Treating Cancer with Charged Particles
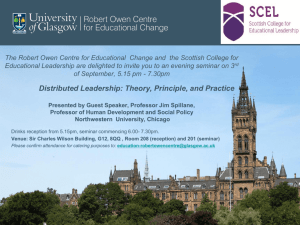
advertisement

Treating Cancer with Charged Particles Claire Timlin Particle Therapy Cancer Research Institute, Oxford Martin School, University of Oxford Slides are a PTCRi group effort. Contents • Introduction to Charged Particle Therapy • Production and Delivery of Medical Proton Beams • Introduction to the Particle Therapy Cancer Research Institute • Research Projects – – – – – Malignant Induction Modelling Virtual Phantoms Data Recording and Sharing Biological Effectiveness of Particle Beams Clinical Ethics of Charged Particle Therapy • Proton Therapy in the UK 2 PP Seminar 30/11/2010 Introduction to Charged Particle Therapy 3 PP Seminar 30/11/2010 Development of Radiotherapy • 1895: Wilhelm Conrad Rontgen discovers Xrays • 1896: First x-ray treatment 3 months later! • 1898: The Curies discover radium • 1905: First Curie therapy – birth of brachytherapy 4 PP Seminar 30/11/2010 The Evolution of External Beam Radiation Therapy 1950’s The First Cobalt Therapy Unit and Clinac 1970’s Cerrobend Blocks Electron Therapy Standard Collimator 5Slide courtesy of Prof. Gillies McKenna 1980’s Computerized 3D CT Treatment Planning 1990’s Multileaf Collimator Dynamic MLC and IMRT High resolution IGRT PP Seminar Particle Therapy 2000’s? Functional Imaging 30/11/2010 History of Proton Therapy • 1946: – Therapy proposed by Robert R. Wilson, Harvard Physics • 1955: – 1st Proton Therapy at Lawrence Tobias University of California, Berkeley • 1955-73: – Single dose irradiation of benign CNS lesions Proton Therapy Centres Worldwide http://www.uhb.nhs.uk/ProtonsBirmin gham/background/facilities.htm • 2010: – > 67 000 patients had been treated with protons worldwide – 29 proton therapy centres operating worldwide – ~ 20 more planned or under construction 6 PP Seminar 30/11/2010 Low vs. High Linear Energy Transfer Radiation Sparsely ionising radiation (low-LET) e.g. -rays, -particles Low concentration of ionisation events electron tracks Densely ionising radiation (high-LET) e.g. -particles C6+ ions High concentration of ionisation events 7Slide courtesy of Dr Mark Hill PP Seminar DNA 30/11/2010 Radiation Induced Damage • Central Nervous System – blindness, deafness, paralysis, confusion, dementia, chronic tiredness • Bowel – colostomy, chronic bleeding. • Lung – shortness of breath – pneumonias • Kidney – renal failure and hypertension • Reproductive organs – sterility • Everywhere: – severe scarring in medium to high dose regions – possible increase in induced cancers in low-medium dose regions • Therefore must avoid dose to normal tissues.......... 8 PP Seminar 30/11/2010 Conformal Radiotherapy • Advantages – Reduced dose to organs at risk • Fewer complications – Increased tumour dose • Higher probability of tumour control • Disadvantages – Requires precise definition of target – Complicated planning and delivery therefore expensive! – Large volumes of lowintermediate dose (e.g. IMRT) -> secondary cancers 9 PP Seminar 30/11/2010 Photon vs. Proton/Ion Depth-dose Curve Photons Dose Protons Carbon Ions Depth • High energy photons favoured over low energies due to skin sparing • Dose falls off but not to zero 10 PP Seminar • Density of ionizations increase as the particles slow down -> peak in dose • No dose past peak 30/11/2010 The Spread Out Bragg Peak Incident energy is modulated to form spread out Bragg Peaks the cover the tumour Unnecessary dose Skin sparing Unnecessary dose 11 PP Seminar 30/11/2010 Combining Fields 80 60 50 150 0 0 40 X-Rays 12 150 Protons/Ions PP Seminar 30/11/2010 IMRT vs. Proton Therapy 13 PP Seminar 30/11/2010 Medulloblastoma in a Child X-rays 100 60 With Xrays 10 With Protons 14 PP Seminar 30/11/2010 Orbital Rhabdomyosarcoma Protons/Ions X-Rays 15 PP Seminar 30/11/2010 Courtesy T. Yock, N. Tarbell, J. Adams Proton Therapy in Action Anaplastic Ependymoma Brain Tumour http://news.bbc.co.uk:80/1/hi/england/7784003.stm 15th Dec http://news.bbc.co.uk/1/hi/england/7795909.stm 19th Dec http://news.bbc.co.uk/1/hi/england/7906084.stm 23rd Feb Pre-treatment During-treatment Post-treatment CPC, Friedmann, NEJM, 350:494, 2004 16 Slide courtesy of Prof. Gillies McKenna PP Seminar 30/11/2010 Production and Delivery of Medical Proton Beams 17 PP Seminar 30/11/2010 Beam Acceleration HIT, Germany • Cyclotron – – – – – – • Synchrotron – – – – – – Protons up to ~250 MeV Requires degraders High current Small(ish) Simple(ish) Main Manufacturers • IBA ,Varian Carbon up to 400MeV/ Dynamic energy change Lower current Bigger More complicated Main Manufacturers • Hitachi, Siemens – Best choice for protons at present? – Only viable choice for heavy ion therapy at present? Future accelerators that do the job better? e.g FFAG, Laser Driven? 18 PP Seminar 30/11/2010 Beam Transport • Gantries • Fixed Beams 19 •Clinical Indications •Flexibility •Space •Cost PP Seminar 30/11/2010 Beam Delivery - Scanning • Parallel proton pencil beams are used (~3mm σ ) • Sweeper magnets scan the target volume in transverse plane (steps of 4mm) • One litre target volume typically 10000 spots are deposited in less than 5min. Beam direction Target Patient Beam direction Target Patient 20 PP Seminar 30/11/2010 Beam Delivery - Scattering Courtesy of T. Lomax, PSI, Switzerland. 21 PP Seminar 30/11/2010 Introduction to the Particle Therapy Cancer Research Institute 22 PP Seminar 30/11/2010 The Particle Therapy Cancer Research Institute PTCRi 23 PP Seminar 30/11/2010 The PTCRi Collaborators • Also work closely with (not an exhaustive list!): – – – – – – – Oxford Radcliffe Hospitals Trust CERN Mayo Clinic, Minnesota, USA RAL Ethox, University of Oxford Maastro, Maastrict, Netherlands Electa-CMS, Germany • For more info on the PTCRi team see: http://www.ptcri.ox.ac.uk/people/ 24 PP Seminar 30/11/2010 Challenges in Charged Particle Therapy Radiobiological modelling validated with existing cell, small animal and clinical data Investigating equipoise and clinical utility in collaboration with ETHOX. Oxford PT centre or collaboration? • Which particle (, p, C)? – Radiobiology – Cost-effectiveness New, improved radiobiological experiments on cells (and small animals)? • Which clinical indications? – Clinical ethics • Treatment Planning and Delivery Database for multiple parallel radiobiological calculations (with Jim Loken) -> sensitivity analyses EU Projects: ULICE, PARTNER, ENLIGHT. – MC vs. treatment planning algorithms – Biological heterogeneity – Uncertainty in radiological models and parameters At treating centres – Organ Motion • Recording and sharing clinical data • Late effects e.g. carcinogenesis FFAG (PAMELA), laser driven accelerators. 25 Voxelised virtual phantom Radiobiological modelling validated with existing cell, small animal and clinical data. • Accelerator design PP Seminar 30/11/2010 Novel Accelerator and Gantry Design 26 PP Seminar 30/11/2010 FFAG Accelerator Fixed Field Alternating Gradient synchrotrons, FFAGs, combine some of the main advantages of both cyclotrons and synchrotrons: • Fixed magnetic field – like a cyclotron ‒ fast cycling ‒ high acceptance ‒ high intensity ‒ easy maintenance ‒ high reliability • Strong focussing – like a synchrotron ‒beam extraction at any energy ‒higher energies or ion acceleration 27 PP Seminar 30/11/2010 FFAG Gantry A PAMELA NS-FFAG Gantry conceptual design Conventional Carbon Gantry at Heidelberg •Gantry is a beam delivery system which can rotate around the patient in 3600 •Delivering beams, avoiding critical organs and minimal transverse irradiation •Consists of bending magnets, focusing magnets, beam scanning system •Only one C- ion gantry existing at present , weighs ~600 tons •Use of FFAG technique is expected to reduce the size considerably 28 PP Seminar 30/11/2010 Laser Driven Ion Acceleration plasma sheath metal foil Pulsed laser -++ -++--+++-++---+ + -- eions (Target Normal Sheath Acceleration-TNSA) Contaminant layer •High intensity (>1019 Wcm-2) laser irradiate thin foil (~10μm) •Laser electric field is higher than atomic electron binding energy (~1016 Wcm-2) and the surface will be instantly ionised and plasma is created. •Laser electric field and magnetic field drive plasma electrons into the target with relativistic energies •Some of the energetic electrons escapes through the rear side of the target (non irradiated surface) and large space charge is generated on the rear surface. •This sheath field is of the order of ~1012 Vm-1, ionises rear surface and accelerate ions to MeV energies (generally present in the form of contaminants) •Any ion species can be accelerated 29 PP Seminar 30/11/2010 Advantages and Challenges of Laser Driven Ion Acceleration Advantages •Extreme laminarity: rms emittance < 0.002 mm-mrad •Short duration source: ~ 1 ps •High brightness: 1011 –1013 protons/ions in a single shot (> 3 MeV) •High current : kA range •minimal shielding and expensive magnets are not required Challenges •Clinical energies are not achieved yet (~65MeV proton at present) •Energy spread, repetition rate, neutron contamination, beam stability… 30 PP Seminar 30/11/2010 Malignant Induction Modelling 31 PP Seminar 30/11/2010 Radiation Action on Cells Direct DNA damage DNA dsb Repair No repair Mis-repair Mutation Cell survival 32 Slide courtesy of Prof. Boris Vojnovic Transformation PP Seminar Cell death 30/11/2010 Induction and cell kill What is the form of the induction function? Linear, quadratic? Probability of transforming a cell 33 Cell killing Induction Form of cell killing function known with some certainty at clinical energies, the parameters are tissue dependent and can have large uncertainties. Probability the cell survives Probability of inducing a potentially malignant mutation Risk needs to be •accurately modelled •confirmed experimentally •taken into account when deciding on the optimal treatment plan PP Seminar 30/11/2010 Voxelised 3D Calculations of Biological Endpoints • • 34 Model and parameter sensitivity analyses Validation with clinical data on secondary malignancies PP Seminar 30/11/2010 Virtual Phantoms 35 PP Seminar 30/11/2010 Virtual Phantoms • Virtual phantom provides an anthropomorphic reference geometry for Monte Carlo particle transport • Two flavours: 36 Computationally intensive voxellised phantoms Geometrically simple mathematical phantoms (3D equivalent of pixels) (cylinders, spheres, cones, etc...) • Nowadays have the memory and processing power to deal with megavoxels PP Seminar 30/11/2010 Virtual Phantoms • ICRP Reference Man consists of 7 million voxels (3D pixels) • Each voxel assigned an organ type that specifies density, elemental composition, etc. • Size and masses typical of average man • Female phantoms also exist, children being developed 37 PP Seminar 30/11/2010 PTCRi Phantom work • ICRP man has been converted to a simulated CT scan – can be input into treatment planning software • Enables assessment of TPS accuracy by comparison to Monte Carlo: – Accuracy of the TPS method of mapping CT number (x-ray linear attenuation coefficient) to proton stopping power – Effect of air cavities and tissue boundaries on the range and profile of proton beams • Also interested in examining the second cancer induction risk due to scatter from the beam head. 38 PP Seminar 30/11/2010 Data Recording and Sharing 39 PP Seminar 30/11/2010 EU Projects: ENLIGHT and PARTNER http://enlight.web.cern.ch 40 Slide courtesy of Faustin Roman http://partner.web.cern.ch PP Seminar 30/11/2010 40 EU Project: ULICE • ULICE: Union of Light Ion Centres in Europe • Aims: – Transnational access to particle radiotherapy facilities – Facilitating joined up research across Europe – Addressing efficacy and cost-benefits for CPT • Methods: ‒ developing and recommending standards for key observations and measurements in CPT ‒ facilitate data sharing and reuse through pan-European collaborative groups ‒ at the point at which key European centres are commissioning facilities 41 PP Seminar 30/11/2010 European Heavy Ion Centres Centres in Europe treating with heavy ions NRoCK (Kiel) RKA (Marburg) HIT MedAustron (Heidelberg) (Wiener Neustadt) ETOILE (Lyon) Connect centres ... ... and make most of available data! CNAO (Pavia) 42 PP Seminar 30/11/2010 Data Sharing and Interpretation - Challenges Platform for translational research Medical Users Doctor and clinical practiseclinicians (1/2) from multiple disciplines with specific views on data researchers Biologist across Europe with different levels of technical knowledge Statistician data owners Chemist Physicists with different privileges Common access point Data from multiple disciplines with specific terminologes stored across Europe In various independent repositories with different ethical and legal requirements 43 PP Seminar 30/11/2010 GRID? : Coordinated resource sharing and problem solving in dynamic, multi-institutional virtual organizations… (I. Foster et al) Hadrontherapy Information Sharing Platform (HISP) Prototype connecting: • Users • Data sources with • Grid resources • Security framework • Data integration services by • Portals • Interfaces 30/11/2010 Slide courtesy of Faustin Roman PP Seminar USECASES: 1. REFERRAL 2.RESEARCH 44 A patient opinion… http://www.nature.com/nm/journal/v16/n7/full/nm0710-744.html 30/11/2010 PP Seminar Slide courtesy of Faustin Roman 45 Biological Effectiveness of Particle Beams 46 PP Seminar 30/11/2010 Relative Biological Effectiveness • Photons and protons (at clinical energies) have similar biological effects – Clinically a modifier (RBE) of 1.1 is applied to physical dose for protons • For heavier ions (e.g. C) RBE has large uncertainties • RBE needed* to calculate physical dose to administer to achieve prescribed biological dose *maybe there is a better way? New treatment regimes requiring new methods of optimisation? 47 PP Seminar 30/11/2010 RBE vs. Dose for Protons Where does the 1.1 come from? Paganetti et al.: Int. J. Radiat. Oncol. Biol. Phys. 2002; 53, 407 48 PP Seminar 30/11/2010 RBE vs. Dose for Protons More data is required to determine magnitude of proton RBE variation with dose for a variety of tissues Where? CERN? V79 Cells. Wouters et al.: Radiat Res 1996 vol. 146 (2) pp. 159-70 49 PP Seminar 30/11/2010 Modeling RBE vs. Dose for Carbon RBE increases with decreasing dose Analysis of 77keV Data from Suzuki et al, IJRBP, Vol. 48, No. 1, pp. 241–250, 2000 50 PP Seminar 30/11/2010 RBE – The Solution? • Radiobiological experiments – GSI, Germany – Gray Institute for Radio-oncology and Biology – Future – CERN? • Validated (or at least validatable!) radiobiological models – Mechanistic vs. empirical? 51 PP Seminar 30/11/2010 Clinical Ethics of Charged Particle Therapy 52 PP Seminar 30/11/2010 Ethical Issues in CPT • Controversy among the medical community about CPT • Few Randomised Control Trials (RCTs), the “gold standard” for evidence of clinical effectiveness • Dose distributions obtained with CPT mostly superior conventional radiotherapy • RCTs are unethical if they lack “equipoise” • Biological dose uncertainties enough to restore equipoise? • Limited number of centres – What is the optimal use? 53 • Paper to discuss issues • Workshop next year PP Seminar 30/11/2010 Proton Therapy in the UK 54 PP Seminar 30/11/2010 Proton Therapy in UK - Clatterbridge • World First: hospital based proton therapy at Clatterbridge, near Liverpool • >1700 patients with ocular melanoma; local control ~97%. • Targets the cancer • Avoids key parts of eye (optic nerve, macula, lens) 55 PP Seminar 30/11/2010 Proton Therapy in UK – Where Next? • http://www.bbc.co.uk/news/uk-england-11519263 • Decision of Department of Health - 17th September 2010 • “The three potential trial sites are the Christie NHS Foundation Trust in Manchester, University College London Hospital and University Hospitals Birmingham NHS Foundation Trust.” • Research and treatment centre at Oxford? • Centres should: – Treat patients currently eligible for treatment abroad – Optimise treatment regimes – Expand indications – Research biological effectiveness of protons and heavier ions 56 – Train staff............ PP Seminar 30/11/2010 Summary • CPT is a rapidly expanding field • Many challenges still to be tackled – Optimal treatments for protons • • Fractionation schemes Dose delivery – Heavy Ions • • – – – – – • Radiobiological uncertainties Treatment planning and delivery uncertainties Organ motion Cost-effectiveness Clinical ethics Achieved by – – – – – 57 Which ions? For which indications? Accelerator development Radiobiological modelling and experiments Advanced treatment planning and delivery techniques e.g. MC, proton radiography Consistent data recording and data sharing Clinical studies with long-term follow-up PP Seminar 30/11/2010 • Thank you for listening..... ......any questions? 58 PP Seminar 30/11/2010 • Back up slides 59 PP Seminar 30/11/2010 Contributions to the Proton Bragg Peak Coulomb interactions with atomic electrons Energy spread and energy loss differences Nuclear interactions with atomic nuclei 60 Illustrations courtesy of M. Goitein PP Seminar 30/11/2010 ULICE - Work Package 7 • seeks to provide automatic support for the management and use of these standards – customise components of information systems and analysis engines from the definition of the data – better documentation and design leads to transparency and reliability of results 30/11/2010 PP Seminar 61 Contributions to the Proton Bragg Peak Coulomb interactions with atomic electrons Energy spread and energy loss differences Nuclear interactions with atomic nuclei 62 Illustrations courtesy of M. Goitein PP Seminar 30/11/2010 The combined effect (in water) Used for imaging Credit: 63 Historically Currently used in used in radiotherapy radiotherapy Figure by MIT OpenCourseWare. PP Seminar Transferred to charged particles Scattered 30/11/2010 Curing Cancer with X-rays Dose Linac 64 PP Seminar Slide courtesy of Ken Peach 30/11/2010 Can we do better? Dose The Bragg Peak Proton 65 PP Seminar Slide courtesy of Ken Peach 30/11/2010 66 PP Seminar 30/11/2010 Proton Therapy 67 PP Seminar 30/11/2010