(MBT) skills training on clinical practice
advertisement

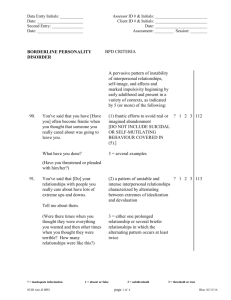
DSM-5 diagnostic criteria for borderline personality disorder (APA, 2013) A pervasive pattern of instability of interpersonal relationships, self-image and affects, and marked impulsivity beginning by early adulthood and present in a variety of contexts, as indicated by five (or more) of the following: 1 – Frantic efforts to avoid real or imagined abandonment. Note: Do not include suicidal or self-mutilating behaviour covered in Criterion 5 2 – A pattern of unstable and intense interpersonal relationships characterized by alternating between extremes of idealization and devaluation 3 – Identity disturbance: marked and persistently unstable self-image or sense of self 4 – Impulsivity in at least two areas that are potentially self-damaging (e.g., spending, sex, substance abuse, reckless driving, binge eating). Note: Do not include suicidal or self-mutilating behaviour covered in Criterion 5 5 – Recurrent suicidal behaviour, gestures or threats or self-mutilating behaviour 6 – Affective instability due to a marked reactivity of mood (e.g., intense episodic dysphoria, irritability or anxiety usually lasting a few hours and only rarely more than a few days) 7 – Chronic feelings of emptiness 8 – Inappropriate intense anger or difficulty controlling anger, (e.g., frequent displays of temper, constant anger, recurrent physical fights) 9 – Transient, stress related paranoid ideation or severe dissociative symptoms. Note: DSM-5 diagnoses as ‘borderline personality disorder‘ ICD-10 diagnoses as ‘emotionally unstable personality disorder‘. MBT developed using DSM criteria. 4 Wards within a Unit 28 Beds per Ward Mixed Sex Patients aged 18 – 65 Also 14 – 18 year olds in one ward Staff on Shift Patterns An accident and emergency for mental health A melting pot of diagnoses and disorders Evidence-based and developed Specifically for BPD Mentalizing is how we implicitly and explicitly interpret the actions of oneself and others Empathy as a foundation The Not Knowing Stance Provide Alternative Perspectives Restrained Imagination - Aims to encourage patients and staff to see themselves from the outside, others from the inside Common sense view of the mind Cost-effective BPD accounts for estimated 20% of psychiatric inpatients Associations with frequent and lengthy admissions BPD carries a diagnostic baggage and a negative staff perception No studies on staff perceptions of MBT MBT studies limited to specialised settings MBT Skills Training is a new and compact two day workshop Ethical and R&D approval Purposive sampling of staff nurses, across 4 acute mental health wards, who had completed MBT Skills Training 50% participation – 9 from 18 2 x Focus Groups with a neutral facilitator Semi-structured topic guide Thematic analysis – 3 cycles of coding Staff Perceptions on BPD Inpatient Care Impact on Staff Impact of MBT Skills Training Clinical Supervision Changed Perceptions of BPD Inpatient Environment BPD Behaviour on a Ward BPD Effect on the Ward Admission Pattern Ability to Work Effectively with BPD Personal Distress Uncomfortable Emotions Negative Perceptions Empathy Use of MBT Changes in Staff Benefits of MBT MBT Limits Attendance Benefits of Group CS One to One Clinical Supervision Informal Clinical supervision Yes! An understanding of reasons behind behaviour Awareness of the impact of feelings of abandonment More empathy towards people with BPD BPD is extremely challenging for staff nurses in acute mental health Staff experience significant personal distress MBT gives staff a ‘secret weapon’ Clinical Supervision provides support, reassurance and ‘ammunition’ Staff had a better understanding of BPD and more empathy as a result All staff nurses attend MBT Skills Training MBT is offered as part of the pre-registration nursing programme Group Clinical Supervision is offered weekly and within protected time Further research into MBT skills training and inpatient care of BPD Any Questions? daniel.warrender@nhs.net