Powerpoint
advertisement
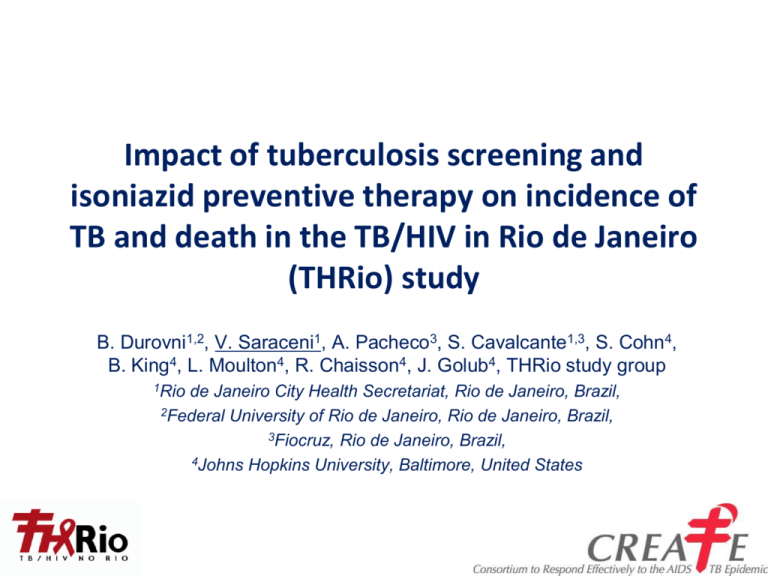
Impact of tuberculosis screening and isoniazid preventive therapy on incidence of TB and death in the TB/HIV in Rio de Janeiro (THRio) study B. Durovni1,2, V. Saraceni1, A. Pacheco3, S. Cavalcante1,3, S. Cohn4, B. King4, L. Moulton4, R. Chaisson4, J. Golub4, THRio study group 1Rio de Janeiro City Health Secretariat, Rio de Janeiro, Brazil, 2Federal University of Rio de Janeiro, Rio de Janeiro, Brazil, 3Fiocruz, Rio de Janeiro, Brazil, 4Johns Hopkins University, Baltimore, United States THRio Objectives • To determine if implementation of a policy of widespread use of isoniazid preventive therapy (IPT) in HIV-infected patients with access to ARV therapy reduces the incidence of active TB and death in the HIV clinic population • Scale up of tuberculin skin testing (TST) and IPT among HIVinfected patients in public primary health units in Rio de Janeiro within the current HIV clinic infrastructure – In an effort to reduce: • TB Incidence • Mortality THRio Study Design and Timeline Cluster-Randomized, Step-Wedge Trial Intervention and Follow-up Period (for all clinics) 48 Sep 05 Jan 08 60 Aug 09 4 Intervention • Training clinics to properly implement TB screening and adhere to TST/IPT policy for all HIV-infected patients • TST to be done for all eligible clinic patients – No prior TB history – No prior IPT – No prior +TST • IPT x 6 months for all TST+ without active TB and all contacts of active TB cases 5 TST and IPT • 69% had at least one TST placed and read • 83% started IPT • 0.84% had an adverse event • 84% completed IPT Time to TST and Time to IPT Before and After THRio Intervention • Time to TST and time to IPT are both markedly improved post-intervention Time to IPT 1.0 Time to PPD 0.2 0.4 Proportion with no IPT 0.6 0.8 1.0 0.8 0.6 0.4 0.0 0.2 0.0 Proportion with no PPD Pre-intervention Post-intervention Pre-intervention Post-intervention 0 50 100 150 200 Weeks Durovni et al., AIDS 2010, 24 (suppl 5):S49–S56 0 50 100 Weeks 150 Methods for Current Analysis Primary endpoints: Incidence of TB and TB or death at the clinic level before and after the intervention Eligible patients who made > 1 visit after 1 Sept 2003 • ‘Eligible’ = no prior TB or IPT • ‘Prevalent’ TB and deaths (within 60 days of enrollment) excluded • Patients remain in the denominator until TB or Death Intent-to-treat Analysis – includes all eligibles “Stayers” Analysis -- among those remaining in clinic contact, censoring those missing for >1 year (mITT) Statistical analysis: Crude hazard ratios (HR) obtained from frailty-adjusted Cox models are presented CONSORT Diagram (modified for stepped wedge cluster-randomized trial) Clinics Eligible for Inclusion (n=29) Clinics Receiving Intervention (n=29) Patients in Clinics Eligible for Intervention (n=12,815) Eligible patients contributing to control phase (n=9,853 ) Patients in Clinics Ineligible for Intervention (n=4,480) Eligible patients contributing to intervention phase (n= 10,840) THRio cohort characteristics (n=12,815) • Median age: 37 years old • Male: 61% • Median years since HIV diagnosis: 2.4 years • HAART at entry: 60% • Median CD4 cell count at entry: 403 cells/mm3 THRio Results TB cases, total contribution time, incidence per 100pyrs Control Phase Cases Person years Rate/100pyrs Intervention Phase 221 254 16,834 23,126 1.31 1.10 TB/Death cases, total contribution time, incidence per 100pyrs Control Phase Cases Person years Rate/100pyrs Intervention Phase 617 696 16,834 23,126 3.67 3.01 THRio Results: Unadjusted Cox Models Intent To Treat Outcome Cases HR (95% CI) p-value TB 475 0.233 TB or Death 1313 0.87 (0.68-1.10) 0.72 (0.62-0.82) • Intent-to-treat – Among all eligibles <0.001 THRio Results: Unadjusted Cox Models Intent To Treat Modified Intent To Treat (Stayers) Outcome Cases HR (95% CI) p-value TB 475 0.233 TB or Death 1313 TB 403 TB or Death 1073 0.87 (0.68-1.10) 0.72 (0.62-0.82) 0.57 (0.44-0.76) 0.56 (0.47-0.66) <0.001 <0.001 <0.001 • Intent-to-treat – Among all eligibles • Stayers – mITT - Among those remaining in clinic contact (Patients censored at the moment they go one year without a clinic contact) Conclusions • Overall, the THRio intervention had a modest impact (13% reduction) on TB, but showed an important and statistically significant impact on TB and death (28% reduction) in the primary intent-to-treat analysis; • The “Stayers” analysis, including those who were more likely to be exposed to the intervention (mITT), showed an even larger and highly significant impact on reduction of TB incidence (43%) and TB incidence and death (44%) • TST screening and provision of IPT to HIV-infected patients with access to highly active antiretroviral therapy significantly reduces the risk of TB and death and should be widely implemented Rio de Janeiro • Betina Durovni • Solange Cavalcante • Valeria Saraceni • Antonio Pacheco • Giselle Israel • Vitoria Vellozo • Rita Ferreira • Lilian Lauria • THRio Study Team THRio Study Team JHU • Richard Chaisson • Jonathan Golub • Larry Moulton • Silvia Cohn • Bonnie King • Anne Efron • Susan Dorman Funding: Bill and Melinda Gates Foundation 16