is Psychosis in Borderline Personality Disorder any
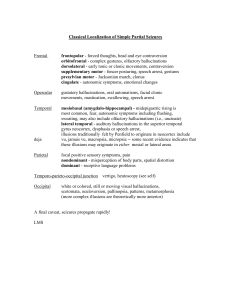
advertisement

Meanwhile, back at the Borderline…… Psychosis and Borderline Personality Disorder Chris Holman October 2012 ISPS conference • • • • Introduction What do people with BPD say? What do I think BPD is? What is the range of psychotic experiences people describe? • What is going on to cause the experiences? • Does this tell us anything interesting about psychotic experiences? …something about words… schizophrenia = “schizophrenia” borderline PD = “borderline PD” psychosis = psychosis Psychosis ?= Dissociation DSM 4 • ‘Transient, stress-related paranoid ideation or severe dissociative symptoms’ • Pseudohallucinations • Berrios and Dening (1996), Pseudohallucinations: a conceptual; history. Psychological Medicine, 26, 753 – 64 Rachel’s story • Auditory hallucinations • Visual hallucinations, associated with hallucinatory experiences in other modalities • Paranoia • Other psychotic experiences • Triggers and things that help • Why does she not tell people? • Difference from flashbacks Borderline Personality Disorder • Stern A., (1938) Psychoanalytic investigation and therapy in borderline group of neuroses. Psychoanalytic Quarterly 7, 467-8 BPD 5 of: • Efforts to avoid abandonment • Unstable/intense relationships • Unstable identity • Damaging impulsivity • Recurrent suicide/self-harm • Affective instability • Chronic emptiness • Inappropriate anger • Paranoia/dissociation BPD • Central Place of Affect Regulation – Affective Instability – Inappropriate anger – Suicide/self-harm • Interpersonal Difficulties – Unstable/intense relationships – Efforts to avoid abandonment – Chronic emptiness • Impaired Sense of Self – Unstable identity – Impulsivity BPD • Paranoia and Dissociation ? What is BPD? Fonagy, P, Gyorgy, G, Jurist, E, Target, M, (2004) Affect Regulation, Mentalisation and the Development of the Self Pub: Karnac • Social Bio-feedback theory of affect mirroring • Primary Carer (Maternal) Attachment Style and Infant Development Antonio Damasio (2000) The Feeling of What Happens Pub: Vintage • Construction of the Sense of Self ….a few recent studies…. ‘Persistent hallucinosis in borderline personality disorder’, Yee et al (2005) Comprehensive Psychiatry 46, 147 – 154 • Survey of a series of 171 people: ‘auditory hallucinations occur in 30%’ • 10 people who reported hallucinations described in detail • Hallucinations are persistent and an important part of their experience • Associated with Abuse ‘Persistent hallucinosis in borderline personality disorder’, Yee et al (2005) Comprehensive Psychiatry 46, 147 – 154 Types of hallucination • • • • Normative Traumatic-intrusive Psychotic Organic Hallucinosis Borderline Personlaity Disorder and Psychosis: a Review Barnow et al. (2010) Current Psychiatric Reports 12, 186 - 195 • Vague distinctions between hallucinations, paranoia and dissociation • No theoretical formulation • Agree psychotic phenomena are related to trauma history Olanzapine for the treatment of borderline personality disorder: variable dose 12-week randomised double-blind placebo-controlled study Charles Schulz et al. (2008) BJPsych 193, 485 492 • 52 centre study of 385 participants, Olanzapine vs Placebo • Main measure Zanarini rating scale (include others, but no measure of Psychosis) • Both Olanzapine and Placebo showed significant improvement at 12 weeks …things we might conclude… • Hallucinations in all modalities are common in people with BPD • They are persistent, troubling, and often experienced as directing the person to self-harm or other behaviours • They are trauma-related • Paranoia is a common state of mind • Other psychotic experinces occur but are not so common • They are not the same as flashbacks • They are not the same as dissociation …so what’s going on...? Dissociation • Direct trauma response: ‘coping strategy’ • over-regulation in response to overwhelming terror • Emotional Personality EP (as against Apparently Normal Personality ANP) (Nijenhuis et al. (2010) Trauma-related structural dissociation of the personality Activitas Nervosa Superior 52, 1 – 23) • Related to flashbacks and over-arousal (PTSD) …so what’s going on...? Hallucinations • Disturbance of Perception • More likely when disturbed or isolated • Involve distress-related experinces Affect and perception • Capgras syndrome: absence of affective ‘label’ robs face of significance • Misperceptions by bereaved people • Misidentify self in the mirror Affective labelling trumps sensory evaluation Affect and perception See it with feeling: affective predictions during object perception. L F Barrett and Moshe Bar (2009) Phil Trans Roy Soc B 364, 1325 – 1334 • The mind/brain is constantly producing hypotheses about external perceptions and internal experiences (‘resting brain’) • The Proactive Brain: using analogies and associations to generate predictions (M Bar (2007) Trends in Cognitive Sciences 11, 280) • Affective response to provisional perception occurs early Affective experience is at least equal with cognitive in generating hypotheses Hallucinations and Perceptual Set A set of affective and cognitive conditions which regulate perception Implies: • improved affect regulation will reduce vulnerability • Grounding and mindfulness are useful interventions • ‘Violating the Perceptual Set’ will resolve the hallucination Conclusions • Psychotic experiences are common and sustained in many people with BPD • Hallucinations in BPD are trauma-related • They can be understood if one places affect at the heart of the experience of external reality • (Say something about Paranoia) • These are not the same as Dissociative experiences Discussion • Does this tell us anything we did not know already? • Is this different from the process causing Hallucinations in ‘Schizophrenia’?