO EFFLUX PROTEINS METABOLIZED GLUCURONYL TRANSFERASES UGT B > UGT 1A1, UGT 1A3 ENTEROHEPATIC RECIRCULATION GLUCURONIDES CLEARED BY KIDNEYS 14 MORPHINE IN RENAL FAILURE ACCUMULATION OF MORPHINE TO GLUCURONIDE DELAYED OPIOID TOXICITY ACCUMULATION OF MORPHINE 3 GLUCURONIDE DELAYED NEUROTOXICITY HEMODIALYSIS BUT NOT PERITONEAL DIALYSIS REMOVES GLUCURONIDE METABOLITES 15 MORPHINE IN RENAL FAILURE CLINICAL IMPORTANCE: DOSE REDUCTION EXTEND INTERVALS AVOID SUSTAINED RELEASE PRN SCHEDULE AS INITIAL DOSING STRATEGY HEMODIALYSIS RELATED CHANGES IN ANALGESIA 16 DOSE REDUCTION FOR GFR GFR (ml/min) Morphine (%) Methadone (%) 20-50 75 100 10-20 50 100 <10 25 50 17 MORPHINE CLEARANCE IN LIVER DISEASE MORPHINE T ½ IS PROLONGED WITH: ALTERED CLOTTING TIMES PRESENCE OF ASCITES HISTORY OF ENCEPHALOPATHY 18 MORPHINE IN LIVER DISEASE INCREASED BIOAVAILABILITY RELATIVELY SPARED T ½ LITTLE INFLUENCE OF HYPOALBUMINEMIA CLINICAL IMPORTANCE START AT LOWER THAN USUAL DOSES MAINTAIN INTERVALS AVOID SUSTAINED RELEASE IN ADVANCED CIRRHOSIS 19 OXYCODONE ORAL BIOAVAILABILITY 60% ALBUMIN BOUND 40% ACTIVELY TRANSPORTED INTO CNS PLASMA/BRAIN RATIO 3 METABOLIZED BY CYP2D6, CYP3A4 OXYMORPHONE NOROXYCODONE METABOLITES ± OXYCODONE CLEARED BY KID. 20 OXYCODONE IN RENAL DISEASE ↑ NOROXYCODONE & OXYMORPHONE HALF-LIFE OF OXYCODONE IS LENGTHENED CNS TOXICITY AT NORMAL DOSES CLINICAL IMPORTANCE START AT REDUCED DOSES DO NOT USE SUSTAINED RELEASE OXYCODONE USE PRN TO FIND CORRECT INDIVIDUAL DOSING INTERVAL 21 OXYCODONE IN LIVER DISEASE MAXIMUM CONCENTRATION INCREASES 40%, AUC 90% IMMEDIATE RELEASE T ½ GOES FROM 3.4 TO 14 HOURS (4.6-24) HYPOALBUMINEMIA PLAYS A MINOR ROLE CLINICAL IMPORTANCE DO NOT USE SUSTAINED RELEASE OXYCODONE LENGTHEN INTERVALS BETWEEN DOSES USE A PRN TO FIND INDIVIDUAL INTERVALS 22 METHADONE ORAL BIOAVAILABILITY 80% LOW FIRST PASS CLEARANCE BINDS TO ALPHA1 ACID GLYCOPROTEIN CROSSES THE BBB (EFFLUX PROTEINS) METABOLIZED BY MULTIPLE CYTOCHROMES CYP3A4, CYP3A5, CYP2B6, CYP2D6, CYP1A2 INACTIVE METABOLITE 23 METHADONE IN RENAL DISEASE INACTIVE METABOLITE FECAL EXCRETION MULTIPLE CYTOCHROME METABOLISM CLINICAL IMPORTANCE: RELATIVELY SAFE IN RENAL FAILURE 24 METHADONE IN LIVER DISEASE BOTH METHADONE AND METABOLITES ARE EXCRETED IN FECES VS. URINE T ½ IS PROLONGED IN SEVERE LIVER DISEASE (20 HRS TO 32 HRS) HEPATITIS C STIMULATES CYP3A4 COMPENSATE FOR REDUCED CYTOCHROMES 25 SUMMARY OPIOIDS USED IN LIVER FAILURE / CIRRHOSIS MORPHINE HYDROMORPHONE ? LEVORPHANOL ? BUPRENORPHINE 26 SUMMARY OPIOIDS USED IN RENAL FAILURE METHADONE ? FENTANYL BUPRENORPHINE HYDROMORPHONE > MORPHINE 27 28 Case History 1 • 42 year old male with hepatitis C with hepatocellular carcinoma and abdominal pain from hepatic capsular invasion • Physical Examination: no ascites, mild palm erythema, no asterixis • Laboratory: albumin 3.0 mg /dl, PT INR 1.3 29 Case History 1 Treatment • Acetaminophen 1000 mg 4 times daily • Naproxen 5000 mg 3 times daily • Oxycodone 5 mg every 4 hours ATC • Morphine 5 mg every 4 hours ATC • Transhepatic arterial embolization • Celiac block 30 Case History 1 • He sustains a portal vein thrombosis and develops ascites • His pain escalates to a 7(NRS) unrelieved by oxycodone 5 mg every 4 hours • Laboratory: Bilirubin 2mg /dl, Albumin 2.8, PT-INR 1.6, Creatinine 1 mg /dl 31 Case History 1 Treatment • Fentanyl Transdermal at 50 mcg /h • Oxycodone Sustained Release 20 mg twice daily and 5 mg of immediate release every 2 hours as needed • Morphine 1 mg /h IV continuous with 1 mg q2 hours as needed • Methadone 5 mg every 3 hours as needed • Titrate the immediate release oxycodone and avoid the sustained release • Trans-hepatic embolization 32 Case History 1 • He is on morphine 1 mg/h continuous infusion, but has developed asterixis, visual hallucinations and tactile hallucinations • Pain is 5 by NRS • Laboratory: Bilirubin 3mg /dl, PT-INR 2, Creatinine 2.2mg/dl 33 Case History 1 Treatment • Reduced morphine to 0.5 mg /h and add naproxen • Switch to methadone • Switch to buprenorphine • Switch to continuous fentanyl at 25 mcg /h • Celiac block • Oxycodone 5 mg every 4 hours by mouth 34 REFERENCES Davis M. Cholestasis and Endogenous Opioids. Clin Pharmacokinet 2007 46:825-850. Tegeder I, Lotsch J, Geisslinger G. Pharmacokinetics of Opioids in Liver Disease. Clin Pharmacokinet 1999; 37:17-40. Volles D, McGory R. Perspectives in Pain Management. Critical Care Clinics 1999;15. Rhee C, Broadbent AM. Palliation and Liver Failure: Palliative Medications Dosage Guidelines. J Pall Med 2007;10:677-685. 35 ADJUVANT ANALGESICS 36 37 ADJUVANT ANALGESICS ANY DRUG WITH A PRIMARY INDICATION OTHER THAN PAIN BUT WITH ANALGESIC PROPERTIES IN SOME PAINFUL CONDITIONS CO-ADMINISTSERED WITH CLASSICAL ANALGESICS (ACETAMINOPHEN, NSAIDS, OPIOIDS) CO-ANALGESIC ARE SOMETIMES USED SYNONYMOUSLY FOR ADJUVANT ANALGESIC 38 ADJUVANT ANALGESIC ARE ADDED TO OPIOIDS TO: ENHANCE ANALGESIA ALLOW OPIOID DOSE REDUCTION FIRST LINE DRUGS FOR NON MALIGNANT PAIN MISNOMER IF DRUG USED AS FIRST LINE 39 OPIOIDS VS. ADJUVANTS OPIOIDS LACK OF END ORGAN DAMAGE LACK OF “CEILING” DOSE VERSATILITY (MULTIPLE ADMINISTRATION ROUTES) ADJUVANTS POTENTIAL FOR END ORGAN DAMAGE “CEILING” DOSE LIMITED VERSATILITY (FOR MOST) 40 OPIOIDS VS. ADJUVANTS OPIOIDS NO “THERAPEUTIC” LEVEL ANALGESIC TOLERANCE WIDE DIFFERENCES IN EQUIANALGESIA BETWEEN INDIVIDUALS DUE TO PHARMACOGENOMICS ADJUVANTS THERAPEUTIC PLASMA LEVELS LACK OF ANALGESIC TOLERANCE CONSISTENT EQUIANALGESIA 41 OPIOIDS VS. ADJUVANTS OPIOIDS PSYCHOLOGIC DEPENDENCY RISK CHANGE IN THERAPEUTIC INDEX WITH CONVERSION (ROUTE CHANGE) EFFICACY UNRELATED TO TYPE OF PAIN PRESCRIPTION RESTRICTIONS (LEGAL) ADJUVANTS RELATIVE LACK OF PSYCHOLOGIC DEPENDENCE LACK OF BENEFIT TO ROUTE CHANGE, THERAPEUTIC INDEX REMAINS UNCHANGED EFFICACY GENERALLY LIMITED TO EITHER NOCICEPTIVE OR NEUROPATHIC PAIN RELATIVELY FREE OF LEGAL RESTRICTION 42 OPIOIDS VS. ADJUVANTS OPIOIDS WITHDRAWAL SYNDROME WITH CHRONIC USE RESPONSES BETWEEN OPIOIDS DIFFER (NONCROSS TOLERANCE) PERIPHERAL AND CENTRAL ACTION DOSES LIMITED BY SIDE EFFECTS ADJUVANTS WITHDRAWAL SYNDROME DEPENDS UPON ADJUVANT NON-CROSS TOLERANCE BETWEEN CLASSES (NSAIDs, ANTI-SEIZURE MEDICATIONS) PERIPHERAL AND CENTRAL ACTION DOSES LIMITED BY LACK OF RESPONSE AT THERAPEUTIC LEVELS AND END-ORGAN FAILURE 43 ADJUVANT ANALGESIC STRATEGY OPTIMIZE OPIOID DOSING AND SCHEDULE BEFORE ADDING AN ADJUVANT CONSIDER OTHER TECHNIQUES FOR PAIN CONTROL OPIOID ROTATION OPIOID CONVERSION ROUTE TREATMENT OF SIDE EFFECTS FROM OPIOIDS NON-PHARMACOLOGIC APPROACHES 44 ADJUVANT ANALGESIC STRATEGY SELECT ADJUVANTS BASED UPON PAIN MECHANISM AND PATIENT CO-MORBIDITY PRESCRIBE AN ADJUVANT BASED UPON PHARMACOLOGICAL CHARACTERISTICS, INDICATIONS (APPROVED AND UNAPPROVED) SIDE EFFECT PROFILE, DRUG INTERACTIONS, VERSATILITY AND COST 45 ADJUVANT ANALGESIC STRATEGY USE THE ADJUVANT WITH THE BEST BENEFIT TO RISK PROFILE DO NOT INITIATE SEVERAL ADJUVANTS AT ONCE START LOW AND TITRATE TO RESPONSE REASSESS RESPONSE AND TAPER TO EFFECT CONSIDER COMBINING ADJUVANTS IN DIFFICULT PAIN (COMPLIMENTARY ACTIONS) 46 ADJUVANT SELECTION CHOICES ARE NOT BASED UPON EVIDENCE OF DIFFERENTIAL EFFICACY BUT: TYPE OF PAIN SEVERITY OF PAIN (PAIN INTERFERENCE) ADDITIONAL SYMPTOMS (DEPRESSION, ANOREXIA) CO-MORBIDITY (HEART FAILURE, DEMENTIA, RENAL DYSFUNCTION) 47 ADJUVANT ANALGESICS FEW EVIDENCE BASED STUDIES IN CANCER BASED ON EXPERIENCE IN NON-MALIGNANT PAIN 48 CALCIUM CHANNEL BLOCKERS GABAPENTIN CANNABINOIDS ZICONOTIDE 49 SODIUM CHANNEL BLOCKERS CARBAMAZEPINE PHENYTOIN/PHENOBARBITAL TRICYCLIC ANTI-DEPRESSANTS MEXILITINE LIDOCAINE LAMOTRIGINE 50 MONOAMINE REUPTAKE INHIBITORS TRICYCLIC ANTI-DEPRESSANTS SELECTIVE SEROTONIN REUPTAKE INHIBITORS ATYPICAL ANTI-DEPRESSANTS – VENLAFAXINE, MIRTAZAPINE, DULOXETINE 51 GABA AGONISTS CLONAZAPINE VALPROIC ACID 52 NMDA INHIBITORS KETAMINE AMANTADINE MEMANTINE LEVORPHANOL METHADONE DEXTROMETHORPHAN MAGNESIUM 53 MISCELLANEOUS CANNABINOIDS CLONAZEPAM PSYCHOSTIMULANTS EMLA CAPSAICIN 54 SUMMARY ADJUVANTS POTENTIATE OPIOID ANALGESIA OPIOID “SPARING” OPIOID DOSING AND SCHEDULE SHOULD BE OPTIMIZED BEFORE ADDING AN ADJUVANT ANALGESIC 55 SUMMARY CHOICE OF AN ADJUVANT BASED UPON TYPE AND SEVERITY OF PAIN SYMPTOMS OTHER THAN PAIN THERAPEUTIC INDEX DRUG INTERACTIONS EFFICACY AND COST 56 Case History 1 • 42 year old male with hepatitis C with hepatocellular carcinoma and abdominal pain from hepatic capsular invasion • Physical Examination: no ascites, mild palm erythema, no asterixis • Laboratory: albumin 3.0 mg /dl, PT INR 1.3 57 OPIOID ROTATION 58 OPIOIDS A MINORITY OF INDIVIDUALS DEVELOP UNCONTROLLED AND RATE-LIMITING SIDE EFFECTS DURING TITRATION WITH MORPHINE AGGRESSIVE ATTEMPTS TO PREVENT AND TREAT ADVERSE EFFECTS SHOULD BE MADE BEFORE ROTATION IS CONSIDERED 59 DIFFERENT OPIOIDS ARRAY OF G PROTEINS ACTIVATION DIFFERENT OPIOID RECEPTORS INTRINSIC EFFICACY RECEPTOR DESENSITIZATION AND TRAFFICKING TYPE OF MU RECEPTOR SUBTYPES 60 DIFFERENT METABOLIC PATHWAY CYTOCHROMES: CYP1A2, CYP2D6, CYP3A4 CONJUGASES: UGT1A3, UGT1A1, UGT2B7 CYP2D6 ACTIVATES CODEINE AND TRAMADOL UGT2B7: MORPHINE TO M-6G 61 OPIOID EFFICACY FRACTIONAL RECEPTOR OCCUPANCY TO PRODUCE RELIEF RELATED TO ABILITY TO ACTIVATE RECEPTOR LEADS TO CHANGES IN EQUIVALENTS WITH PAIN SEVERITY AND AT HIGH DOSES LESS SHIFT IN DOSE RESPONSE CURVES WITH HIGH INTRINSIC EFFICACY OPIOIDS 62 HIGH INTRINSIC EFFICACY OPIOIDS FENTANYL METHADONE SUFENTANIL 63 OPIOID ROTATION OPIOID RESPONSIVENESS IS HIGHLY VARIABLE BETWEEN INDIVIDUALS OPIOID RESPONSIVENESS NOT TO BE JUDGED ON ANALGESIC RESPONSE TO ONE OPIOID INADEQUATE PAIN RELIEF AND DOSE LIMITING SIDE EFFECTS 64 INDICATION FOR OPIOID ROTATION 39% COGNITIVE FAILURE 24% HALLUCINATIONS 16% UNCONTROLLED PAIN 11% MYOCLONUS 9% NAUSEA 1% LOCAL IRRITATION 65 ALTERNATIVE: SWITCHING ROUTES MORPHINE ROUTE CHANGE: ALTERS METABOLISM REDUCES NEUROTOXIC METABOLITES REDUCES MYOCLONUS 3-FOLD 66 ROUTE CONVERSION (STEADY STATE) ORAL PARENTERAL MORPHINE 3 1 HYDROMORPHONE 2 1 METHADONE 2 1 OXYCODONE 2 1 67 SUBLINGUAL OPIOIDS: ROUTE CONVERSION FENTANYL METHADONE BUPRENORPHINE ? 1:2 (1:3) 1:2 68 TRANSDERMAL OPIOIDS: ROTATION MORPHINE EQUIVALENT FENTANYL 100:1 BUPRENORPHINE 110:1 69 OPIOID ROTATION PREDOMINATELY FOR PAIN USE 100% EQUIVALENTS PREDOMINANTLY FOR SIDE EFFECTS USE 50-70% EQUIVALENTS 70 OPIOID ROTATION EQUIVALENTS OPIOID EQUIVALENTS MORPHINE 1:1 HYDROMORPHONE 1:5 OXYCODONE 1:1 (1:1.5) FENTANYL METHADONE 1:100 (TD/IV) <90 1:4 >90 <300 1:8 >300 <1000 1:12 >1000 1:20 71 OPIOID ROTATION EQUIVALENTS 1 OPIOID OPIOID EQUIVALEN T HYDROMORPHINE (IV) METHADONE (PD) 1.14:11 FENTANYL (TD) METHADONE (PD) 1:17-20 FENTANYL (TD) BUPRENORPHINE (TD) 1:1.1 DOSE DEPENDENT 72 OPIOID ROTATION PITFALLS OTHER CAUSES OF COGNITIVE FAILURE, HALLUCINATIONS, MYOCLONUS AND NAUSEA DELAYS IN SIDE EFFECT RESOLUTION WHICH MAY BE ATTRIBUTED TO THE SECOND OPIOID ORGAN FAILURE WILL CHANGE EQUIVALENTS DRUG INTERACTION WILL CHANGE EQUIVALENTS 73 OPIOID ROTATION PITFALLS BI-DIRECTIONAL DIFFERENCES IN EQUIVALENTS WITH ROUTE CONVERSION AND ROTATION METHADONE ORAL TO IV: 1:2 METHADONE IV TO ORAL: 1:1 HYDROMORPHONE TO MORPHINE: 1:3.7 MORPHINE TO HYDROMORPHONE: 5:1 74 SUMMARY OPIOID ROTATION TO RE-ESTABLISH PAIN CONTROL RESOLVE SIDE EFFECTS IN THE MAJORITY NON-CROSS TOLERANCE EQUIVALENT TABLES ARE GUIDELINES 75 SUMMARY DOSES ADJUSTED BASED ON CLINICAL CONTEXT 50-70% EQUIVALENCE FOR SIDE EFFECTS ADJUSTMENT ANALGESICS CAN BE “OPIOID SPARING” ALLOW DOSE REDUCTION AND RESOLVE TOXICITY 76 SUMMARY METHADONE ROTATIONS ARE UNIQUE; SHOULD BE DONE BY EXPERIENCED CLINICIAN ROUTE CHANGES ALTERNATIVE TO ROTATION BASED LARGELY ON ORAL BIOAVAILABILITY 77