Personality Disorders: Dr. Mark Johnston
advertisement

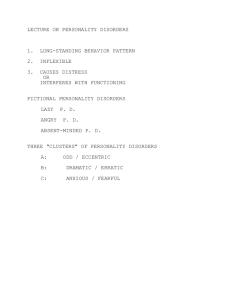
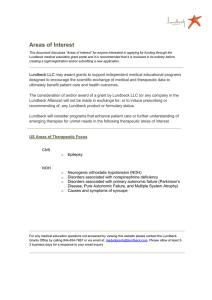
Personality Disorders Dr. Mark Johnston, MD, FRCPC Friday, 2 October, 2015 CFPC CoI Templates: Slide 1 Faculty/Presenter Disclosure • Faculty: Dr. Mark Johnston • Relationships with commercial interests: – Grants/Research Support: Otsuka, Roche, Merck, Lundbeck, Forum, Pfizer – Speakers Bureau/Honoraria: Pfizer, Lundbeck, Purdue, J&J, BMS – Consulting Fees: None. CFPC CoI Templates: Slide 2 Disclosure of Commercial Support • This program has received financial support from Lundbeck in the form of logistical support and educational grant. • Potential for conflict(s) of interest: – Dr. Mark Johnston has received NSCFP funding from Lundbeck CFPC CoI Templates: Slide 3 Mitigating Potential Bias • Medications are not approved for the treatment of PD’s • Some might be used off-label, but efficacy is limited AD Research Specific Personality Disorders CLUSTER A : Odd, Bizarre, Eccentric CLUSTER B : CLUSTER C : - Paranoid PD Dramatic, Emotional, Erratic - Antisocial PD Anxious, Fearful - Avoidant PD - Schizoid PD - Borderline PD - Dependent PD - Schizotypal PD - Histrionic PD - Obsessivecompulsive PD - Narcissistic PD Personality Disorders affect an average 10% of people Cluster A Paranoid Pervasive distrust of others, including friends, family, and partner Guarded and suspicious, constantly on the lookout for clues or suggestions to validate fears Strong sense of personal rights Withdraw from others and struggles with building close relationships Cluster A Schizoid Detached and aloof Prone to introspection and fantasy No desire for social or sexual relationships Indifferent to others and to social norms and conventions, and lacks emotional response Highly sensitive with a rich inner life Rarely present to medical attention (well functioning, untroubled by oddness) Cluster A Schizotypal Oddities of appearance, behavior, speech, and unusual perceptual experiences Anomalies of thinking similar to those seen in schizophrenia Odd beliefs, magical thinking, suspiciousness, obsessive rumination Fear social interaction; think others are harmful Ideas of reference (beliefs or intuitions that events and happenings are somehow related to them) Cluster B Antisocial More common in men than women Callous unconcern for the feelings or others Disregards social rules and obligations Irritable and aggressive, acts impulsively, lacks guilt, and fails to learn from experience No trouble finding relationships, but they are usually fiery, turbulent, and short lived Correlated with crime (criminal record, history of being in and out of prison) Cluster B Borderline Lacks sense of self, therefore experiences feelings of emptiness and fears of abandonment Pattern of intense, but unstable relationships, emotional instability, outbursts of anger and violence, and impulsive behavior Suicidal threats and acts of self harm (frequently seek medical attention) Sometimes results from childhood sexual abuse (more common in women) Cluster B Histrionic Lack a sense of self-worth; depend for their wellbeing on attracting the attention and approval of others Dramatizing (“playing a part”) May take great care of appearance and behave in a manner that is overly charming or seductive Crave excitement and act on impulse of suggestion Sensitive to criticism and rejection, and react badly to loss or failure Cluster B Narcissistic Extreme feeling of self-importance, entitlement, and need to be admired Envious of others and expects to be envied Lacks empathy and readily exploits others to achieve their aims To others, they may seem self-absorbed, controlling, intolerant, selfish, or insensitive If felt obstructed or ridiculed, they can fly into a fit of anger and revenge or rage Cluster C Avoidant Believe they are socially inept, unappealing, or inferior Constantly fear being embarrassed, criticized, or rejected Avoid meeting others, and restrained even in intimate relationships Experience anxiety May be associated with actual or felt rejection by parents or peers in childhood Excessively monitor internal reactions, both their own and those of others Cluster C Dependent Lack of self-confidence and excessive need to be looked after Needs help making everyday life decisions Fears abandonment; goes through considerable lengths to secure and maintain relationships See oneself as inadequate and helpless; submits to one or more protective others Naive and child-like perspective; limited insight into themselves and others Vulnerable to abuse and exploitation Cluster C Obsessive-compulsive Excessive preoccupation with details, rules, lists, order, organization, or schedules Perfectionism so extreme, it prevents a task from being completed Doubting and cautious, rigid and controlling, humorless, and miserly Underlying anxiety arises from lack of control over a world that eludes his understanding Little tolerance for complexity or nuance; sees things black and white (either all good or all bad) Relationships strained by unreasonable and inflexible demands that they make upon them Causes • Childhood abuse Causes • Social environment Causes • Problems in brain functioning Borderline 5 of the following 9 symptoms must be present: 1) Frantic efforts to avoid real or imagined abandonment 2) A pattern of unstable and intense interpersonal relationships characterized by altering between extremes of idealization and devaluation 3) Identity disturbance: Markedly and persistently unstable self image or sense of self 4) Impulsivity in at least two areas that are potentially selfdamaging (spending, sex, substance abuse, reckless driving, binge eating) Borderline Cont’d 5) Recurrent suicidal behavior, gestures, or threats, or selfmutilating behavior 6) Affective instability due to marked reactivity of mood (intense episodic dysphoria, irritability, or anxiety usually lasting a few hours and only rarely more than a few days) 7) Chronic feelings of emptiness 8) Inappropriate, intense anger or difficulty controlling anger 9) Transient, stress-related paranoid ideation or severe dissociative symptoms The Brain It has been show that brain regions that process negative emotions (for example, anger and sadness) are overactive in people with BPD, while brain regions that would normally help damp down negative emotions are underactive “I hate you, but don’t leave me” • People with BPD need to develop more comfort with their own emotions • They have so much anxiety they start to use projection: Form of defense Unwanted feelings or impulses are displaced onto another person (usually the counselor in this case) Denying their existence in themselves, while attributing them to others • Example: A person who is rude may constantly accuse others of being rude Continued As the Counselor : •Remain neutral •Constantly re-assuring them against their own fears is BAD •Ask them to judge whether there’s really anything to worry about •Offer emotional support, understanding, patience, and encouragement — change can be difficult and frightening to people with borderline personality disorder, but it is possible for them to get better over time Case Study Molly is a 21 year old unemployed women. She has currently dropped out of University where she was studying Biology, stating that “life is just too hard right now” and that she just can’t make things work. Molly has been treated previously for Anorexia Nervosa and non-suicidal self-injuring behaviors with little success. She has always been a worrier and stressed over small things. Her mood fluctuates often and she has difficulty controlling her anger. Case Study Cont’d Molly’s roommate has been very supportive of her, but the recent increase of starving, purging, cutting, and burning behaviors have had a very negative effect on her. As a result, she has asked Molly to move out. Molly has recently broken up with her boyfriend, so she can’t live with him. She described their relationship as “intense”. Her only other option is to move back home with her parents who Molly describes as cold and controlling. Molly presents herself as a pleasant, friendly women who is happy to chat about mundane things, but becomes guarded to speaking about her health and relationships. Options of Coping 1) Counseling Cognitive Behavioral Therapy (CBT), Dialectical Behavioral Therapy (DBT), Schema-focused Therapy 2) Remain neutral Don’t get sucked in! Remember, people with Borderline Personality Disorder tend to have major difficulties with relationships 3) Medication No medications have been approved by the U.S. Food and Drug Administration to treat BPD; but there are some to help with symptoms such as anxiety, depression, or aggression Dialectical Behavioral Therapy Modified form of Cognitive Behavioral Therapy; adapted to meet particular needs of people who experience emotions very intensely, such as people with Borderline Personality Originally created for treatment of BPD, but is now used in a variety of treatment settings DBT is a therapy designed to help people change patterns of behavior that are not helpful, such as self-harm, suicidal thinking, and substance abuse Uses group work (skills training), individual therapy, and self-monitoring to change target behaviors DBT The main focus is on increasing the persons emotional and cognitive regulation by learning about the triggers that lead to reactive states Also focuses on accepting who you are at the same time as acknowledging that they need to change in order to reach their goals Places particular importance on the relationship between the person and their therapist; this relationship is used to actively motivate the person to change DBT Cont’d Skills taught in DBT: Mindfulness, distress tolerance, interpersonal effectiveness, emotion regulation Medication • Antidepressants • Atypical Antipsychotics Comorbidity • Someone with a PD is likely to have a co-occurring major mental disorder, including: Anxiety disorders Mood disorders Impulse control disorders Substance abuse or dependence Conclusion A personality disorder is a type of mental illness in which you have trouble perceiving and relating to situation and to people – including yourself Therapy is the best form of treatment for personality disorders; use medication only as a last resort Families play a crucial role in supporting their affected family member’s recovery, but families also need support and nurturing to recover from the impact of their family member’s illness