Medical-surgical case study - Georgina Crookes MS
advertisement

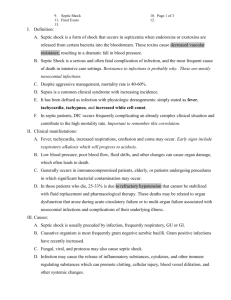
Running head: COMPREHENSIVE CASE STUDY Comprehensive Case Study Georgina Crookes University of Arizona 1 COMPREHENSIVE CASE STUDY 2 Background Information The patient of this case study includes a 42-year old woman admitted to the medicalsurgical floor due to septic shock. The patient presented in the emergency department with her primary complaint being that she felt “very sick for the past couple of days.” The patient reports having had no surgical history prior to hospitalization and the only medical history was cellulitis a couple of years ago. After performing a CBC, CMP and a urinalysis, the patient was diagnosed with septic shock, acute kidney injury and a UTI. She patient has no known drug allergies and is a full-code status. Her background includes that she is a member of the Tohono O'odham nation and has resided on the reservation for the past 30 years. She lives with her mother, sister and two nieces. The patient is a counsel representative for the district and speaks of how happy she is in her job. The patient talks about the tribe and how closely knit the community is and how supportive they have been. The patient states her role in her family is that she is a caregiver. She spoke of her younger sister being incarcerated and having to take care of her nieces while she is away, but how willing she was to take on the job. While being hospitalized she said she is not worried about how her condition has affected things at home because of how loving and supportive her family is. Developmentally the patient is appropriate as she is a productive member in her community and takes on the maternal role. She responded very appropriately and thoroughly which indicated she had proper language/ mental development. According to Erik Erikson’s psychosocial theory the patient is in the generativity versus stagnation stage. The patient should be considered to be generative due to her having established a successful career and family. The patient seems to have an understanding of the “big picture” of life, which is an important aspect 3 COMPREHENSIVE CASE STUDY at this stage. (Potter, Perry, Stockert, & Hall, 2013). The patient denies any history of tobacco, alcohol use, but does have a history of recreational cocaine use. Although she lives on the reservation with a supportive mix of people she still interacts with individuals that are negative influences. When exposed to a more negative crowd of people she was susceptible to doing recreational drug use. Physiology Many organ systems are affected during septic shock since this disease process is a systemic wide infection. The two major organ systems that this case study focuses on are the urinary system and cardiovascular system. The first organ system affected in this patient’s case would be the renal/ urinary system. The kidneys are two organs that lay in the posterior region of the abdominal cavity. They are responsible for maintaining a stable environment for cell and tissue metabolism. The kidneys specific functions include: metabolic waste products excretion, acid-base regulation, solute and water transport balance and nutrient conservation. Additionally, the functional unit of the kidney is called the nephron; its functions specifically include regulating the concentration of water and soluble substances like sodium salts by filtering the blood, reabsorbing what is needed, and excreting the rest as urine. From the kidneys urine travels down the two ureters into the bladder. The bladder is responsible for collecting urine from the kidneys and then excreting it through the urethra. The urethra extends from inside the body to an opening on the outside the body where urine exits in a process called urination (McCance, Huether, Brashers, and Rote, 2014). Additionally, the cardiovascular system has been affected which includes the heart, the blood vessels and all of the circulating blood. The heart is the organ responsible for pumping the blood to the different areas of the body. The blood vessels are the means of transportation in 4 COMPREHENSIVE CASE STUDY which the blood travels to throughout the entire body. Blood contains RBC’s, WBC’s, platelets and plasma responsible for maintain homeostasis of nutrients, wastes, and gases. With each heartbeat the heart contracts and relaxes. The heart receives deoxygenated blood, passes it through the lungs to become oxygenated and then pumps out the oxygenated blood to be circulated. The ejection fraction is the percentage of blood leaving your heart each time it contracts. The stroke volume is the amount of blood ejected by the left ventricle in one contraction and that is multiplied by the heart rate per minute to get the cardiac output. All of these factors are important for maintaining adequate circulation. Blood pressure is the measure of the pressure exerted by blood against the walls of the arterial system. This is most greatly affected again by the cardiac output, but also by the systemic vascular resistance, which opposes the movement of blood (Lewis et al., 2014). Pathophysiology Sepsis is a systemic inflammatory response to a pathogen. “Septic Shock then occurs in the presence of sepsis but additionally includes hypotension and inadequate tissue perfusion. The three major pathophysiological effects of septic shock include: vasodilation, misdistribution of blood and myocardial depression” (Lewis et al., 2014, p. 1637). Suspected organisms causing septic shock are gram-negative and gram-positive bacteria. The body’s exaggerated immune response to septic shock causes mass inflammation and coagulation release. “Cytokines are released due to the endotoxins, along with tumor necrosis factor (TNF), interleukin-1 (IL-1), and other proinflammatory mediators that act through secondary mediators such as platelet-activating factor, IL-6 and IL-8. The release of plateletactivating factor results in the formation of microthrombi and obstruction of the microvasculature” (Lewis et al., 2014, p. 1636). The results of this mass release include COMPREHENSIVE CASE STUDY 5 widespread vasodilation, platelet clumping causing endothelium damage and adhesion. “Decreased ejection fraction occurs causing ventricle dilation to increase stroke volume. This high cardiac output and low systematic vascular resistance (SVR) leads to development of hypotension and MODS,” (Lewis et al., 2014, p. 1637). Though septic shock is a complex condition that consumes many resources “approximately 500,000 cases of septic shock can be expect annually in the United States,” (Giuliano & Kleinpell, 2005, p. 140). Clinical manifestations of septic shock include fever, chills, irritability, fatigue, tachycardia, hypotension, and hyperventilation (McCance et al., 2014). The patient presented into the emergency department with a UTI of which she had no knowledge about. “During their lifetime, at least 20% of women develop at least one UTI,” (Lewis et al., 2014, p.1064). Common symptoms of a UTI would include: dysuria, frequent urination, lower abdominal pain, cloudy urine and a mild fever (McCance et al., 2014). Unfortunately, the patient went undiagnosed without antibiotics for a while and the infection then spread up into the kidneys causing pyelonephritis. This acute, severe infection progressed even further spreading into her blood stream, which put the patient into septic shock. The urinary tract area tends to normally be sterile due to the low level of acidity and abundant glycoproteins that interfere with the growth of bacteria (McCance et al., 2014). Many times organisms, such as E.coli, are introduced to the urethral opening and travel up causing an UTI. “Precipitating factors include sexual intercourse, catherization, and improper wiping,” (Lewis et al., 2014, p. 1065). Also, a woman’s urethra is much shorter than a males being only 3 to 4 centimeters versus 18 to 20 centimeters, which leaves women much more susceptible to UTIs. 6 COMPREHENSIVE CASE STUDY The patient additionally was diagnosed with acute kidney injury as her signs showed creatinine levels of 3.2, 1.6 and 2.0. The patient initially had BUN levels of 19 and 23, but levels increased to 26 (see Appendix A for rest of laboratory results). Acute kidney injury is caused from a multitude of issues but for this patient it was likely due to “toxic/inflammatory injury to kidney cell that resulted in alteration in the kidney function,” (McCance et al., 2014, p. 1360). Another possible reason for the kidney injury is due to the lack of tissue perfusion that septic shock places on the body. The inability to deliver oxygen to vital organs can caused ischemia resulting in injury. The patient has had no surgeries or procedures previously so there is no relationship of the current disease processes with the patient’s history. Physician’s Orders The patient is currently on orders for a renal diet due to her kidney dysfunction. She is being monitored on her fluid intake and is having low sodium, phosphorous and protein meals. Her activity order is for her to be up to chair and is allowed to walk ad lib. She should have assistance when ambulating due to the increased risk for postural hypotension related to possible hypovolemia. She currently has the use of SCDs for prevention of a venous thrombolytic event (VTE) with a continuous order for pulse oximetry. Daily weights were ordered for the patient due to her kidney dysfunction causing fluid excess. She was on vitals every 15 minutes including monitoring mean arterial pressure (MAP) for the first four hours, then every 30 minutes for the next eight hours, then taken per unit routine. Patient is on continuous cardiac monitoring since she is at risk for hypotension; she additionally is on continuous central venous pressure (CVP) monitoring. She is on 2 liters of oxygen via nasal cannula to promote optimal oxygen delivery. The physician ordered removal of all rings and constricting jewelry prior to fluid resuscitation due to risk of swelling. 7 COMPREHENSIVE CASE STUDY Medications The patient is currently on a multitude of scheduled medications, continuous and PRN medications for the treatment of her septic shock, acute kidney injury and UTI. There are a few medications, which are vital for proper treatment and prophylactic measures (See Appendix C for the rest of the patient’s medications). Enoxaprin (Lovenox) is a low-molecular weight heparin that is used as an anticoagulant. It is being used for this patient due to the increased risk for clotting. Septic shock causes microthrombi to form so this medication will decrease the chance of a VTE. The nursing implications include assessing for signs of bleeding and hemorrhage including nosebleeds, unusual bruising, black stools, hematuria among others. Patient responded well to the medication and did not report any side effects. Amoxicillin-clavulanate (Augmentin) is a broad-spectrum drug that is being used for the treatment of septic shock and her UTI. It will bind to the bacterial cell walls causing cell death. The nursing implications include monitoring bowel function. Diarrhea, abdominal cramping, fever, and bloody stools are signs of pseudomembranous colitis. Patient responded well to the medication and did not report any side effects. Piperacillin/tazobactam (Zosyn) is a broad-spectrum drug that is being used for the treatment of her UTI. This medication will also bind to bacterial cell wall membrane, causing cell death. The nursing implications include monitoring bowel function. Diarrhea, abdominal cramping, fever, and bloody stools could be a sign of pseudomembranous colitis. Assess for skin reactions including rash, fever, edema, mucosal erosions or ulcerations, and red or inflamed eyes. The patient responded well to the medication and did not report any side effects. 8 COMPREHENSIVE CASE STUDY Lactated Ringers is a mineral and electrolyte replacement therapy that is being used for fluid resuscitation. This medication will help improve the patient’s hypovolemic state caused by septic shock. The purpose is to increase her blood pressure and therefore improve tissue perfusion. The nursing implications include assessing for fluid balance (intake and output, daily weight, edema and lung sounds). The patient responded well to the medication as it was continuous and did not report any side effects. Diagnostic Tests Renal ultrasounds are used to “detect renal or perineal masses. This noninvasive procedure involves passing sound waves into body structures and recording images as they are reflected back,” (Lewis et al., 2014, p. 1059). The patient had suspected acute kidney injury and performing a renal ultrasound would allow a better look. Results showed hepatomegaly (enlargement of the liver), cholelithiasis (gallstones), and mild extrahepatic biliary ductal dilation. A MRI without CT is useful for “visualization of kidneys and the gallbladder. Computer generated images rely on radiofrequency waves and alteration in magnetic field,” (Lewis et al., 2014, p. 1059). The scan was used due to suspected presence of gallstones and the images would reveal as such. The results indeed showed gallbladder stones with no inflammation present. The third test is a urinalysis, which “confirms suspected urinary tract infection and identifies causative organisms,” (Lewis et al., 2014, p. 1057). The UTI can show the presence of bacteria in the urine, which will help with the diagnosis. The urinalysis revealed hazy urine with bacteria >10^5/mL, slight blood, but no glucose or ketones. The results of this test are significant because it indicates that the patient should be placed on an antibiotic and indicated that the UTI caused the septic shock (See Appendix B for information on all diagnostic tests). COMPREHENSIVE CASE STUDY 9 Nursing Diagnoses and Review of Literature The first nursing diagnosis for the patient is ineffective tissue perfusion related to systemic vasodilation secondary to septic shock as evidence by the patient’s hypotension. The goal is to increase tissue perfusion and the SMART outcome is that the patient will have a systolic blood pressure equal to or higher than 90 mmHg by the end of shift. The first intervention would be to administer oxygen to the patient due to the increased tissue oxygen requirements that septic shock places on the patient’s body. During septic shock, lactic acid levels increase due to the body transferring to using anaerobic metabolism. “Clearance of lactic acid levels following resuscitation is associated with survival emphasizing the importance in increasing systemic oxygen delivery in restoring tissue perfusion and enhancing outcome during septic shock,” (Tuchschmidt, Fried, Astiz, & Rackow, 1992, p. 219). The second intervention would be to examine the condition of the skin, mucosa and nails for inadequate tissue perfusion. The conditions of these are useful in determining whether cyanosis may be present. Checking for changes in color and temperature are simple yet effective for preventing further oxygen desaturation (Potter et al., 2013). The third intervention would be continuous monitoring of patient including blood pressure, oxygen saturation and electrocardiogram. The rationale is that these parameters are useful for the identification and treatment of septic shock. The research article by Giuliano and Kleinpell (2005) showed the importance of using continuous monitoring parameters for critically ill patients with sepsis. This descriptive study’s purpose was to gain an understanding of both physicians and critical care nurses’ preferences with regards to their use of monitoring parameters with septic patients. The participant’s survey ranked order from 1-4, the different parameters of physiologic monitoring including: continuous ECG, invasive blood pressure, pulmonary artery pressure and arterial oxygen saturation. These COMPREHENSIVE CASE STUDY 10 parameters were selected because they were “recommended by practice and professional standards, commonly available for standard critical care monitoring, used by critical care staff, and broadly reflective of the pathophysiologic changes that often occur early in the course of the septic disease process,” (Giuliano & Kleinpell, 2005, p.143). The results showed that out of the 617 professionals, “the majority of the respondents agreed that all four types of continuous physiologic monitoring, ECG (76.7%), invasive blood pressure (75.2%), pulmonary artery pressures (61%), and SpO2 (41.8%) are necessary in the care of patients with sepsis,” (Giuliano & Kleinpell, 2005, p.146). The implications of this study further proved the importance and value of these continuous physiologic parameters. This patient would benefit greatly from the use of monitoring due her critical condition. Monitoring can be considered a prophylactic measure because this would allow for nurses to be aware of her condition and notify the physician before her condition worsens. Finally, the outcome was met due to the goal being reached with a systolic pressure equal to or above 90mmHg by the end of the shift. The second nursing diagnosis for this patient is increased risk for infection r/t decreased immune system and increased WBCs. The goal is to prevent increased risk for infection and the SMART outcome is that the patient will have white blood cells within the 4.0-11.0 k/mm3 range by discharge. The first intervention will be to teach the patient signs and symptoms of infection. “Patients need to be able to recognize sources of infection and understand measures used to protect themselves” (Potter et al., 2013, p. 398). The rationale is that if the patient learns signs of infection including fever, erythema and inflammation then the patient will be able to notify the provider before the infection worsens. The second intervention is to encourage the patient to eat a well-balanced diet high in essential nutrients; provide dietary supplements if indicated. The COMPREHENSIVE CASE STUDY 11 rationale is that patients with poor nutritional status could be in a state of immune unresponsiveness and therefore are more susceptible to infection (Ackley & Lawdwig, 2013). The third intervention is to promote good hand washing by patient and staff. “A major component of patient and worker protection is hand hygiene. Contaminated hands of health care workers area primary source of infection transmission in health care settings,” (Potter et al., 2013, p. 410) The author Hughes (2006) looks at proper hand washing techniques to promote infection control in hospitals. Hand washing is considered to be one of the simplest yet most effective ways at preventing infection spread. Proper hand-hygiene involves using soap and rubbing them vigorously together for at least 15 seconds using soap. The friction of rubbing hands together removes soil and transient organisms from the hands. Including scrubbing underneath the fingernails is important because nails have shown to increase subungual bacteria, which will again put the patient at risk. The CDC estimates that every year in the United States 7% to 10% of patients contract a hospital-acquired infection resulting in approximately 80,000 deaths (Hughes, 2006). Health-care professionals and patients should abide by strict hand hygiene guidelines and ensure it as a priority for ultimately the safety of the patient and others. Finally, the outcome has not been met due to inability to assess because of the time frame allotted. The third nursing diagnosis is excess fluid volume related to kidney dysfunction as evidence by decreased urine output and increased weight gain. The general goal is to prevent furthering of excessive fluid volume and the SMART outcome is that the patient will not gain any more weight by the time of discharge. The first intervention is to monitor I/Os “measuring and recording all liquid intake and output during a 24-hour period is an important aspect of fluid COMPREHENSIVE CASE STUDY 12 balance assessment. If intake is substantially greater than output then the patient may be gaining excessive fluid,” (Potter et al., 2013, p. 898). This patient’s intake has been severely greater than her output, so monitoring I/O’s is important. The second intervention is daily weighing, “daily weights are an important indicator of fluid status. Each kilogram of weight gained or lost overnight is equal to 1 L of fluid retained or lost. These fluid gains or losses indicate changes in the amount of total body fluid. When weighing the patient she needs to wear the same clothes and compare the weight to that of the day before for comparison,” (Potter et al., 2013, p. 898 ). This patient in particular needs to be monitored due to her severe fluid retention. The third intervention is to perform lung auscultation since excessive fluid volume can occur in the lungs as well as other places in the body. Due to this patient’s decreased kidney functioning the fluid can travel to the lungs. Listening to lung sounds for crackles, monitoring respirations for effort will help. This patient in particular already has decreased tissue perfusion due to sepsis; monitoring lung sounds can prevent orthopnea (Ackley & Lawdwig, 2013). The article by Yerram, Karuparthi and Misra (2010) looks at preventing fluid overload in patients with acute kidney injury (AKI) by monitoring intake and output. AKI is thought to have occurred because of hypotension causing renal hypoperfusion, which leads to ischemia. The fluid resuscitation is extremely important in patients with septic shock due to the relative hypovolemia, but it is important to note that fluid overload is considered “almost inevitable” for patient with AKI. “To mitigate the development of fluid overload, and its adverse effects, a strategy of careful early guided fluid resuscitation to achieve hemodynamic stability, followed by careful reassessment of fluid status should be followed,” (Yerram, Karuparthi, & Misra, p. 352). Finally, the outcome has not been met due to inability to assess because of the time frame allotted. 13 COMPREHENSIVE CASE STUDY References Ackley, B. J. & Ladwig, G.B. (2014). Nursing diagnosis handbook: An evidence-based guide to planning care (10th ed.). St. Louis, MO: Mosby Elsevier. Giuliano, K., & Kleinpell, R. (2005). The sse of common continuous monitoring parameters. AACN Clinical Issues: Advanced Practice in Acute and Critical Care, 16(2), 140-148 Hughes, N. (2006). Health & safety: Handwashing. The American Journal of Nursing, 106(7), 96-96 McCance, K. L., & Huether, S. E. (2014). Understanding pathophysiology (7th ed.). St. Louis: Mosby Elsevier. Potter, P. A., Perry, A. G., Stockert, P. A., & Hall, A. M. (2013). Fundamentals of nursing (8th ed.). St. Louis, MO: Elsevier Mosby. Tuchschmidt, J., Fried, J., Astiz, M., & Rackow, E. (1992). Elevation of cardiac output and oxygen delivery improves outcome in septic shock. Chest, 102(1), 216-220. doi:10.1378/chest.102.1.216 Yerram, P., Karuparthi, P., & Misra, M. (2010). Fluid overload and acute kidney injury. Hemodialysis International, 14(4), 348-354. doi:10.1111/j.1542-4758.2010.00498.x Vallerand, A., & Sanoski, C. (2013). Davis's drug guide for nurses. Philadelphia: F. A. Davis Company. 14 COMPREHENSIVE CASE STUDY Appendix A: Laboratory Tests Lab Test WBC Neutrophils (ANC) Lymphocyte Monocytes Hemoglobin (Hgb) Hematocrit (Hct) Platelets Serum Na Serum K Serum Cl Serum CO2 BUN Creatinine Normal Value 4.0 11.0 k/mm3 35-80% 10-45% 3-15% 13.0 - 18.0 g/dL 41.0 - 54.0 % 130-450 K/uL 135 - 145 mmol/L 3.5 - 5.2 mmol/L 101 -111 mmol/L 14-32 mmol/L 7-20 mg/dL 0.6- 1.5 mg/dL Glucose 65-99 mg/dL Ca 8.7 - 10.5 mg/dL Mg GFR 1.8 - 2.5 mg/dL <60 Date performed and result 11/07 17.6 74.5 10.8 8.8 12.9 Pathophysiological explanation of each abnormal value Leukocytosis due to septic shock increases levels of WBC. Increased infection causes cascade of WBC’s. Within normal limits 135 Within normal limits Within normal limits Decreased hemoglobin due to septic shock or due to medication Decreased hemoglobin due to septic shock or due to medication DIC or thrombocytopenia occurs during sepsis shock due to release of platelet activating factor Within normal limits 3.2 Kidney dysfunction leads to hypokalemia 107 Within normal limits 19 Within normal limits 37.5 271 37 High levels indicate kidney injury and UTI 3.2 High levels indicate acute kidney injury 129 1.8 Evidence shows that septic shock induces hyperglycemic response. Increased glucose could also be due to food and/or medication Calcium is low due to improper functioning of the kidneys. The kidneys along with PTH regulate the levels. Within normal limits 16 Low levels indicate kidney injury 7.7 15 COMPREHENSIVE CASE STUDY Appendix B: Diagnostic Tests Name of Test MRI without contrast Date of Test 11/11/2014 Renal Ultrasound 11/09/2014 Chest X-Ray 11/11/2014 Urinalysis 11/07/2014 Purpose of Test To check for gallstones To check for renal dysfunction Evaluation for pneumonia To check for UTI Test Results Gallbladder stones with no inflammation -hepatomegaly -cholelithiasis -mild extrahepatic biliary ductal dilation Negative for pneumonia -hazy urine with bacteria >10^5/mL reveals patient is positive for UTI 16 COMPREHENSIVE CASE STUDY Appendix C: Medications Name Dose, Route, Due, Frequency Class/ Mechanism of Action Most Common or Serious Side Effects enoxaprin Lovenox .4mL subQ qday @0900 Anticoagula nt. MOA: antithrombin -dependent. Bleeding, hemorrhage, anemia heparin flush 3mL IV flush q12h @0900 & @2100 Anticoagula nt MOA: prevents the formation of blood clots. The flush prevents blockage in the central line Bleeding, hemorrhage Contraindicatio ns/ Major Interactions Increased risk of bleed with NSAIDs, penicillins, warfarin, ticlopidine, abcoximabid, dextran, thrombolytics, clopidogrel and drugs that affect platelet function and coagulation Acute Hemorrhage, Decreased Platelets due to the Medication Heparin, Decreased Blood Platelets Nursing Interventions Patient Teaching Assess hemorrhage and bleed S/S. monitor CBC, platelet ct, stools for occult blood. Protamine sulfate 1 mg per 1 mg of enoxaparin is antidote for overdose Assess for signs of bleeding and hemorrhage (bleeding gums; nosebleed; unusual bruising; black, tarry stools; hematuria. aPTT test prior to therapy. Protamine Sulfate is the antidote for overdose Monitor for bleeding, bruising and increased thrombosis Advise patient to report any symptoms of unusual bleeding or bruising to health care professional immediatel y. Instruct patient not to take medications containing aspirin or NSAIDs while on heparin 17 COMPREHENSIVE CASE STUDY piperacillin/ tazobactam Zosyn Antiinfective piperacillin: Binds to bacterial cell wall membrane, causing cell death tazobactam: Inhibits betalactamase, an enzyme that can destroy penicillins. confusion, dizziness, headache, insomnia, lethargy, diarrhea, constipation, N/V, bleeding, leukopenia, pseudomembranous colitis, rash May alter excretion of lithium. Probonecid may cause decreased renal excretion and increased blood levels. Monitor bowel function for cramping, diarrhea due to pseudomembranous colitis. Obtain specimens for culture and sensitivity prior to initiating therapy. amoxicillinclavulanate Augmentin 500mg125mg PO 1tab q12h @0900 @2100 Bactericidal MOA: binds to bacterial cell wall causing cell death. Resistance of betalactamase Pseudomembranous colitis, diarrhea, N/V, hepatic dysfunction, vaginal candidiasis, rash Hypersensitivity to penicillins or clavulanate. May increase effects of warfarin, May decrease effectiveness of oral contraception Monitor bowel function for cramping, diarrhea due to pseudomembranous colitis. Acetaminoph en PO 650mg= 2tabs q4h PRN Antipyretic MOA: Inhibits the synthesis of prostaglandi ns that may serve as Hepatotoxici ty (high doses), Rash, uticaria, neutropenia, StevensJohnson Concurrent use of NSAIDS may increase the risk of adverse renal effects. 2.25g IV Piggyback, q6h, 200mL/hr @0300, @0900, @1500, @2100 therapy. Caution patient to notify health care professional if fever and diarrhea occur, especially if stool contains blood, pus, or mucus. Instruct patient to notify health care professional immediatel y if diarrhea, abdominal cramping, fever, or bloody stools occur and not to treat with antidiarrhea ls without consulting health care professional s. Assess overall Advise health status patient to and alcohol avoid usage before alcohol (3 administering or more acetaminophen glasses per . Evaluate day 18 COMPREHENSIVE CASE STUDY mediators of pain and fever, primarily in the CNS Lactated Ringers Injection 1,000 mL IV infusion @60 ml/hr continuous Ondanestron (Zofran) 2mL IV push q6h PRN Mineral and electrolyte replacement syndrome Hypervolemi a Infusion site reactions, MOA: including hydration Infection at therapy the site of injection, extravasatio n and infusion site anesthesia Antiemetic Headaches, dizziness, MOA: drowsiness, blocks the fatigue, effects of weakness, serotonin at torsade de 5-HT3 pointes, receptor sites constipation, located in diarrhea, dry vagal nerve mouth terminals and the chemorecept or trigger zone in the CNS Patients with fluid retention or those who are hyponatremic. Use cautiously in patients prone to metabolic, acidbase or fluid/electrolyte imbalances Hypersensitivity, hepatic impairment patient, concurrent use of apomorphine, congenital long QT syndrome patients hepatic, hematologic, and renal function periodically during prolonged, high-dose therapy. Assess fluid balance (intake and output, daily weight, edema, lung sounds) throughout therapy increase the risk of liver damage) if taking more than an occasional 1-2 doses Monitor ECG in patients with hypokalemia, hypomagnesia, HF, bradarrhythmi as, assess for extrapyramidal effects, Advise patient to tell nurse about irregular heart beat, facial twitching if they occur Explain purpose of the infusion and the importance of proper fluid/ electrolyte balance COMPREHENSIVE CASE STUDY I have reviewed the Code of Academic Integrity and can attest that this document is consistent with the provisions of the code and represents my own original work. Signed: Georgina Crookes 19