Treating the Difficult Patient
advertisement

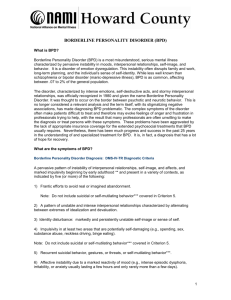
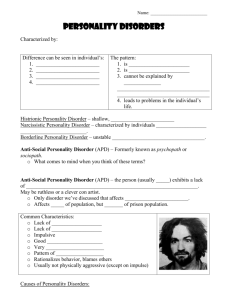
Borderline Personality Disorder Curley Bonds, MD Presentation by Amber Kondor, MD Telemental Health and Psychiatric Consultation Los Angeles County DMH Special Thanks – Ricardo Mendoza, MD Chief Mental Health PsychiatristTelemental Health and Psychiatric ConsultationLos Angeles Co. Dept. of Mental Health Understand the Prevalence and Relevance of Borderline Personality Disorder in Primary Care Be better able to identify, diagnose, and understand a patient with BPD Define Countertransference and understand its relevance Learn strategies to effectively communicate and care for patients with BPD • Prevalence ~2-6% of gen pop, ~10% of outpatient psych patients; 30-60% of personality disorders (Common in primary care!) • Women:men = 4:1 • The apple doesn’t fall far from the tree – 5x more common in family members of probands • A large proportion have a history of sexual abuse, unstable and traumatic childhood, early sexual activity, drug use, and pregnancies • More than half of adults with BPD self-mutilate Up to 10% of adults with BPD commit suicide – 400X more likely than the general population – but this is largely a “parasuicidal” population BPD is associated with considerable mental and physical disability 90% have 1 or more psych diagnoses Major Depression – 60% of patients with BPD Anxiety Disorders – 30% have panic disorder with agorophobia Alcohol and other Substance Use Disorders – 12% Bipolar Disorder – 10% PTSD Dissociative Identity Disorder (AKA Multiple Personality Disorder) Eating Disorders (especially Bulimia) – vomiting as presentation in primary care ADHD Antisocial Personality Disorder Other Personality Disorders (Cluster B traits) Borderline between neurosis and psychosis – a historic way of looking at the disorder • Unstable mood, affect, behavior, relationships, and self-image • Marked by impulsivity, suicidal acts, self-mutilation, identity problems, and feelings of emptiness or boredom • ICD-10 uses the name “emotionally unstable personality disorder” A pervasive pattern of instability of interpersonal relationships, self-image, and affects, and marked impulsivity beginning by early adulthood and present in a variety of contexts. Five (or more) criteria must be met for diagnosis of BPD. (1) Frantic efforts to avoid real or imagined abandonment (not including self-mutilating behavior) “I’ve damaged so many relationships through the need for control and the fear of being left, and for a long time I thought that fear was justified” – anonymous blogger Patients with BPD will often stay in physically and emotionally abusive relationships, just so they won’t be alone. (2) A pattern of unstable and intense interpersonal relationships characterized by alternating between extremes of idealization and devaluation (3) Identity disturbance: markedly and persistently unstable self-image or sense of self Uncertainty of self-image, sexual orientation, career choice or other long term goals, friendships, values “Sometimes I feel as though I’m two different people, ripping at each other” – anonymous blogger with BPD (4) Impulsivity in at least 2 areas that are potentially self-damaging (spending, sex, drugs, recklessness, binge eating) (5) Recurrent suicidal behavior, gestures, or threats, or self –mutilating behavior (6) Affective Instability due to a marked reactivity of mood (intense episodic dysphoria, irritability, or anxiety – for hours to days at a time) (7) Chronic feelings of emptiness “Constantly being terrified of abandonment and confused over everything you are isn’t a walk in the park; it’s a depressing, stressful, soul-destroying way to exist.” – anonymous blogger with BPD (8) Inappropriate, intense anger or difficulty controlling anger WHAT DO YOU MEAN I CAN’T HAVE MORE XANAX??? (9) Transient, stress-related paranoid ideation or severe dissociative symptoms Low K EKG changes in a young person; arrhythmias Enlarged Parotids, dental changes, gum irritation Self mutilation – cuts, burns, etc Childhood trauma, esp. sexual abuse Early history of drug use, pregnancies, high risk behaviors Multiple somatic complaints, multiple former PCPs Difficult doctor-patient relationship What are you likely to encounter in your office? Splitting your office staff, previous doctors – examples to follow Splitting – the inability to feel two opposing emotions simultaneously, or to integrate the good with the bad Requests for urgent appointments after hours, multiple phone calls, often desperate. Extending appointment times, repeated crisis or emergency appearances at the office Sudden hostility at not meeting their immediate demands (prescribing benzos, etc) STRUCTURE Set boundaries together, and stick to them Actively structure encounters Brief frequent visits, with verbal plan for future visits Be “Radically Genuine” Honest and straightforward LaForge, E. (2007) Stay calm and empathic to diffuse hostility Emotional Outbursts: recognize feelings but request appropriate behavior “I see that you’re angry, and we can continue talking about this if you will lower your voice.” (note the recognition of the emotion, and clear request for appropriate behavior) If the patient doesn’t respond – leave the room, indicating that when their behavior is appropriate, the conversation can resume. LaForge, 2007 Beware of splitting: don’t devalue or over defend “the woman you have working at the front desk is completely useless. If you weren’t so good at treating your patients, no one would come to this clinic.” “I’m so lucky I found you – I think my last doctor was trying to kill me with his incompetence. Reacting may reinforce the behavior Splitting is often an unconscious process in BPD patients – remain as neutral as possible, and talk about your feelings with a colleague LaForge, 2007 Watch for Countertransference What is countertransference? The emotions that the patient encounter/relationship stirs up in you Positive countertransference: Clinician unconsciously responds to idealization to stay in the patient’s favor Negative Countertransference: Unconsciously responding to devaluing by ignoring, avoiding or devaluing the patient’s complaints, even feeling tempted to punish the patient LaForge, 2007 Strive for conservative medical management – but provide an appropriate thorough, routine medical evaluation Overuse of diagnostic resources promotes a “sick” role for the patient Patients with BPD do appear to display a high degree of somatization Address their concerns, but also teach about stress and its effects on health – it’s generally a bad idea to tell them, “It’s all in your head.” LaForge, 2007 Open honest discussion of the role of emotions/life stressors in medical concerns – and even aspects of BPD, if appropriate They might begin to understand the connection Your stable doctor-patient relationship may be their first stable relationship! Your influence may help them get the appropriate mental health treatment The patient needs to know that you are not abandoning them – you are still their PCP, but they will be forming an additional relationship LaForge, 2007 Bring a chaperone for physical exams – patients with BPD misinterpret reality and have poor boundaries. They may mistake elements of a physical exam as indicative of a personal relationship. Patients with BPD constitute a majority of patients who falsely accuse their therapists of sexual involvement – it’s wise to have a third party as a buffer. LaForge, 2007 Suicide and self-harm will be issues The patient will likely acknowledge this Take the behaviors seriously REFER for psychiatric treatment, involuntary hospitalization if necessary: It is appropriate to refer when patients engage in repeated self-injurious or life-endangering behaviors, or when their needs for reassurance or safety monitoring involve many interappointment contacts 1. A 44-Year-Old Woman With Borderline Personality Disorder; JAMA, February 27, 2002—Vol 287, No. 8 1035 2. LaForge, E. (2007). The Patient with Borderline Personality Disorder. Journal of the American Academy of Physician Assistants. 20,46-50. Low-Serotonin Trait Vulnerability in BPD- Manifests as significant impulsivity SSRIs Benzos for co-occurring anxiety? Use sparingly and monitor usage Affective instability may be treated with mood stabilizers Meds are effective at target symptoms, but not curative Treat co-morbid Axis I disorders – takes higher doses and longer to take effect Dialectical Behavior Therapy – developed by Marsha Linehan – is the mainstay Requires a significant commitment from the patient Prognosis is not bad- over many years of therapy, the majority will improve. The PCP is likely to have the essential role in initiating psychotherapy treatment (adjunct, not replacement for primary care) In treating BPD patients in the medical setting, set clear boundaries, be honest and clear in communications, validate their feelings and reassure, but don’t get too close! Monitor your own countertransference (and talk with colleagues to help with this). Long term attachment and stable support systems are the essence of what is needed in people with BPD. Once you build rapport, talk to your patient about DBT – they can get better! American Psychiatric Association (1994), Diagnostic and Statistical Manual of Mental Disorders, 4th Edition. Washington: American Psychiatric Association. Davison, SE. (2002). Principles of managing patients with Personality Disorder. Advances in Psychiatric Treatment. 2002, 8:1-9. Gross, R, et al. Borderline Personality Disorder in Primary Care. Archives of Internal Medicine, 2002; 162(1):53-60. LaForge, E. (2007). The Patient with Borderline Personality Disorder. Journal of the American Academy of Physician Assistants. 20,46-50. Ward, R.,(2004). Assessment and Management of Personality Disorders. American Family Physician. 2004 Oct 15;70(8):1505-1512. Literature to consider: Sansone, R. and Sansone, L. Borderline Personality Disorder in the Medical Setting: Unmasking and Managing the Difficult Patient.