Slides for Chapter 5
advertisement

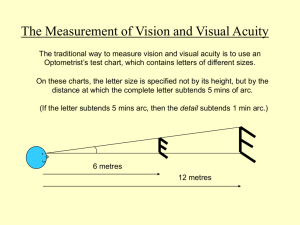
CHAPTER 5. SPATIAL ACUITY Harold Bedell, College of Optometry, University of Houston Why cover “acuity” in a course called “Central Visual Mechanisms”? …because we are now talking about how the whole visual system works and how we can measure vision. Acuity has a neural basis, but it is typically measured in a “whole organism” (person or animal), though it is also possible to measure the acuity of single neurons. Comparison of Spatial Acuity Tasks and Thresholds Acuity Task Typical Stimulus Minimum Threshold Detection Single black spot 15” – 20” Single black line 0.5” – 1.0” Spatial interval 2” – 4” Vernier lines 3” – 6” Two black lines/spots 30” – 40” Grating 30” – 40” Letters or numerals 30” – 40” Localization Debate: are resolution and identification acuity the same? Resolution Identification Detection acuity is the angular size of the smallest visible target It is an intensity discrimination task You need to be able to explain the reason that detection acuity is an intensity discrimination All types of visual acuity are determined largely by optical and “neural” defocus For all types of acuity, need to consider these three things: The retinal image Photoreceptor sampling Convergence (receptive field center size) = “neural defocus” How images spread out on the retina & interaction with pupil size 1.5 mm Relative Retinal Illuminance 2.4 mm 6.6 mm -4 -2 0 2 Angular Distance (min) 4 Dashed line = theoretical point-spread function based on pupil alone (larger pupil give narrowest point-spread) Solid line = actual pointspread function based on all factors (intermediate pupil is best) For wide objects the eye’s optics only affect the edges of the shadow’s image on the retina light At cornea dark On retina As the object gets thinner, the shadow gets thinner. BUT, when the object is smaller than 3 arc seconds (3”) the width of the shadow stays the same Target The line against the sky Target Luminance 1.0 Shadow on cornea 0.8 0.6 0.4 0.2 0.0 Retinal Illuminance 1.0 Shadows on retina 0.8 0.6 3 SEC ARC 0.4 0.2 0.0 Photoreceptor Array -1 0 Retinal Position (min) +1 Target The line against the sky Target Luminance 1.0 Shadow on cornea 0.8 0.6 0.4 0.2 0.0 Retinal Illuminance 1 SEC ARC 1.0 Shadows on retina 0.8 0.6 0.4 0.2 0.0 Photoreceptor Array -1 0 Retinal Position (min) +1 Photoreceptor mosaic at the fovea (2 people) Shadow at cornea Spread out image on retina Target Target Luminance 1.0 Shadow on cornea 0.8 0.6 0.4 0.2 0.0 Retinal Illuminance 1 SEC ARC 1.0 Shadows on retina 0.8 0.6 3 SEC ARC 0.4 0.2 0.0 Photoreceptor Array -1 0 Retinal Position (min) +1 To detect the line, the hyperpolarization of the cone at 0 must be different enough from that of adjacent cones so that the ganglion cell activity sends a strong enough signal to cortex to be detected. In the fovea, each cone connects, through the bipolar cell, to a ganglion cell. One cone = RF center. This forms a direct line to LGN and cortex. Target Target Luminance 1.0 Shadow on cornea 0.8 0.6 0.4 0.2 0.0 Retinal Illuminance 1 SEC ARC 1.0 Shadows on retina 0.8 0.6 3 SEC ARC 0.4 0.2 0.0 Photoreceptor Array -1 0 Retinal Position (min) +1 To detect the line, the hyperpolarization of the cone at 0 must be different enough from that of adjacent cones so that the ganglion cell activity sends a strong enough signal to cortex to be detected. Actually, a series of cones in the center of the shadow would be less hyperpolarized than the ones on either side. These cones would signal, through a bipolar cell and a ganglion cell, the presence of a line. Detection acuity is the angular size of the smallest visible target It is an intensity discrimination task When the shadow is so pale that the row of cones under the shadow is not hyperpolarized enough, relative to the rows of cones on each side, to cause less firing in on-center ganglion cells and more firing in off-center ganglion cells than is produce in the ganglion cells fed by adjacent rows of cones. Visual acuity is determined largely by optical and "neural" defocus The retinal image Photoreceptor sampling Convergence (receptive field center size) = “neural defocus” A line needs to be thicker in the periphery to be detected because of convergence; several photoreceptors connect to a bipolar cell and several bipolar cells connect to a ganglion cell. Outside the fovea, convergence increases Localization acuity (also called “hyperacuity”) is the smallest spatial offset or difference in location between targets that can be discriminated Comparison of Spatial Acuity Tasks and Thresholds Acuity Task Typical Stimulus Minimum Threshold Detection Single black spot Single black line 15” – 20” 0.5” – 1.0” Localization Spatial interval Vernier lines 2” – 4” 3” – 6” Resolution Two black lines/spots Grating 30” – 40” 30” – 40” Identification Letters or numerals 30” – 40” Vernier lines Spatial Interval s Offset s Ds Various forms of localization tasks March 2007 Vision Research Vernier Acuity in the Barn Owl Visual acuity is determined largely by optical and "neural" defocus The retinal image Photoreceptor sampling Convergence (receptive field center size) = “neural defocus” The threshold for detecting the mis-alignment of lines is less than the width of a cone, so the retina cannot detect this itself. Rather, this discrimination is achieved at the cortical level (somewhere). Localization (hyperacuity) tasks seem to involve neural mechanisms beyond the retina (presumably in visual cortex) Resolution acuity Also called “minimum separable acuity” Resolution acuity is the smallest spatial separation between two nearby points or lines that can be discriminated The Minimum Angle of Resolution (MAR) This is what is generally called “visual acuity” and is the most common measure of visual function made by eye-care practitioners Uses of Spatial Acuity Measures •Assess if refractive error is present •Decide when to change glasses Rx •Assess visual function (best corrected refractive error) •Assess job eligibility (pilots, police, etc.) •Follow disease and treatment •Decide whether a person should drive •Decide whether a person qualifies for disability •Low vision assessment •Prediction of improvement with vision aids Table 5-1: Comparison of Spatial Acuity Tasks & Thresholds Acuity Task Typical Stimulus Minimum Threshold Detection Single black spot Single black line 15 - 20 sec of arc 0.5 - 1.0 sec of arc Localization Spatial interval Vernier lines 2 - 4 sec of arc 3 - 6 sec Resolution Two black lines/spots Grating 30 - 40 sec of arc 30 - 40 sec of arc Identification Letters or numerals 30 - 40 sec of arc Chapter 1: most of the measures of vision people make are threshold measures. All acuity measures (all three types) are threshold measures Detection acuity: we measure the threshold line width (or spot size) Localization acuity: we measure the threshold offset Resolution acuity: we measure the threshold separation Visual acuity is determined largely by optical and "neural" defocus The retinal image Photoreceptor sampling Convergence (receptive field center size) = “neural defocus” Target More realistic depiction of the Target point-spread Luminance 1.0 function (line0.8 spread function 0.6 here, viewed in 0.4 0.2 cross-section) 0.0 Retinal Illuminance 1.0 0.8 0.6 0.4 0.2 0.0 Photoreceptor Array -1 0 Retinal Position (min) +1 The closer together the points or lines, the less of a “dip” in intensity in between the retinal images Photoreceptor sampling At the fovea, there is a match between photoreceptor size and spacing, and MAR Center-to-center spacing of 20” – 40” in the fovea Resolution 30” – 40” (0.5’) – one row of cones in between What happens when the retinal image is defocused? Why is it that the MAR gets larger (poorer acuity) when images are out of focus? (slides from Dr. Fullard) Use Blur Ratio pupil diameter (in meters) ametropia yA Blur Ratio tan tan (visual angle of VA chart letter) The closer together the points or lines, the less of a “dip” in intensity in between the retinal images The closer together the points or lines, the less of a “dip” in intensity in between the retinal images Convergence (receptive field center size) = “neural defocus” The larger the receptive field, the poorer the resolution acuity (lines must be spaced farther apart) A B Outside of Fovea At Fovea 1 2 1 3 B-1 B-2 B-3 B B B G-1 G-2 G-3 G G G LGN-1 LGN-2 LGN-3 LGN LGN LGN V1-1 V1-2 V1-3 V1 The result of larger receptive fields is that the stimuli need to be farther apart for the central “dip” in intensity to be detected at the cortex A B Outside of Fovea At Fovea 1 2 1 3 B-1 B-2 B-3 B B B G-1 G-2 G-3 G G G LGN-1 LGN-2 LGN-3 LGN LGN LGN V1-1 V1-2 V1-3 V1 Resolution acuity is the smallest spatial separation between two nearby points or lines that can be discriminated The Minimum Angle of Resolution (MAR) This is what is generally called “visual acuity” and is the most common measure of visual function Target Target Luminance 1.0 0.8 0.6 0.4 0.2 0.0 Retinal Illuminance 1.0 0.8 0.6 0.4 0.2 0.0 Photoreceptor Array -1 0 Retinal Position (min) +1 How do you measure resolution acuity? Resolution acuity can be measured using multiple lines (gratings) If there are 60 lines per degree, each line is 1’ and each pair (cycle) is 2’ (30 c/deg) 1 light-dark cycle = 1.50 min arc 1 line = 0.75 min arc 1 degree 40 light-dark pairs = 40 cycles per degree “Standard normal” VA (resolution visual acuity; MAR) is 1 min of arc (1’ arc) On a log scale, log(1) = 0, so standard normal VA is 0 on a logMAR chart; 10’ arc = 1 on chart “better” acuity means able to resolve smaller angles “worse” or “poorer” acuity means larger angles are needed Grating acuity measures are relatively insensitive to optical defocus An example of “How you measure vision determines the result” Worse (poor acuity) LogMAR 1.8 Gratings Letters 1.6 1.4 1.2 1.0 0.8 0.6 0.4 0.2 Better (good acuity) 0.0 0 2 4 6 Blur (diopters) 8 10 12