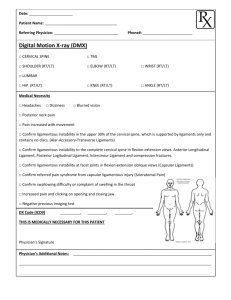
Cervical-Instability
advertisement

Cervical Instability Normal Anatomy • Normal stability of any joint is made of 2 aspects – Static Stabilisers – osseous configuration, capsules and ligaments – Dynamic Stabilisers- muscle function through dynamic ligament tension, force couples, joint compression and/or neuromuscular control • Approximately 50% of rotation occurs at C1/2 • Ligaments provide the primary source of stability • Vast amount of neurological and vascular structures Atlantoaxial Joint Transverse Ligament of the Atlas Atlantoaxial Joint Tectorial Membrane Atlantoaxial Joint Alar Ligament and Transverse Ligament Pathophysiology • Excessive movement at the upper cervical spine • Can be the result of bony fracture, ligamentous laxity or rupture or neuromuscular deficits • Can result in pain, neurological or vascular compromise Mechanism Of Injury • Traumatic – Whiplash – Fractures, Dislocations – Surgery • Systemic – Upper Respiratory Infection • Congenital – – – – – Down Syndrome RA Os Odontoideum Klippel-Feil Syndrome Hypermobility Syndrome Associated Pathologies • Cervical Artery Dysfunction • Cervical Myelopathy • Cervicogenic Headaches Subjective • History of trauma or congenital/systemic disease • Neck pain • Intolerance to prolonged positions • Feeling need to support the head • Sharp pain or catch with movements Subjective • Signs of neurological or vascular compromise – – – – – – – – – Drop attacks Facial or lip paraesthesia Bilateral or quadrilateral symptoms Nystagmus Dizziness Blurred vision Metallic taste in mouth Lump back of throat Think neuro, think vascular, think cranial nerves, think CNS Objective • Based on Subjective History • May not be appropriate in some cases • Start with cranial nerve and BP testing Objective Serious (Static Stability) • Reduced sensation • Reduced power • Reflex changes • Cranial Nerve Changes • Significant muscle spasm • Reluctance to move Non Serious (Neuromuscular) • Sensorimotor changes – Smooth Pursuit Neck Torsion – Saccadic Eye Testing – Joint Position Error • Full range of movement with painful stretching end of range • Painful catch/ unsmooth movements • Increased joint play Special Tests • Sharp Purser – Sitting relocation of C1 on C2 • Alar Ligament Testing – Supine testing of rotation and lateral flexion of Upper Cx with fixation of C2 • Transverse ligament Testing – Supine with fingers around patients head and between occiput and C2. Lift head and C1 anteriorly and hold for 20-30 mins Further Investigation • MRI • X-ray • Open Mouth X-Ray Management • Referral to a specialist if signs of neurological or vascular compromise • Conservative management for those with congenital or neuromuscular reasons for instability • Surgery nearly always for traumatic instability Conservative - Management • • • • Sensorimotor rehabilitation Cervical and scapular rehabilitation Manual Therapy to Thoracic Spine Acupuncture for pain relief Surgical - Management • Depends on pathology causing instability References • • • • • • • • • Lincoln (2000) Clinical Instability of the upper cervical spine. Manual Therapy Olson and Joder (2001) Diagnosis and Treatment of Cervical Spine Clinical Instability. JOSPT Niere and Torney (2004) Clinicans’ perception of minor cervical instability. Manual Therapy Cook et al (2005) Identifiers suggestive of clinical cervical spine instability: A Delphi study of physical therapists Mintken et al (2008) Upper cervical ligament testing in a patient with Os Odontoideum Presenting with Headaches. JOSPT Mathers et al (2011) Occult Hypermobility of the Craniocervical Junction: A Case Report and Review Osmotherly and Rivett (2011) Knowledge and use of craniovertebral instability testing by Australian physiotherapists Osmotherly et al (2012) The anterior shear and distraction tests for craniocervical instability. An evaluation using magnetic resonance imaging Rebbeck and Liebert (2014) Clinical management of cranio-vertebral instability after whiplash, when guidelines shoulder be adapted: A Case report


![[These nine clues] are noteworthy not so much because they foretell](http://s3.studylib.net/store/data/007474937_1-e53aa8c533cc905a5dc2eeb5aef2d7bb-300x300.png)


