Antidepressants and Anxiolytics
advertisement

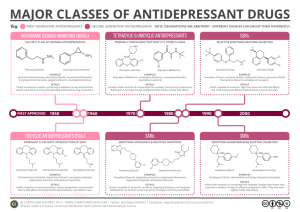
Antidepressants, Anxiolytics, and Sedative/Hypnotics Antidepressants • Tricyclic Antidepressants (TCAs) • Monoamine Oxidase Inhibitors (MAOIs) • Selective Serotonin Reuptake Inhibitors (SSRIs) • Serotonin Norepinephrine Reuptake Inhibitors (SNRIs) • Atypical antidepressants • Atypical antipsychotics Depression • Depressed mood, loss of pleasure or interest in usual activities • Sustained over time • Subtypes – Major depression – Clinical depression – Subclinical depression – Post-partum – Bereavement Depression • Every patient in the hospital needs to have depression addressed – Loss of functionality – Loss of youth/feeling of control – Chronic illness – Altered sleep and exercise patterns\ – Altered role Depression Treatment • • • • Cognitive therapy Behavioral therapy (exercise, art, etc.) ECT Pharmacology – Older protocol: treat major depression 6 – 12 months – Newer: long term or lifelong therapy – Distinguish: situational/transient depression TCAs • Old drugs, cheap • Multiple actions unsure – Inhibition of Norepinephrine & Serotonin reuptake • Multiple side effects • Not effective for depression except at high doses • May be toxic before becomes effective • Often used as adjunct for sleep and pain Adverse Effects • • • • • • • Orthostatic hypotension Anticholinergic effects Diaphoresis Sedation Cardiac toxicity Seizures Hypomania TCA Treatment • Must start low avoid toxicity – Takes several weeks to achieve effect – Starting high does not decrease time • Selecting a drug – Most are dosed once daily, usually HS – Choosing your side effects • More sedating drugs for patients with insomnia, etc. – Common agents: amitriptyline, nortriptyline, imipramine MAOIs • Older drugs • Relatively effective, but high toxicity – Especially drug and food interactions • Considered third line therapy • Hypertensive crisis – When using MAOIs, avoid • Avocadoes, cheese, wine, beer, soups, soy sauce, chocolate, caffeine, smoked foods • Yeah… no wonder they’re depressed • Linezolid (Zyvox): MAOI features SSRIs • Relatively new (1987) • Most prescribed class for depression • Blocks reuptake of serotonin only – Take 2 – 3 weeks for therapeutic effect • Uses: – Depression – Anxiety – Social phobia, obsessive-compulsive, PDD Adverse Effects • • • • • • Sexual dysfunction Weight gain Serotonin syndrome: 2 – 72 hours Withdrawal Syndrome Teen suicide? My experience with patients: – “feel flat,” “feel unresponsive” – Disturbing dreams Agents • • • • • • Fluoxetine (Prozac) Sertraline (Zoloft) Paroxetine (Paxil) Fluvoxamine (Luvox) Citalopram (Celexa) Escitalopram (Lexapro) (left hand of citalopram) Teaching Points • • • • Therapeutic delay Warning signs of Serotonin Syndrome Withdrawal syndrome Sexual side effects SNRIs • Venlafaxine (Effexor) – NE & serotonin reuptake inhibitor (weak dopamine); causes mild excitation • Duloxetine (Cymbalta) Atypical Antidepressants • Bupoprion (Wellbutrin) • Nefazadone (Serzone) – multiple effects • Mirtazapine (Remeron) – new class of drug; increased release of NE and serotonin Bupoprion (Wellbutrin) • Unclear action, but definitely blocks something with Dopamine • May increase sexual desire • May cause excitation • Dopamine associated with addictive behaviors – Bupoprion marketed for smoking cessation (Zyban) – Also may help concentration ADD Atypical Antipsychotics • Are not used for depression alone – Potentiate other antidepressant drugs – Used for depression with psychotic features • Common agents – Clozapine (Clozaril) – Risperidone (Risperdal) – Olanzapine (Zyprexa) – Quetiapine (Seroquel) Sedative-Hypnotics • • • • Benzodiazepines Benzo-like Barbiturates Miscellaneous Benzodiazepines • Safer and lower abuse potential that other CNS depressants (barbiturates) • Mechanism – Potentiate GABA (CNS neurotransmitter) – Bind to GABA-chloride gate receptors and enhance the natural action of GABA – Finite action • All are controlled substances Benzodiazepines • Effects – CNS • • • • Reduce anxiety Promote sleep Muscle relaxation Anterograde amnesia – CV: PO none; IV hypotension, cardiac arrest – Resp: weak depressants alone Kinetics • Most well absorbed PO • Metabolism – Most have active metabolites – Duration is wildly different among agents – Example • Flurazepam: 2-3 hour half-life; metabolite 50 hours Benzo Uses • • • • • • • Anxiety Insomnia Seizure Muscle Spasm Alcohol withdrawal (DT prevention) Panic Disorder Surgery – Induction of anesthesia – Conscious sedation Adverse Effects • CNS: drowsy, lightheaded, concentration, MVA • Amnesia • Paradoxical effects • Resp depression • Abuse • Don’t use in pregnant women Common Benzos • • • • • • • Diazepam (Valium) Lorazapam (Ativan) Alprazolam (Xanax) Clonazepam (Klonopin) Chlordiazepoxide (Librium) Temazepam (Restoril) Midazolam (Versed) – conscious sedation Benzo-like • Unrelated to Benzo chemical structure, but upregulate GABA in a similar manner • Schedule IV drugs – Zolpidem (Ambien) • Middle of the night confusion – Zaleplon (Sonata) • Better for falling asleep, not staying asleep Barbiturates • Bind to GABA-chloride receptor – Directly activate receptor – Enhance GABA’s natural action – No ceiling on effect • Highly addictive • Therapeutic uses for – Seizure – Anesthesia induction • Common: Phenobarbital Other Sedative-Hypnotics • Antidepressants – Amitriptyline (Elavil) – Trazadone • 1st generation antihistamine – Diphenhydramine (Benadryl, Nytol, Sominex) – Doxylamine (Unisom) – Hydroxyzine (Atarax) Anxiety • Benzos, SSRIs, others – Generalized Anxiety Disorder – Situational anxiety • SSRIs – Panic disorder – Obsessive-Compulsive D/O – Social anxiety – PTSD Other Anxiolytics • Buspirone (Buspar) – No sedation – No abuse potential – No interaction with ETOH – BUT, develops slowly: at least a week – Takes several to reach full potential – Used for short term therapy (up to a year) • Beta blockers – Primarily for performance/test anxiety Vitamin H: The Abused Antipsychotic • Haloperidol (Haldol) – Often prescribed by physicians for inpatient “agitation” – “ICU psychosis” – Haldol is not a sedative. Should not be used as either a sedative nor anxiolytic – If giving it more than twice a day • CALL THE PHYSICIAN AND GET ANOTHER DRUG ORDERED!!!!!!