BIOMED 370: The Treatment Of Mood Disorders
advertisement
BIOMED 370: The Treatment of
Mood Disorders
March 9, 2005
Lawrence H. Price, M.D.
Professor of Psychiatry and Human Behavior
Brown University School of Medicine
Clinical Director and Director of Research
Butler Hospital
345 Blackstone Blvd
Providence, RI 02906
DSM-IV MOOD DISORDERS
Depressive Disorders
Bipolar Disorders
Other Mood Disorders
Major Depression
Bipolar I D/O
Mood D/O due to
Gen Med Cond
Dysthymia
Bipolar II D/O
Substance-Induced
Mood D/O
Depressive D/O NOS
Cyclothymia
Mood D/O NOS
Bipolar D/O NOS
SPECIFIERS
FOR DSM-IV MOOD DISORDER EPISODES
Most recent episode
Severity/Psychosis/Remission
Course of recurrent episodes
Longitudinal Course
Mild
+Full Interepisode Recovery
Moderate
-Full Interepisode Recovery
Severe
-Psychosis
+Psychosis
Mood-Congruent
Mood-Incongruent
In Partial Remission
In Full Remission
Catatonic
Postpartum Onset
Chronic (Dep episodes only)
Melancholic (Dep episodes only)
Atypical (Dep episodes only)
Seasonal Pattern
Rapid Cycling
BASIC PRINCIPLES OF
ANTIDEPRESSANT USE
A.
B.
Achieve adequate dosing
•
•
Gradual titration upward.
Prepare patient for early side effects.
Treat for adequate duration
•
•
4-6 weeks for an acute trial.
6 months or longer for maintenance.
C.
Assess adequacy of response
D.
Ensure adherence
•
•
•
Avoid complex dosing schedules.
Make sure prescription is affordable.
Address side effects.
PHASES OF TREATMENT FOR DEPRESSION
Kupfer, J Clin Psychiatry,52(suppl 5):28, 1991..
ANTIDEPRESSANT TREATMENTS
I.
PRIMARY ANTIDEPRESSANTS
II.
MOOD STABILIZERS (Thymoleptics)
III. STIMULANTS
IV. ELECTROCONVULSIVE THERAPY (ECT)
V.
SURGICAL APPROACHES
VI. COMBINATION BIOMEDICAL APPROACHES
VII. NOVEL BIOMEDICAL APPROACHES
VIII. PSYCHOSOCIAL TREATMENTS
IX. OTHER SOMATIC TREATMENTS
BIOMEDICAL ANTIDEPRESSANT
TREATMENTS: MONOTHERAPIES
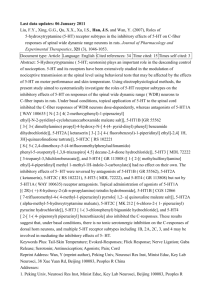
I. PRIMARY ANTIDEPRESSANTS
A. Selective serotonin reuptake inhibitors
(SSRIs)
B. Mixed monoamine reuptake inhibitors
C. Monoamine receptor antagonists
D. Tricyclic (TCAs) and related heterocyclics
E. Monoamine oxidase inhibitors (MAOIs)
F. NMDA antagonists
BIOMEDICAL ANTIDEPRESSANT
TREATMENTS: MONOTHERAPIES
A. Selective serotonin reuptake
inhibitors (SSRIs)
1.
2.
3.
4.
5.
Fluoxetine (Prozac®, Sarafem®)
Sertraline (Zoloft®)
Paroxetine (Paxil®)
Fluvoxamine (Luvox®)
a. Citalopram (Celexa®)
b. Escitalopram (Lexapro®)
Selective Serotonin Reuptake Inhibitors
(SSRIs): Mechanism of Action
5-HT
5-HT
5-HT Release
5-HT
5-HT
5-HT
5-HT
5-HT
5-HT
5-HT
5-HT
5-HT
5-HT
5-HT
5-HT
5-HT
5-HT
5-HT
5-HT
5-HT
5-HT
Downregulation of
presynaptic 5-HT1A
autoreceptors
5-HT
5-HT
Synaptic 5-HT
Reuptake transporter
Inhibition of 5-HT
reuptake transporter
5-HT = serotonin.
Blier and Abbott. J Psychiatry Neurosci. 2001;26:37.
Stimulation
of postsynaptic
5-HT receptors
5-HT
Selective Serotonin Reuptake Inhibitors
(SSRIs): Pros/Cons
Pros
Effective in 60%-70%
of patients
Cons
Nausea and headaches
Ease of dosing
Orgasmic dysfunction and
decreased libido
Broad comorbidity coverage
(eg, anxiety disorders)
Interactions with tryptophan,
MAOIs, fenfluramine
Lower side effect burden vs
TCAs
Discontinuation syndrome
Safer in overdose vs TCAs
Richelson. Mayo Clin Proc. 2001;76:511.
Weight gain
BIOMEDICAL ANTIDEPRESSANT
TREATMENTS: MONOTHERAPIES
B. Mixed monoamine reuptake inhibitors
1. NE/(DA) reuptake inhibitor
a. Bupropion (Wellbutrin®, Zyban®)
2. NE/5-HT reuptake inhibitors
a. Venlafaxine (Effexor®)
b. Duloxetine (Cymbalta®)
Bupropion (1985)
Mechanism
of Action
O
NH
Cl
Bupropion
Weak NA and DA
reuptake inhibitor
Metabolized to
less active
hydroxybupropion,
threohydrobupropion
and erythrohydrobupropion
Ascher et al. J Clin Psychiatry. 1995;56:395.
Croft et al. Clin Ther. 1999;21:643.
Coleman et al. Clin Ther. 2001;23:1040.
Pros
Efficacy similar
to SSRIs
Fewer sexual
side effects
Effective in
smoking
cessation
Possible
weight loss
Cons
Insomnia
Asthenia
Nausea
Increased
seizures at
higher doses
Potential for
drug-drug
interactions
Venlafaxine (1993)
Mechanism
of Action
N(CH3)2
OH
CH
H3CO
Venlafaxine
5-HT reuptake
inhibitor with NA
reuptake
inhibition
at higher doses
Metabolized to
equally active
O-desmethylvenlafaxine
Wellington and Perry. CNS Drugs. 2001;15:643.
Kent. Lancet. 2000;355:911.
Thase et al. Br J Psychiatry. 2001;178:234 .
Pros
Higher remission
rates?
Pharmacologically
“cleaner” than
TCAs
Cons
Nausea
Sweating
Orgasmic
dysfunction
Hypertension
Insomnia
Discontinuation
syndrome
Tremor
Dose titration
Tachycardia
Cost
Duloxetine (2004)
Mechanism
of Action
NH
S
O
Dual NA and
5-HT reuptake
inhibitor
Duloxetine
Pitsikas. Curr Opin Investig Drugs. 2000;1:116.
Goldstein et al. J Clin Psychiatry. 2002;63:225.
Pros
Cons
Higher remission
Insomnia
Effective in some
pain syndromes
(but so are
similar drugs)
Asthenia
No increase in
blood pressure?
Nausea
Urinary retention
BIOMEDICAL ANTIDEPRESSANT
TREATMENTS: MONOTHERAPIES
C. Monoamine receptor antagonists
1. Serotonin receptor antagonists
a. Trazodone (Desyrel®)
b. Nefazodone (Serzone®-withdrawn
2004)
2. NE/5-HT receptor antagonist
a. Mirtazapine (Remeron®)
Nefazodone (1994)
Cl
N
N
N
N
N
O
Nefazodone
O
Mechanism
of Action
Pros
Cons
Antagonist of postsynaptic
5-HT2 receptor
Similar efficacy to
TCAs + SSRIs (?)
Somnolence
Weak and transient
5-HT and NA reuptake
inhibitor (prob. not
significant)
Improved sleep structure
vs SSRIs
Dizziness
Fewer sexual side effects
Very rare liver failure
Metabolized to equally
active hydroxynefazodone
Schatzberg et al. J Clin Psychiatry. 2002;63:18.
Kent. Lancet. 2000;355:911.
Nausea
Hypotension
BID dosing and slow
dose titration
Mirtazapine (1996)
Mechanism
of Action
Antagonist of
central presynaptic
2-adrenergic
autoreceptors on
NA neurons and
heteroceptors
N
N
N
CH3
Mirtazapine
on 5-HT neurons
5-HT2 and 5-HT3
antagonist
Pros
Unique
pharmacology
Ease of dosing
Lower
orgasmic
dysfunction
Can be
combined
with SSRIs
Use in elderly
Anttila and Leinonen. CNS Drug Rev. 2001;7:249.
Kent. Lancet. 2000;355:911.
Cons
Somnolence
Weight gain
BIOMEDICAL ANTIDEPRESSANT
TREATMENTS: MONOTHERAPIES
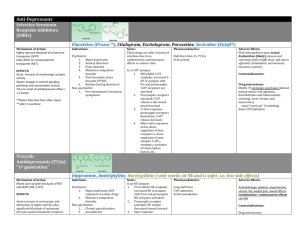
D. Tricyclics (TCAs) and related heterocyclics
1. Tertiary amines
a. Amitriptyline (AMI; Elavil®)
b. Imipramine (IMI; Tofranil®)
c. Clomipramine (CMI; Anafranil®)
d. Doxepin (DOX; Sinequan®)
e. Trimipramine (Surmontil®)
2. Secondary amines
a. Nortriptyline (NOR; Pamelor®, Aventyl®)
b. Desipramine (DMI; Norpramin®)
c. Protriptyline (PRO; Vivactyl®)
d. Amoxapine (Asendin®)
3. Tetracyclics
a. Maprotiline (Ludiomil®)
Tricyclic Antidepressants (TCAs):
Proposed Mechanism of Action
NA
Synaptic NA
NA
NA
NA
NA
NA
NA
NA
NA
Reuptake
transporters
NA
NA
NA
NA
TCA-inhibition
of NA + 5-HT
reuptake transporters
Stimulation of
postsynaptic
intracellular
processes
Synaptic 5-HT
5-HT
5-HT
5-HT
5-HT
5-HT
5-HT
5-HT
5-HT
5-HT
5-HT
NA = noradrenaline; 5-HT = serotonin.
Kandel et al. Principles of Neural Science. 1991.
5-HT
5-HT
Tricyclic Antidepressants (TCAs):
Pros/Cons
Pros
Effective in 60%-70%
of patients
Potent NA reuptake inhibitors
Some are also potent 5-HT
reuptake inhibitors
Analgesic effects
Feighner. J Clin Psychiatry. 1999;60(suppl 4):4.
Cons
Interact with cholinergic,
histaminic, and adrenergic
receptors, causing
– Dry mouth
– Urinary hesitance
– Blurred vision
– Constipation
– Sedation
– Weight gain
– Orthostatic hypotension
Cardiac conduction effects
Discontinuation syndrome
Potentially lethal in overdose
BIOMEDICAL ANTIDEPRESSANT
TREATMENTS: MONOTHERAPIES
E. Monoamine oxidase inhibitors (MAOIs)
1. Hydrazines
a. Phenelzine (Nardil®)
b. Isocarboxazid (Marplan®)
2. Non-hydrazine
a. Tranylcypromine (Parnate®)
[b. Selegiline {deprenyl} (Eldepryl®)]
Monoamine Oxidase Inhibitors (MAOIs):
Proposed Mechanism of Action
NA
NA
Synaptic NA
NA
NA
NA
NA
NA
MAO
NA
NA
NA
NA
NA
NA
Reuptake
transporters
MAO-inhibition
prevents
breakdown
of NA + 5-HT
NA
NA
NA
Stimulation of
postsynaptic
intracellular
processes
Synaptic 5-HT
5-HT
5-HT
5-HT
5-HT
5-HT
5-HT
5-HT
MAO
NA
5-HT
5-HT
5-HT
5-HT
5-HT
5-HT
5-HT
5-HT
5-HT
5-HT
NA = noradrenaline; 5-HT = serotonin.
Kandel et al. Principles of Neural Science. 1991.
Older Monoamine Oxidase Inhibitors
(MAOIs): Pros/Cons
Older MAOIs
– Irreversibly inhibit MAO-A and MAO-B
– Enhance synaptic levels of all 3 monoamines
Pros
– Effective in 60%70% of patients
– Some patients
(eg, those with
atypical depression)
may respond better
to MAOIs
Cons
–
–
–
–
–
Feighner. J Clin Psychiatry. 1999;60(suppl 4):4.
Lotufo-Neto et al. Neuropsychopharmacology. 1999;20:226.
Food restrictions
Orthostatic hypotension
Weight gain
Sexual dysfunction
Potentially lethal drug
interactions with opiates,
SSRIs, sympathomimetics
BIOMEDICAL ANTIDEPRESSANT
TREATMENTS: MONOTHERAPIES
F. NMDA Antagonists
1.Excitatory amino acid (EAA)
release inhibitor
a. Lamotrigine (Lamictal®)
BIOMEDICAL ANTIDEPRESSANT
TREATMENTS: MONOTHERAPIES
II. MOOD STABILIZERS (THYMOLEPTICS)
A. Lithium (Li; Li2CO3, LiCl)
B. Anticonvulsants
1. Valproate (VPA; Depakote®)
2. Carbamazepine (CBZ; Tegretol®)
BIOMEDICAL ANTIDEPRESSANT
TREATMENTS: MONOTHERAPIES
III. STIMULANTS
Older
A. Dextroamphetamine (Dexedrine®)
B. Methylphenidate (Ritalin®)
C. Pemoline (Cylert®)
Novel
D. Modafinil (Provigil®)
E. Atomoxetine (Strattera®)
BIOMEDICAL ANTIDEPRESSANT
TREATMENTS: MONOTHERAPIES
IV. ELECTROCONVULSIVE THERAPY (ECT)
A. Unilateral
B. Bilateral
V. SURGICAL APPROACHES
A. Orbitofrontal leucotomy
B. Stereotactic subcaudate tractotomy
C. Stereotactic limbic leucotomy
VI. COMBINATION BIOMEDICAL
APPROACHES
Definition:
Simultaneous use of two or more
different drugs acting on the core
symptoms of affective illness
COMBINATION MONOTHERAPY AGENTS
FOR DEPRESSION
1. Multiple primary antidepressants (agents
with different mechanisms of action)
Examples:
• SSRI+NRI
• MRTZ+reuptake inhibitor
EXCEPTIONS: MAOI+reuptake inhibitor
2. Thymoleptics (esp. Li)
3. Stimulants
4. ECT
OTHER COMBINATION AGENTS
FOR DEPRESSION
1.
2.
3.
4.
5.
6.
7.
Benzodiazepines
Neuroleptics (antipsychotics)
Gabapentin
Triiodothyronine (T3)
Estrogen, testosterone
5-HT1A antagonists (pindolol)
2-adrenoceptor antagonists (e.g.,
yohimbine, idazoxan)
8. DA receptor agonists (e.g., pergolide,
bromocriptine, pramipexole, ropinirole)
VII. NOVEL BIOMEDICAL
APPROACHES TO DEPRESSION
1. Pharmacologic
2. Neurophysiologic stimulation
NOVEL PHARMACOLOGIC
APPROACHES TO DEPRESSION
1. Novel anticonvulsants
a. Topiramate (Topamax®)
b. Levetiracetam (Keppra®)
c. Oxcarbazepine (Trileptal®)
d. Tiagabine (Gabatril®)
2. Antiglucocorticoids
a. Ketoconazole
b. Metyrapone
c. Aminoglutethimide
3. Thyroxine (high-dose T4)
4.
5.
6.
7.
8.
Inositol
DHEA
Fatty acids (Omega-3, EPA)
Tramadol
Hypericum perforatum (St.
John’s wort)
9. S-adenosyl methionine
(SAM-e)
10. Mifepristone (RU-486)
11. Riluzole
12. Substance P antagonists
13. CRF antagonists
14. Reboxetine (Vestra)
15. Gepirone (5-HT1A agonist)
16. Selegiline Transdermal
NOVEL NEUROPHYSIOLOGIC STIMULATION
APPROACHES TO DEPRESSION
1. Continuation ECT
2. Repetitive transcranial magnetic
stimulation (rTMS)
3. Magnetic seizure therapy (MST)
4. Vagus nerve stimulation (VNS)
5. Deep brain stimulation (DBS)
VNS Pulse Generator & Lead
• Pacemaker-like pulse generator
• Bipolar lead with two stimulating
electrodes
• Intermittent stimulation
– 30 sec on/5 min off
– 24 hours/day
• On-demand therapy mode
• 10.3 mm thick
• Weighs 38 grams
• Battery life of 8-12 years (Model 101)
Vagus Nerve Stimulation
• Pulse generator programming controlled through
a telemetric wand attached to a PC
• ON/OFF cycle is programmable
• Typical cycle:
– 30 sec ON
– 5 min OFF
VIII. PSYCHOSOCIAL ANTIDEPRESSANT
TREATMENTS
• Cognitive therapy
• Behavior therapy
• Interpersonal psychotherapy
• Brief psychodynamic therapy
• Social skills training
IX. OTHER SOMATIC ANTIDEPRESSANT
TREATMENTS
• Sleep deprivation
• Light therapy
• Exercise
• Complementary and alternative
therapies
Evolution of Antidepressants
MAOIs
1950s
TCAs
1950s
SSRIs
1980s
Mixed reuptake
inhibitors/
Receptor antagonists
1990s
Peptide
antagonists,
glutamate
modulators
and other novel
therapies
2000 and
beyond
Unmet Needs With Current
Antidepressant Therapies
20%-40% of patients do not respond to any single
antidepressant
~50% of patients who respond have significant
residual symptoms
Relapses are common, particularly after
discontinuation of therapy
Suboptimal tolerability and side-effect profiles
Low long-term adherence
Crown et al. J Clin Psychiatry. 2002;63:963.
Pampallona et al. Br J Psychiatry. 2002;180:104.
DSM-IV BIPOLAR DISORDERS
Bipolar I
Bipolar II
Cyclothymia
Manic
Hypomanic
Hypomanic Sx
Hypomanic
Depressed
Depressive Sx
Mixed
Depressed
Conceptual Problems in Classifying
Treatments for Bipolar Disorder
• Antimanics
• Antidepressants
• Thymoleptics (Mood Stabilizers)
ANTIMANIC TREATMENTS
I.
Lithium
II.
Divalproex (Valproate; Depakote®)
III. Atypical neuroleptics‡
III. Carbamazepine (Tegretol®)*
IV. Other neuroleptics*‡
V.
Electroconvulsive therapy (ECT)*
* Not FDA-approved for mania
‡
Mood-stabilizing properties of all such drugs not fully
established
Lithium
Mechanism: 5-HT and Ach function, DA function; PI
turnover; adenylate cyclase activity; regulation of G protein
and PKC activity
Dose: 600 - 2400 mg/day (0.5-1.5 mmol/L)
Pros:
Efficacy in mania established, with largest
supporting database
Response predictors known
Cons :
Poor tolerance, patient acceptance, narrow
therapeutic index
Tremor / neurocognitive effects, weight gain, renal
toxicity, nausea, acne, hair loss, hypothyroidism
Signs and Symptoms of Lithium Toxicity
Mild:
Impaired concentration, lethargy, irritability,
muscle weakness, tremor, slurred speech,
nausea [plasma lithium = 1.0 - 1.5 meq/L]
Moderate: Disorientation, confusion, drowsiness,
restlessness, unsteady gait, coarse tremor,
dysarthria, muscle fasciculations, vomiting
[plasma lithium = 1.5 - 2.5 meq/L]
Severe:
Impaired consciousness (with progression
to coma), delirium, ataxia, generalized
fasciculations, extrapyramidal symptoms,
convulsions, impaired renal function
[plasma lithium > 2.5 meq/L
Divalproex (Valproate)
Mechanism: GABA synthesis and release, GABA
catabolism, effects of GABA at receptor; regulation of
PKC activity
Dose: 750 - 2500 mg/day (50-125 g /mL)
Pros:
Efficacy in mania established
Better than Li in mixed states and rapid cyclers
Well-tolerated
Cons :
? Efficacy in prophylaxis
Weight gain, nausea, hair loss, tremor,
platelets, liver & pancreas toxicity, ?polycystic
ovary disease
Atypical Neuroleptics
1.
2.
3.
4.
5.
6.
Clozapine (Clozaril®)*
Olanzapine (Zyprexa®)
Risperidone (Risperdal®)
Quetiapine (Seroquel®)
Ziprasidone (Geodon®)
Aripiprazole (Abilify®)
*Not FDA-approved for mania
Atypical Neuroleptics in Bipolar Disorder:
Considerations
•
Effective in acute mania (as are conventional
neuroleptics).
•
Superior to conventional neuroleptics with
respect to adverse effects.
•
Possibly heterogeneous mechanisms of action
and clinical effects with respect to each other.
•
Possible thymoleptic properties.
•
Limitations
–
Limited long-term data
–
Adverse effects
–
Aggressive marketing push
Carbamazepine
Mechanism: NE, DA, GABA function; adenylate
cyclase activity; blocks adenosine receptors
Dose: 400 - 1800 mg/day (4-15 g/mL)
Pros:
Efficacy in mania established
Usually well-tolerated
Cons:
? Efficacy in prophylaxis
Ataxia and neurocognitive effects, weight gain,
nausea, hair loss, leukopenia, hepatotoxicity,
Na, hepatic enzyme induction
Oxcarbazepine as alternative?
BIPOLAR ANTIDEPRESSANT
TREATMENTS
I.
Lamotrigine
Lamotrigine
Mechanism: Inhibits release of excitatory amino acids
(EAAs) (e.g., glutamate, NMDA)
Dose: 100 - 400 mg/day (usu. 200 mg/day)
Pros:
– Efficacy in preventing bipolar depression
relapse
– Usually well-tolerated
Cons :
– ? efficacy in acute bipolar depression; doubtful
efficacy in acute mania or mania prophylaxis
– Slow dose titration
– VPA inhibits LMTG metabolism by 50%;
– CBZ increases LMTG metabolism by 100%
– Rash can lead to Stevens-Johnson
Other Agents Reported to have Antimanic
or Thymoleptic Properties
1.
2.
3.
4.
5.
6.
7.
8.
9.
10.
Calcium channel antagonists (esp. verapamil)
Benzodiazepines (clonazepam, lorazepam) (high
doses)*
Thyroid hormone (hypermetabolic doses)*
Tryptophan*
Clonidine
Inositol
Donepezil
Novel anticonvulsants: Oxcarbazepine (Trileptal®),
Tiagabine (Gabatril®), Zonisamide (Zonegran®),
Levetiracetam(Keppra®)
Transcranial magnetic stimulation (rTMS)
Surgery (esp. subcaudate tractotomy)
*Primarily adjunctive (used in combination with lithium).
Psychosocial Interventions in the
Management of Bipolar Disorder
•
•
•
•
•
•
•
Psychoeducation
Individual, family, and group
psychotherapies
Support groups
Management of comorbid conditions
Maximization of adherence
Legal planning (e.g., durable power of
atty.)
Advocacy
Evolving Conceptualizations in the
Treatment of Bipolar Disorder: Implications
for the use of Antimanics, Antidepressants,
and Thymoleptics
Depression, acute
Depression, prophylactic
Mania, acute
Mania, prophylactic
Rapid-cycling
Subsyndromal mood symptomatology
Subsyndromal other symptomatology
Approaches to Combination Treatment in
Bipolar Disorder
Acknowledge that combinations are the rule rather than the
exception
Use evidenced-based approach--but be aware of strengths and
limitations of RCTs
Consider agents with different mechanisms of action
Be aware of possible synergistic effects
Therapeutic (e.g., Lithium + Thyroid hormone)
Toxic (e.g., VPA + Lamotrigine)
Consider cost/benefit ratio
Use "N=1 clinical trial strategy": Evaluate cost/benefit of each
added agent in a trial of adequate duration at adequate dose;
discontinue agents without sufficient benefit
Strive for simplicity
BUTLER HOSPITAL
MOOD DISORDERS RESEARCH
PROGRAM
Department of Psychiatry and Human Behavior
Brown Medical School
345 Blackstone Blvd
Providence, RI 02906
TEL 401- 455-6537
FAX 401- 455-6534