File
advertisement

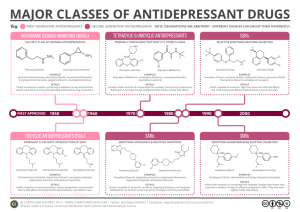
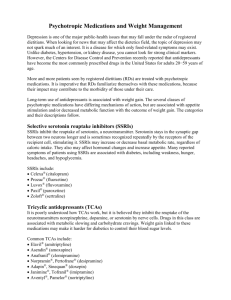
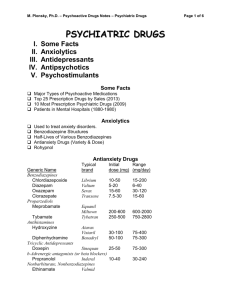
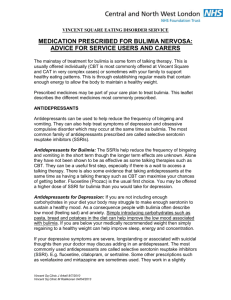
Antidepressant and mood stabilizing agent Safa Mansour Othman Tips to be Covered Antidepressants Definition. what conditions are antidepressants used?? Are there differences among antidepressants? What are side effects of antidepressants? Mood stabilizer agent. Questions. Definition Antidepressants: are a class of drugs that reduce symptoms of depressive disorders by correcting chemical imbalances of neurotransmitters in the brain. Chemical imbalances may be responsible for changes in mood and behavior. Definition Neurotransmitters are vital, as they are the communication link between nerve cells in the brain. Neurotransmitters reside within vesicles found in nerve cells, which are released by one nerve and taken up by other nerves. Neurotransmitters not taken up by other nerves are taken up by the same nerves that released them. This process is called "reuptake." The prevalent neurotransmitters in the brain specific to depression are serotonin, dopamine and norepinephrine (also called noradrenaline). Definition n general, antidepressants work by inhibiting the reuptake of specific neurotransmitters, hence increasing their levels around the nerves within the brain, such as selective serotonin reuptake inhibitors (SSRIs), antidepressants that will affect serotonin levels in the brain. conditions are antidepressants used Antidepressants are used to treat several conditions. They include, but are not limited to: depression, generalized anxiety disorder, agitation, obsessive compulsive disorders (OCD), manic-depressive disorders, childhood enuresis (bedwetting), major depressive disorder, diabetic peripheral neuropathic pain, neuropathic pain, social anxiety disorder, posttraumatic stress disorder (PTSD) etc. conditions are antidepressants used Some off- label uses of antidepressants include, but are not limited to:fibromyalgia, chronic urticaria (hives), hot flashes, hyperhidrosis (druginduced), pruritus (itching), premenstrual symptoms, bulimia nervosa,Tourette syndrome, binge eating disorder, etc. Are there differences among antidepressants? Antidepressants differ in their effects on neurotransmitters, established uses, adverse effects and drug interactions. All antidepressants that are used for depression are effective; there is no evidence that one antidepressant is more effective than another. However, patients may respond to or tolerate one antidepressant, and not respond to or tolerate another antidepressant. What are side effects of antidepressants? Antidepressants that belong to the same class of antidepressant produce similar side effects. Antidepressants may cause withdrawal symptoms if abruptly discontinued. Withdrawal symptoms include nausea, vomiting, dizziness, headache, irritability, sleep disturbance, nightmares, psychosis, and seizures. What are side effects of antidepressants? All antidepressants have a warning about use in children and adolescents. Antidepressants increased the risk of suicidal thinking, and suicidal behavior in short-term studies in children and adolescents with depression and other psychiatric disorders. Anyone considering the use of antidepressant in a child or adolescent must balance this risk of suicide with the clinical need for the drug. Patients who are started on therapy should be closely observed for clinical worsening, suicidal thoughts or unusual changes in behavior. Tricyclic antidepressants (TCAs) side effects Tricyclic antidepressants (TCAs) are a class of antidepressant associated with sedation, dry mouth, blurred vision, constipation, urinary retention, and increased pressure in the eye. Tricyclic antidepressants (TCAs) side effects They are also associated with hypertension, abnormal heart rhythms, anxiety, insomnia, seizures, headache, rash, nausea, and vomiting, abdominal cramps, weight loss, and sexual dysfunction. Tricyclic antidepressants rarely cause liver failure. Selective serotonin reuptake inhibitors (SSRIs) side effects Selective serotonin reuptake inhibitors (SSRIs) and serotonin/norepinephrine reuptake inhibitors (SNRIs) are two classes of antidepressants associated with : abnormal thinking, agitation, anxiety, dizziness, headache, insomnia, sexual dysfunction, sedation, tremor, sweating, weight loss, diarrhea, constipation, dry mouth, rash, and nausea. Rarely, SSRIs have been associated with hyponatremia (low sodium),hypoglycemia (low blood glucose), and seizures. Monoamine oxidize inhibitors (MAOIs) side effects Monoamine oxidize inhibitors (MAOIs) are a class of antidepressant associated with postural hypotension (feeling faint upon standing due to decreased blood flow to the brain Monoamine oxidize inhibitors (MAOIs) side effects high blood pressure, fainting, abnormal heart rhythm, dizziness, headache, drowsiness, insomnia, anxiety, constipation, nausea, diarrhea, sexual dysfunction, weight gain or weight loss, and edema. Seizures, rash, blurred vision, and hepatitis are infrequently associated with MAOIs. What are the possible drug interactions? Tricyclic antidepressants (TCAs) • Combining tricyclic antidepressants (TCAs) with clonidine (Catapres) may lead to dangerous elevations in blood pressure because TCA may inhibit the antihypertensive effect of clonidine. What are the possible drug interactions? Tricyclic antidepressants (TCAs) • Combining TCAs with carbamazepine (Tegretol) may result in lower TCA blood levels and higher carbamazepine levels, leading to decreased TCA efficacy or increased carbamazepine toxicity. What are the possible drug interactions? Tricyclic antidepressants (TCAs) TCAs may increase the effects of epinephrine, norepinephrine and dopamine. Dangerous increases in blood pressure and abnormal heartbeats may occur. Cimetidine (Tagamet) may reduce the breakdown of some TCAs [for example, amitriptyline (Elavil)] and potentially lead to increased side effects. Selective serotonin reuptake inhibitors (SSRIs) interactions Selective serotonin reuptake inhibitors (SSRIs) should not be combined with other drugs that increase brain serotonin levels [for example, MAOIs, TCAs, sumatriptan (Imitrex), linezolid(Zyvox), St John's Wort, amphetamines] because there is a risk of dangerous adverse effects. The risk of gastrointestinal bleeding may be increased when SSRIs are combined with nonsteroidal antiinflammatory drugs (NSAIDs). Monoamine oxidize inhibitors (MAOIs) interactions Monoamine oxidize inhibitors (MAOIs) should not be combined with other antidepressants or other drugs that increase serotonin levels [for example, amphetamines, linezolid (Zyvox), St. Johns Wort, sumatriptan (Imitrex)]. Such combinations cause excessive serotonin levels in the brain, which may lead to confusion, high blood pressure, tremor, hyperactivity, coma, and death. Count's Administration of MAOIs and other antidepressants or drugs that elevate serotonin should be separated by 14 days. Administration of MAOIs with epinephrine, norepinephrine, phenylephrine, pseudoephedrine, and dopamine may lead to hypertensive crisis. MAOIs interact with tyramine containing foods, resulting in a hypertensive crisis. Examples of Antidepressants - Tricyclic antidepressants (TCA) amitriptyline (Elavil) amoxapine clomipramine (Anafranil) desipramine (Norpramin) doxepin (Sinequan) imipramine (Tofranil) nortriptyline (Pamelor) protriptyline (Vivactil) trimipramine (Surmontil) Selective Serotonin Reuptake Inhibitors citalopram (Celexa) escitalopram (Lexapro) fluoxetine (Prozac, Sarafem) fluvoxamine (Luvox) paroxetine (Paxil) sertraline (Zoloft) Monoamine Oxidize Inhibitors: phenelzine (Nardil) tranylcypromine (Parnate) isocarboxazid (Marplan) selegiline (EMSAM, Eldepryl) Other Antidepressants: maprotiline Mirtazapine (Remeron) trazodone Bupropion (Wellbutrin) nefazodone (Serzone) Diagnosis The following nursing diagnosis may be consider the clients receiving therapy with antidepressant medication : 1-risk for suicide rt depressed mood. 2-risk for injury rt side effect of medication, orthostatic hypotension , photosensitivity , arrhythmias , hypertensive crisis or serotonin syndrome . 3-social isolation rt depressed mood. 4-costipation rt side effect of the medication. Planning / implementation The plan of care should include monitoring the side effects from antidepressant medication . Nursing implications: Note (In the following slide ) Mood stabilizer: A mood stabilizer is a psychiatric medication used to treat mood disorders characterized by intense and sustained mood shifts, typically bipolar disorder. Uses: Used to treat bipolar disorder,[1] mood stabilizers suppress swings between mania and depression. Moodstabilizing drugs are also used in borderline personality disorder[2] and schizoaffective disorder. Lithium Carbonate WARNINGS: It is very important to have the right amount of lithium in your body. Too much lithium may lead to unwanted effects such as nausea, diarrhea, shaking of the hands, dizziness, twitching, seizures, slurred speech, confusion, or increase in the amount of urine. Tell your doctor immediately if these effects occur. Note The remaining things with safa The Nursing Process: MoodStabilizing Agents Background assessment data Indications: prevention and treatment of manic episodes associated with bipolar disorder Examples: lithium carbonate, clonazepam, carbamazepine, valproic acid, lamotrigine, gabapentin, topiramate, verapamil, olanzapine The Nursing Process: Mood-Stabilizing Agents (cont.) Background assessment data (cont.) Action: lithium enhances the reuptake of norepinephrine and serotonin in the brain, lowering levels in the body and resulting in decreased hyperactivity. Action of anticonvulsants, verapamil, and olanzapine in the treatment of bipolar disorder is not fully understood. Interactions Contraindications/precautions The Nursing Process: Mood-Stabilizing Agents (cont.) Nursing diagnosis Risk for injury Risk for self-directed or other-directed violence Risk for activity intolerance The Nursing Process: MoodStabilizing Agents (cont.) Planning/implementation Monitor for side effects of lithium Drowsiness, dizziness, headache Dry mouth; thirst; GI upset; nausea/vomiting Fine hand tremors Hypotension; arrhythmias, pulse irregularities Polyuria; dehydration Weight gain Potential for toxicity The Nursing Process: MoodStabilizing Agents (cont.) Lithium Toxicity Therapeutic range: 1.0–1.5 mEq/L Initial symptoms of toxicity include – Blurred vision, ataxia, tinnitus, persistent nausea and vomiting, and severe diarrhea Ensure that client consumes adequate sodium and fluid in diet The Nursing Process: Mood-Stabilizing Agents (cont.) Planning/implementation (cont.) Monitor for side effects of anticonvulsants Nausea and vomiting Drowsiness; dizziness Blood dyscrasias Prolonged bleeding time (with valproic acid) Risk of severe rash (with lamotrigine) Decreased efficacy with oral contraceptives (with topiramate) The Nursing Process: Mood-Stabilizing Agents (cont.) Planning/implementation (cont.) Monitor for side effects of verapamil Drowsiness; dizziness Hypotension; bradycardia Nausea Constipation The Nursing Process: MoodStabilizing Agents (cont.) Planning/implementation (cont.) Monitor for side effects of olanzapine Somnolence, dizziness, asthenia Fever; tachycardia Postural hypotension Dry mouth Constipation Increased appetite; weight gain The Nursing Process: Mood-Stabilizing Agents (cont.) Planning/implementation (cont.) – Educate client and family about the medication Outcome Criteria/Evaluation Questions: thank you