Personal Philosophy of Nursing
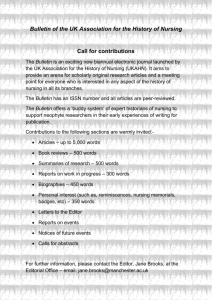
advertisement

PERSONAL PHILOSOPHY OF NURSING Running Head: PERSONAL PHILOSOPHY OF NURSING Personal Philosophy of Nursing Lisa Armstrong NURS 900.01: Discipline of Nursing (Fall 2012) September 14, 2012 Dr. J. Samuels PERSONAL PHILOSOPHY OF NURSING Personal Philosophy of Nursing In my final clinical practicum at the University of New Hampshire, I had the opportunity to work with Manchester VNA & Hospice in a community setting visiting hospice patients in their homes. Throughout this time, I kept a weekly journal reflecting my thoughts, feelings, and general experiences. When asked to consider a nurse/patient scenario encountered in my work, a particular situation sprung immediately to mind, especially as it is relatable to the nursing metaparadigms and themes under discussion. The patient, Dick (pseudonym) was in his final illness trajectory of metastatic cancer. He was extremely cachectic, evidenced by signs of extreme muscle wasting, and he had a large cantaloupe-melon sized tumor located below his liver to the right of his abdomen which was extremely vascularized and unstable. The patient had been receiving blood transfusions at his local hospital, and care via his primary care physician, who had eventually decided that the blood transfusions were not providing any noticeable symptom relief, and that his pain was poorly managed. The patient was subsequently referred to hospice for home-care services. In the initial meeting with Dick and his wife, Jane (pseudonym) it was clearly evident that physical neglect and psychological factors were in play and that the care situation was extremely tenuous. Jane was unwelcoming of hospice support services, and felt that we were “taking over” and “intruders” in her home. She was angry, mistrustful, and uncooperative. Upon initial assessment of Dick, we found him in a bed soaked with urine with towels beneath him. He had several decubitus ulcers on his coccyx and buttocks ranging from stage 2 and 3, to unstageable, as well as multiple occipital, scapula, elbow, and foot ulcers. Dick refused to be touched, stating that he was in too much pain. When Jane was asked what time Dick was last medicated, she stated “I’m no Kevorkian, I’m not giving him any of that PERSONAL PHILOSOPHY OF NURSING morphine shit.” When Dick was asked whether he would like something to take away the pain, he shouted “yes, yes, yes!” but then almost immediately after his outburst glanced at Jane and said “do you think I need it?” When prompted about external support, Jane stated that she did everything herself and was frankly overwhelmed with his care, but simply didn’t trust anyone else to care for him, especially in their home. The feelings that I experienced during this interaction ranged from sorrow and despair at their situation, to anger and frustration that it hadn’t been recognized or acted upon sooner, to fear that Dick and/or Jane would not accept outside support, to the realization that this was now “our ball” and the cascade of decisions that needed to be made would directly affect Dick’s end of life process, and Jane’s perception of Dick’s death and her consequent ability to effectively transition through the grief cycle. From a moral and ethical stance, addressing neglect was our priority. Although not initially considered deliberate or malicious neglect, the patient’s physical injuries coupled with lack of pain control indicated that the caregiver’s competence was questionable and the patient’s risk for further injury was substantiated. On our first visit, although admittedly suspicious, we decided to give Jane the benefit of the doubt, and armed her with the knowledge, education, and tools to accomplish competent care. We considered her situation in the patient context of nursing diagnoses such as anxiety and fear related to death, denial, complicated grieving, caregiver role strain, ineffective coping, sleep deprivation, stress overload, moral distress, hopelessness, powerlessness, social isolation, and disturbed thought processes, and addressed each diagnosis in our plan of care and education. In developing our plan of care for Dick, we focused primarily on symptom management, tying his outcomes to Jane’s ability to care for him. We made it clear to both Dick and Jane that PERSONAL PHILOSOPHY OF NURSING in order for Dick to continue to be cared for in the home environment, Jane needed to be able to demonstrate competent care. Unfortunately, over the course of the next two weeks, it become apparent that Jane was unable, and with regards to appropriate and effective pain management, unwilling to provide competent care to Dick despite many outside resources being provided, and it was suggested that Dick be transferred to a hospice facility. However, Jane adamantly refused to allow Dick to leave the home, and at this stage, Dick’s decision-making capacity was compromised. Jane was Dick’s durable power of attorney, which added another layer of legal complexity to an already difficult situation. It was decided by the attending nurse, with the support of the organization to contact the Bureau of Elder and Adult Services (BEAS) to report neglect and request protective services at this juncture. Jane never allowed a representative from hospice back in her home again despite numerous attempts, and shortly after the report was filed, Dick reportedly died at home. This clinical nurse/patient example touches on all aspects of the nursing metaparadigm domains. From the person --Dick and Jane, to the environment --community healthcare setting, to health, --Dick’s illness, to the nursing domain, --the delivery of care by the hospice nurse. Reflecting on this complex case, and other nurse/patient interactions I have encountered, I’ve come to realize that my personal philosophy encompasses an implicit appreciation and understanding that all domains of the metaparadigm are intrinsically and extrinsically linked in multifaceted ways. I also believe that many different theories may apply to a specific set of circumstances in one, some, or all of the domains as applied to a nurse/patient interaction at any given point in time. PERSONAL PHILOSOPHY OF NURSING Lastly, I consider the central concept of ethical patterns of knowing at the very core of the nursing metaparadigm: “Ethical knowing involves clarifying conflicting values and exploring alternative interests, principles and actions. There may be no satisfactory answer to an ethical dilemma or moral distress; rather, there may only be alternatives, some of which are more satisfactory than others” (Chinn & Kramer, 2011, p.7). Since the beginning of my endeavors towards nursing, I have long pored over, consulted, considered, reflected upon, and been guided by the American Nurses Association Code of Ethics for Nurses, and submit that this code is quite possibly the driving force behind my daily practice. In almost every situation I am in, and during every decision I encounter, I try -- however fleetingly -- to consider whether the action I am taking is right, just, responsible, moral, ethical, fair, and virtuous. I do this, because I fundamentally subscribe to the assertion that I would like to be treated with the same courtesy by my fellow human beings: “To cure sometimes, to relieve often, to comfort always — this is our [nurses] work. This is the first and great commandment. And the second is like unto it – Thou shalt treat thy patient as thou wouldst thyself be treated” – Anonymous, 15th Century. I am also a proponent of the code as it extends to the concepts of general nursing praxis, an ideal which I aspire to. Outlining ethical behavior that goes beyond individual patient encounters, the code encourages nurses to actively engage and participate in further education and knowledge development, collaborate with their community to meet health needs, and empowers nurses socially and politically to further the profession of nursing in a global context. To apply my philosophy within a theoretical framework, I believe that ethics form a fundamental foundation for consideration in all nursing domains. In the person domain, ethical guidelines are employed to protect and serve the best interest of the client, across the continuum of life and health through the consistent advocacy of nonmaleficence, beneficence, autonomy, justice, and fidelity. One theoretical example of this can be found in applying Orem’s theory of PERSONAL PHILOSOPHY OF NURSING self-care and self-care deficit to this domain. In practice, the nurse strives to promote the highest level of patient autonomy, dignity, and independence in his/her care-giving, carefully balancing the need to meet self-care deficits that may be present during any given stage of an illness trajectory. Ethics in the environmental domain lends itself to Roy’s Adaptation model of persons constantly interacting within a changing environment. It is incumbent upon a nurse to recognize that a person will experience illness and wellness during many different physical and psychosocial environments during their lifetime. Such as in the case of my clinical example, environmental ethics not only plays a significant role at the micro level of care, but also at the macro level. Broader environmental ethics considers the extent to which social injustices affect equal access to acute and preventative healthcare across a patient’s entire lifespan, and how these inequalities shape the worldview of the patient as it pertains to their own role in healthcare. In the health domain, ethical knowledge can be viewed and applied intrinsically to the patient in consideration of their basic physical wellbeing using any number of traditional or contemporary theories. It is important, however to recognize that extrinsic factors also play into a person’s health, such as knowledge of historical accessibility to, and interactions with, the healthcare system, understanding the environmental and personal domains interplay, familial health history, psychosocial history, and so on. Generally speaking, the health domain extracts, combines, and utilizes knowledge from all domains in its consideration of any given situation at any given time in a nurse/patient interaction and that health decisions must be based on solid ethical evidence-based practice. The nursing domain is by far the most integral partner in the ethical pattern of knowing and where my philosophy ultimately lies. This is where I, as a future nurse practitioner, feel I PERSONAL PHILOSOPHY OF NURSING can exert the most influence. With ethical knowledge underpinning my practice, I will endeavor to consistently provide holistic and culturally competent care, ensuring that my interaction with my patients, their health and their environment not only reflects the tenets of the code of ethics, but is optimally therapeutic as well as partnership-oriented. Put simply, I seek to deliver ethical and moral care in all aspects of my nursing interactions, whether I am a patient partner, family partner, physician partner, community health partner, learning or teaching partner, research partner, or a global partner in the international profession of nursing. PERSONAL PHILOSOPHY OF NURSING References: Chinn, P.L., & Kramer, M.K. (2011). Integrated Theory and Knowledge Development in Nursing (8th ed.). St. Louis, MO: Mosby, Inc.