Circulation Vivas
advertisement

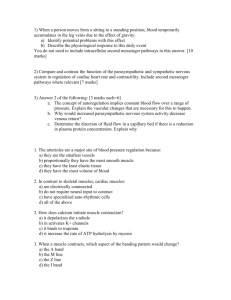
CIRCULATION VIVAS The Heart 2011-1 Describe the normal sequence of electrical excitation of the cardiac conduction system and cardiac muscle? (+ 2006-2) SA -> radially through atria -> AV node -> Bundle of His -> Major bundle branches (L) and (R) -> Purkinje fibers -> ventricular muscle: septum to apex, then up to AV grooves. Spread is from endocardial to epicardial surfaces What are the common mechanisms which cause abnormalities of cardiac conduction? And… What are the possible clinical consequences of these conduction abnormalities? 1. Abnormal pacemakers - ectopic beats - pacemaker failure (sick sinus syndrome) - fibrillation (atrial or ventricular) 2. Re-entry circuits - atrial flutter - other tachyarrythmias 3. Conduction defects - heart block - bundle branch blocks 4. Prolonged repolarisation - long QT (increased vulnerability to ventricular arrythmias/sudden death) 5. Accessory pathways - WPW (Bundle of Kent) and LGL (short PR) -> SVT 2010-2 Please draw a normal ECG tracing Describe the cardiac events that relate to each of the intervals Cardiac cycle: PR R to end of T End of T to P Phase 1 Phase 2 Atrial systole Isovolumetric vent. contraction Phase 3 Ventricular ejection Phase 4 Isovolumetric Vent. Contraction Ventricular filling Phase 5 Atrial systole Ventricluar systole Diastole The Action Potential: R wave S wave ST segment T wave T-P Phase 0 Phase 1 Phase 2 Phase 3 Phase 4 Rapid depolarization Rapid repolarization Plateau Slow repolarization RMP Na influx (fast) Na innactivation Ca influx (slow) K efflux Nil What is the electrophysiological basis for elevation acute MI? R ST wave Phase 0in(Na influx S wave Phase 1 Defect in infarcted cells Rapid repolarization Decreased resting membrane potential Delayed depolarization Cause Accelerated K+ opening Loss of intracellular K+ Current Flow Out of infarct ECG change ST elevation Timing Lasts minutes only Into infarct (diastole) TQ depression ( = ST elevation) ST elevation Minutes -> days Out of infarct After 30mins -> days 2009-2 Draw an ECG trace and identify the 5 phases of the cardiac contractile cycle. Also demonstrate the ventricular volume trace. Cardiac Cycle: 1. Atrial systole 2. Ventricular isovolumetric contraction 3. Ventricular ejection 4. Ventricular isovolumetric relaxation 5. Ventricular filling 2008-2, 2006-1 Please draw a normal ECG tracing, showing the durations of the major intervals Intervals PR 0.18 QRS 0.08 QT 0.4 ST 0.32 How does the ECG change with hyperkalaemia? 1. K+ 7.0: Tall peaked T waves 2. K+ 8.5: Loss of atrial activity, widened QRS 3. Extreme: Arrhythmias (VT and VF), then unexcitable (sinusoidal) How does it change with hypokalaemia? Long PR, ST depression, T inversion, U-wave 2007-2, 2005-2 Describe or draw an action potential in ventricular muscle What are the ion fluxes that produce this action potential How does the ECG relate to the ventricular muscle action potiential The Action Potential vs ECG: R wave S wave ST segment T wave T-P Phase 0 Phase 1 Phase 2 Phase 3 Phase 4 Rapid depolarization Rapid repolarization Plateau Slow repolarization RMP Na influx (fast) Na innactivation Ca influx (slow) K efflux Nil Why does tetany not occur in cardiac muscle 2005-2 - Because of the inactivation of the sodium channels and the prolonged action potential, cardiac muscle cannot contract in response to a second stimulus until near the end of the initial contraction - During phases 0 to 2 and about half of phase 3 (until the membrane potential reaches approximately –50 mV during repolarization), cardiac muscle cannot be excited again; that is, it is in its absolute refractory period - It remains relatively refractory until phase 4 - Therefore, tetanus of the type seen in skeletal muscle cannot occur - Of course, tetanization of cardiac muscle for any length of time would have lethal consequences, so it is a safety feature 2009-2, 2008-2, 2007-1, 2006-2, 2003-1 Describe the features of the action potential in cardiac pacemaker tissue - Rhythmically discharging cells with a membrane potential, that after each impulse declines to the firing level: the prepotential or pacemaker potential triggers the next impulse. 1. Prepotential: Initially IK efflux declines. Then Ih channels open (following hyperpolarization) “funny” channels that pass both K+ and Na+. Completed by Ca2+ influx via T (transient) channels 2. Action potential: due to Ca2+ influx via L (long-lasting) channels 3. Repolarization: due to K+ efflux – no plateau Describe the major differences between a cardiac myocyte AP and the pacemaker 1. Fast Na+ depolarizaton vs slower Ca2+ 2. Pacemaker has automaticity due to rising prepotential 3. Myocyte has a plateau phase 4. Lower resting potential 5. Faster conduction rate (1m/s vs 0.05) How do autonomic factors alter the slope of the prepotential? 2007-1, 2003-1 Sympathetic: - speeds Ih - NA -> via 1 receptors -> cAMP -> opens L channels -> increased ICa -> increases slope of prepotential -> increases rate Parasympathetic: - Vagal cholinergic stimulation -> ACh release -> M2 receptors via B subunit of G protein -> increased intracellular K+ -> slows Ih and cAMP -> hyperepolarization/decreased slope -> slows rate 2010-2, 2005-1, 2003-2, 2003-1 List in order, the mechanical phases of the cardiac cycle Please draw the pressure changes in the ventricle that occur during the cardiac cycle 1. Atrial systole 2. Ventricular isovolumetric contraction 3. Ventricular ejection 4. Ventricular isovolumetric relaxation 5. Ventricular filling 2009-1, 2005-1 Describe the pressure and volume changes at the onset of systole Describe the pressure and volume changes at the onset of diastole At the start of systole: - Mitral and tricuspid valves close (first heart sound) - Ventricles start to contract - AV valves bulge into atria (jugular c wave) - Isovolumetric contraction lasts 0.05s - Until (L) > 80mmHg, (R) >10mmHg - Then aortic and pulmonary valves open At the start of diastole - Ventricles relax - Aortic and pulmonary valves close when momentum of ejected blood overcome by arterial pressure -> vibrations are second heart sound - Initially no change in volume: hence isovolumetric relaxation - AV valves open when pressure falls below atrial pressures Relate the aortic pressure to the phases of the cardiac cycle 2005-1 When do the heart sounds occur? 2003-2 2007-2 Draw and label a diagram of the jugular venous pressure wave How does the ECG relate to the jugular venous pressure Explain the origins of the fluctuations of this wave - a wave: atrial systole - some of the blood regurgitate back into the great veins - c wave: ventricular isovolumetric contraction tricuspid wave bulging - x descent: ventricular ejection - atrial volume increase as tricuspid pulled distally - v wave: isovolumetric relaxation - rise in atrial pressure prior to tricuspid valve opening - y descent: ventricular filling - atrium empty when tricuspid opens 2011-1, 2010-2, 2008-1, 2003-2 (+ contractility) What are the parameters that define cardiac output? CO = SV x HR What are the factors that influence stroke volume? 1. Preload (= EDV or cardiac fiber length) 2. Afterload 3. Contractility What is cardiac preload? Amount of blood in ventricles at the end of diastole = end diastolic volume (Usually 130ml). Also the amount of stretch of cardiac muscles c.f. resting length. What factors affect preload? - Blood volume - Venous return e.g. increased by blood volume, venous constriction, muscle pump, negative intrathoracic pressure, venous compression (uterus in pregnancy) - Increased intrapericardial pressure, e.g. tamponade from pneumothorax, pericardial effusion/hemorrhage, tumour, infection, IPPV - Atrial contraction - Decreased ventricular compliance, e.g. MI, infiltrates How can cardiac output be measured? 1. Direct Fick method: amount of substance taken up/time = A-V difference x blood flow, so… Cardiac Output = Amount of substance consumed (ml/min) Aterial - Venous - commonly O2 is used: consumption measured by spirometry, and A-V difference across the lungs from arterial vs pulmonary venous sample via catheter 2. Indicator dilution method: output of heart = amount of indicator divided by the average concentration after a single circulation. Thermodilution with cold saline is a safe technique. 2011-2, 2009-1, 2008-1, 2006-2 What factors influence myocardial oxygen consumption? 1. Intramyocardial tension which is dependant on: a) Pressure - after load, systolic pressure, contractility b) Radius - preload (nb tension is proportional to radius as per law of Laplace) c) Wall thickness 2. Contractile state of the heart i.e. ionotropy As per Frank-Starling curve: 3. Heart rate i.e chronotropy 4. Also: - cardiac work = SV x MAP of aorta for (L) and pulmonary a. for (R), note 7x more stroke work for (L) ventricle b/c aorta MAP = 80mmHg c.f. pulmonary MAP 10mmHg) - Pressure load increases O2 consumption more than volume load How does decreasing a patient’s heart rate improve symptoms of angina? 1. Decreasing HR decreases O2 demands 2. Lower HR = longer diastole, thus at a slower heart rate there is more time for coronary circulation which occurs in diastole What effect does preload and afterload have 2009-1 - Both increase work. Cardiac work = SV x MAP - Also, both increase intramyocardial tension Preload: Law of Laplace: radius proportional to wall tension Afterload: Increase in pressure increases tension - As per Frank-Starling law and curve, increased preload (EDV) increases SV = more work - Pressure load increases O2 consumption more than volume load, thus AS causes more angina than AR. Reason not well understood - Because afterload aorta > pulmonary (aorta MAP = 80mmHg c.f. pulmonary MAP 10mmHg), note 7x more stroke work for (L) ventricle c.f. (R) What are the changes in cardiac function with exercise and how these mediated? 2006-2 1. Rate and stroke volume 2. Adrenaline and sympathetic discharge 3. Venous return What are the physical laws involved? 1. Starling 2. Laplace Law: P = 2T/R 2011-1, 2010-2, 2009-2, 2006-1 Please draw the starling curve What factors influence myocardial contractility? Positively Inotropic: - Sympathetic stimulation via nerves or circulating catecholamines - Drugs such as xanthines, glucagon, cardiac glycosides, adrenergic agents - Post-extrasystolic potentiation - Increased heart rate (small effect) - Increased myocardial mass (chronic) Negatively Inotropic: - Metabolic abnormalities: hypoxia, acidaemia, hypercarbia - Reduced sympathetic tone - Blockade of circulating catecholamines - Pharamcologic depression (Ca blockers, antiarrhythmics) - Myocardial disease - Increased parasympathetic tone - Reduced intracellular calcium - Hypothermia - Heart failure (intrinsic depression) Frank-Starling Law aka Starlings law of the heart: “energy of contraction is proportional to the initial length of the muscle fibres” i.e. length of fibres (preload) is proportional to the end diastolic volume The Frank-Starling curve demonstrates the relationship between SV and EDV How do changes in myocardial contractility alter the relationship between end diastolic volume and stroke volume? 2011-1 Frank-Starling Curve: - Increasing contractility moves the curve upwards and to the left - Decreasing contractility moves the curve downwards and to the right - More contractility = more is ejected by ventricles giving lower EDV and more SV 2011-2, 2010-1, 2006-1 Describe the factors that control blood flow to the myocardium At rest heart extracts 70-80% of O2. More O2 consumption requires more blood. a) Chemical factors -> vasodilation: Local factors control radius of blood vessels (overall flow and regional flow). Low O2 is the main controlling factor. Hypoxia increases concentrations of CO2, H+, K+ lactate, prostaglandins, adenine nucleotides, and adenosine. b) Neurogenic factors -> controlling radius of blood vessels (overall flow and regional flow) Parasympathetic nerves: vagal stimulation dilates coronaries Sympathetic nerves: α -> vasoconstriction, β -> vasodilatation. However giving NA -> increased HR/contractility via β -> increased O2 demand -> vasodilation. Giving β-blocker and NA -> vasocontriction via α only. So coronary flow is preserved if systemic blood pressure falls -> NA release c) Pressure gradients - Flow is dependant gradient between arteries and veins: thus reduced in CHF where systemic venous pressure is high - During systole ventricular muscle pressure limits flow, especially to subendocardium of the left ventricle: in AS both high pressure and high O2 requirement -> high risk for myocardial ischaemia d) Viscosity of the blood 2007-2 Describe the factors controlling blood flow through skeletal muscle during exercise - Mainly local regulation - Mainly via low O2 -> arterioles and precapillary sphincters open because smooth muscle cannot maintain contraction in hypoxic conditions - Local metabolites: low PO2, high PCO2, increased K+, adenosine, lactic acid - Temperature rise -> vasodilation What other circulatory changes occur in the body during exercise and why - Increased cardiac output via sympathetic stimulation (increased rate and contractility) - Sympathetic vasocontrictor nerves/adrenaline -> contraction of peripheral aterioles not in skeletal muscle (coronary and cerebral systems spared) - Depends if exercise is isometric (length doesn’t change) vs isotonic (force doesn’t change) Isometric: Psychic stimuli act on medulla oblongata -> decreased vagal tone (and cardiac sympathetic stimulation) -> increased heart rate Stoke volume unchanged Blood flow to muscle limited by steady muscle contraction -> compression of vessels Systolic and diastolic blood pressure rises (in seconds) Isotonic: Similar prompt increase in heart rate Also increase in stroke volume Vasodilation in exercising muscles Thus diastolic BP the same or lower, and systolic only rises a small amount - Increase venous return due to muscle pump and thoracic pump - Also increased return because venoconstriction of capacitance vessels The Circulation 2011-2, 2009-1, 2008-1, 2006-2, 2005-2 What factors determine cerebral blood flow? 1. Intracranial pressure 2. Local constriction and dilation of cerebral arterioles 3. Mean arterial pressure at brain level 4. Viscosity of blood 5. Mean venous pressure at brain level - Monro-Kellie doctrine - Cushing reflex - Local autoregulation What is the Monro-Kellie Doctrine? Volume of blood (75ml), CSF (75ml) and brain (1400g) in the cranium at any time remains relatively constant (within a rigid structure). What substances are important for brain metabolism 2008-1 1. Oxygen ~49ml/min = 20% body O2 consumption 2. Glucose (major energy source) ~77mg/min 3. Glutamate (converted to glutamine as detox mech NH3 i.e. ammonia) ~5.6mg/min What is Cushing’s Reflex? 2006-2 Physiologic nervous response to raised ICP resulting in triad of widening pulse pressure, irregular breathing and reduction of the heart rate. Increased ICP > 33mmHg -> ↓ CBF -> ischaemia of RVML - ↑ systemic BP and heart rate (first stage) –> stimulation of baroreceptors –> stimulation of vagal outflow –> bradycardia (second stage) 2010-1, 2009-1, 2003-2 Describe how tissues regulate their own blood flow - 2 theories to autoregulation Myogenic: Intrinsic contractile response of smooth muscle to stretch, so as blood pressure rises the vessels walls are stretched and the vascular smooth muscle contracts. A greater degree of contraction is seen at higher pressures. Respond to tension, so as per Law of Laplace the tension is proportional to the radius (x distending pressure). To maintain a given wall tension at higher pressure requires a reduction in the radius. Metabolic: Products of metabolism are potent vasodilators and thus with reduced blood flow and increased metabolism more accumulate. With increased blood flow more are washed away. Vasodilators include: hypoxia, hypercapnea, acidosis, lactate, K+, temperature, histamine, adenosine Describe how blood flow can vary in different parts of the brain 2005-2 - PET and fMRI show that there is marked variation in local blood flow with brain activity - Active neurons attract blood flow - Neurovascular coupling may adjust local perfusion in response to changes to brain activity - Certain diseases show reduction in flow to affected areas (Alzheimers, Huntington, Manic depressives, schizophrenia) 2004-2, 2003-2 Describe how blood flow is regulated at the level of the endothelium Vasodilators: 1. Prostacyclin - Endothelium derived from arachidonic acid via cyclooxegenase - Inhibits platelet aggregation and vasodilates 2. Nitric oxide (EDRF) - synthesized from arginine by NOS - activated by agents that increase intracellular Ca2+ like bradykinin and acetylcholine - activates guanylyl cyclase producing cGMP -> smooth muscle relaxation - inactivated by haemoglobin 3. Carbon monoxide and H2S (hydrogen sulpide) 4. Kinins Vasoconstrictors: 1. Thromboxane A2 - Platelet derived from arachidonic acid via cyclooxegenase - Promotes platelet aggregation and vasoconstrics 2. Endothelin-1 - potent vasoconstricor - resembles venom of Israeli burrowing asp 3. Serotonin What other general effects do endothelins have on the cardiovascular system - Positive inotrope and chronotrope - Rise in ANP/renin/aldosterone - Decreased GFR and renal blood flow 2010-1 Draw a diagram of the changes in systolic and diastolic pressure as blood flows through the systemic circulation How does the total cross sectional area of the vessels change through the systemic circulation 2007-1, 2003-2 What is the normal value for venous return in the healthy human adult? 5 - 5.5 L/min What are the major factors that influence venous return to the heart? Right atrial pressure aka CVP 1. Circulating blood volume 2. Sympathetic and parasympathetic tone (venous capacitance) 3. Muscle pump 4. Thoracic pump (expiration creates higher negative pressure in thorax (from -2.5 to -6mmHg) and also diaphragm creates some increased pressure in abdomen) 5. Effect of the heart pump (ventricular systole pulls tricuspid valve distally) 6. Gravity What is the relationship between right atrial pressure and venous return? - venous return is determined by a pressure gradient (venous pressure – RAP) and venous resistance circulation is a closed system so cardiac output matches venous return (when averaged over time) achieves balance through Frank-Starling mechanism: if venous return is increased on lying down, preload and SV increase leading to an increase in cardiac output RAP = 4.6mmHg average, with range 2mmHg in inspiration to 6mmHg in expiration (Ganong) 2008-2, 2006-2, 2004-2 Where are Baroreceptors found in the body? 1. Stretch receptors in adventitia of vessel walls, major ones found in carotid sinus (ICA, rise or fall) and aortic arch (apex, rise) to monitor arterial side of circulation. 2. Also low-pressure "cardiopulmonary receptors" in right and left atria, and pulmonary circulation to monitor venous circulation What is the effect of vessel wall distension on a baroreceptor? - Stretch of vessel wall leads to increased baroreceptor discharge - More sensitive to pulsatile pressure than constant pressure - Transmitted by afferents in glossopharyngeal (carotid sinus nerve) and vagus (aortic depressor nerve) nerves to medulla/vasomotor area - NTS -> glutamate to CVLM -> GABA to RVLM: inhibits sympathetic vasoconstriction - NTS -> dorsal motor nucleus and nucleus ambiguous: parasympathetic/vagus stimulation Net effect is: 1. Inhibition of tonic discharge of sympathetic vasoconstrictor nerves 2. Excitation of cardiac vagal innervation -> Results in vasodilation, with decrease in BP, HR and CO. What is the effect of chronic hypertension on the activity of the arterial baroreceptors 2006-2 They ‘reset’ to maintain normal basal activity at the elevated blood pressure (reversible, unknown mechanism) What is the Set Point? 2004-2 - Neutral MAP for vasomotor centre, around 100 mm Hg 2007-1, 2003-2 What are the major factors affecting the regulation of arterial pressure? 1. Baroreceptor reflex rapid, adjusts for changes in posture aortic arch and carotid sinus messages via IX and X -> medulla (RVLM) autonomic nervous system to adjust HR/contractility (vagal) and peripheral vascular resistance (sympathetic) 2. Renin-angiotensin system longer term adjustment of blood pressure compensation of volume loss or BP drop via vasoconstrictor angiotensin II 3. Aldosterone release steroid hormone released from the adrenal cortex in response to ATII or high potassium stimulates sodium retention and potassium excretion by kidneys sodium is main ion determining amount of fluid in vessels via osmosis, thus increases fluid retention and indirectly BP 4. Caridiopulmonary and atrial stretch receptors feedback by regulating the secretion of ADH (vasopressin), rennin and aldosterone increase blood volume which increases cardiac output (by Frank-Starling law) 5. Peripheral chemoreceptor reflex In carotid and aortic bodies decreased flow in hypotension stimulates them 2005-1 Describe the cardiovascular compensations to acute blood loss. Tachycardia; Vasoconstriction; Venoconstriction. Describe the other physiologic compensations to acute blood loss. - Tachypnoea and Increased: - Adrenaline/noradrenaline (sympathetic) - Vasopressin - Glucocorticoids - Renin/angiotensin/aldosterone - Erythropoietin - Plasma protein synthesis 2008-1 What are the basic factors which determine the rate of flow of blood through a blood vessel? Flow = Pressure/Resistance Poiseulle-Hagen formula Where: = viscosity L = length of tube r = radius What factors cause turbulent flow in a blood vessel? Loss of laminar flow, the probability of this can be expressed by Reynold’s number Where: ρ is the fluid density D is the diameter of the tube is the velocity of flow viscosity of the fluid V η is the The higher the value of Reynold’s number the greater the probability of turbulence, which usually occurs when Reynold’s number is between 2000-3000. 2005-2 What factors cause turbulence in blood flow - “critical velocity”, density/viscosity, diameter Reynolds number gives probabilty Why is blood flow slower in capillaries - highest total cross sectional area (4,500 cm2, i.e. 1000x that of the aorta) - velocity = flow/area What is the relationship between pressure and wall tension in blood vessels of different sizes - As per Law of Laplace, P = T/r - Smaller vessels have less tension to balance the pressure What is the relationship between pressure and wall tension in the heart - ventricular dilation means more tension required to generate the same pressure = more work