Digestive System Powerpoint
advertisement
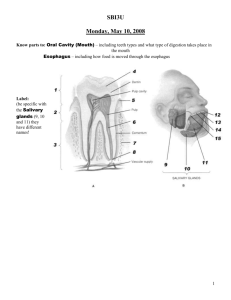
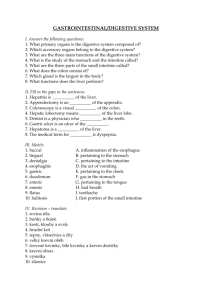
Digestive System Organization of the Digestive System The organs of the digestive system are divided into TWO main groups: The alimentary canal – also called the gastrointestinal (GI) tract Accessory organs – teeth, tongue, salivary glands, liver, gallbladder, pancreas Gastrointestinal (GI) Tract A long, winding, continuous tube that extends from the mouth to the anus Averages about 9 meters (30 feet) Consists of: Oral cavity, pharynx, esophagus, stomach, small intestine, large intestine, rectum, anal canal Accessory Organs Located either within the alimentary canal or outside it Communicates by way of ducts Assist the organs of the alimentary canal in their functions Includes: teeth, tongue, salivary glands, liver, gallbladder, pancreas Digestive Processes Food needs to be turned into a form usable by cells This needs to be done by: Mechanically reducing the food Chemically reducing the food Absorbing the food into the blood through the intestinal wall Carried by blood to the body’s cells Digestive Processes Ingestion Taking food into the mouth (mechanical) Mastication Chewing (mechanical) Salivary action (chemical) Deglutition Swallowing (mechanical) Peristalsis Wavelike contractions that move food through the GI tract (mechanical) Absorption Passage of food molecules from GI tract into circulatory system (mechanical & chemical) Defecation Elimination of undigestible wastes (mechanical) SPECIAL FEATURES OF THE DIGESTIVE SYSTEM Peritoneum: serous membrane, lubricating tissue (pericardium of the heart, pleurae of lungs) Parietal Peritoneum: lines the wall of the abdominal cavity Visceral Peritoneum: covers the abdominal organs Extensions of the Parietal Peritoneum Falciform ligament – attaches liver to diaphragm & anterior body wall Lesser omentum – extends between liver and the lesser curvature of the stomach Greater omentum – extends from greater curvature of stomach to transverse colon Mesentery – supports the intestine Mesocolon – supports large intestine Wall Structure of the Alimentary Canal Mucosa Mucous membrane that lines the lumen of the alimentary canal Consists of a thin layer of loose connective tissue & a small amount of smooth muscle in the external layer Major functions: protection from invading microorganisms, absorption of digested food materials, & secretion of mucous and digestive enzymes Submucosa External to the mucosa Composed of loose connective tissue, rich in blood vessels, lymphatic vessels, nerve endings, & small glands Wall Structure of the Alimentary Canal Muscularis Smooth muscle that externally encircles the submucosa Thickened at certain points along the alimentary canal to form sphincters, which act as muscular valves Provides the mixing of food during mechanical digestion as well as the propulsion of food through the alimentary canal by PERISTALSIS Serosa The visceral peritoneum DIGESTIVE ORGANS Mouth Function: process of chewing (mastication) Moistening of food with saliva begins process of chemical digestion Accessory organs associated with mouth: tongue, teeth, salivary glands Space between tongue and palate is called oral cavity Cheeks and lips are separated by a space called the vestibule Palate: forms the roof of the oral cavity Hard palate: hard, bony anterior part of oral cavity Soft palate: muscular, posterior part, forms archway bordering pharynx Palatine tonsils: along both sides of the archway Uvula: extends from the archway in a downward projection Tongue Anchored to the floor of the mouth by a membranous fold extending from its midline along its undersurface, called the lingual frenulum Contains papillae which contain taste buds and also help to provide friction for moving food Teeth Provide mastication Dentition: two different sets of teeth during normal development First set: appear at about 6 months, continue to erupt until all 20 teeth are present by about 24 months Referred to as deciduous teeth Second set: appear between 6 and 12 years By the end of adolescence, all permanent teeth have erupted except for the third molars, or wisdom teeth (17 and 25 years) Teeth In a full set, there are 32 permanent teeth Types: Incisors – pointed chisel (cutting) Canines – cone-shaped (serve as tearing tool) Premolars & Molars (bicuspids) – broad, flattened surfaces (grinding) Tooth Structure Crown: visible part of tooth above the gum line Root: buried below the gum line Enamel: covers the crown – hardest substance in the body Salivary Glands Collection of accessory organs surrounding the mouth that secrete a fluid called saliva Saliva consists of 99.5% water and 0.5% solutes Medium for dissolving soluble food molecules Solutes include mucus and enzymes Lysozyme destroys bacteria Salivary amylase begins chemical digestion of starchy foods Parotid Glands Largest salivary glands Located in front of and slightly below each ear between the skin of the cheek and the masseter muscle Secretes a clear, watery fluid that is rich in salivary amylase Submandibular Glands Located along the inner surface of the jaw in the floor of the mouth Secrete a more viscous fluid than parotids due to the mucus in their secretions Sublingual Gland Lies under the tongue Secrete a thick and stringy fluid due to the abundance of mucus Digestion in the Mouth: Digestion begins here Mastication – chewing and mixing of food with saliva Creates a BOLUS Pharynx Chamber located behind the oral cavity extending from the internal nares to the larynx Its walls are composed of skeletal muscle lined with mucus membrane Divided into 3 segments: nasopharynx, oropharynx, and laryngopharynx Function: transports food from mouth to esophagus Plays an important role in the act of swallowing Act of Swallowing: Begins as food bolus is pushed from the mouth into the pharynx by the tongue Soft palate and uvula rise to keep food from entering the nasal cavity Followed by contraction of muscles in the wall of the pharynx, which moves the larynx upward as the epiglottis presses downward (closes off trachea) Muscles in lower pharynx relax, opening the passage into the esophagus The food bolus is pushed into the esophagus and onward to the stomach by peristalsis, which begins in the pharynx and continues along the length of the esophagus Esophagus Muscular tube that extends from the pharynx to the stomach for about 25 cm (10 inches) Located behind the trachea in the neck and upper thorax Collapsed when it is not propelling food to the stomach Forms a sphincter (lower esophageal sphincter/ cardiac sphincter) near its union with the stomach Acts as a valve to prevent upward movement of material from the stomach Opens as peristaltic waves reach the stomach Stomach Pouch-like organ that is about 25 cm (10 inches) long and in most people can hold over 2 liters of food When empty, its inner linings form deep folds known as rugae (ROO-JE) The convex lateral margin of the stomach is called the greater curvature The greater omentum extends from the greater curvature The concave medial margin is known as the lesser curvature The lesser omentum extends from the lesser curvature Parts of the stomach Cardia – small area surrounding the opening that receives food from the esophagus Fundus – expanded region that bulges above the cardia; serves as a temporary holding area for food Body – main part of the stomach; lies between the fundus and the pylorus Pylorus – narrowed, inferior region At the terminal end is the pyloric sphincter Serves as a valve to control the movement of food from the stomach to the small intestine Stomach Wall – MUCOSA Characterized by millions of tiny openings that can be seen only with a magnifying lens or microscope called gastric pits Gastric pits lead into tube-like gastric glands that secrete a collection of chemicals called gastric juice 2-3 liters of gastric juice pour out from these glands each day Glands contain secratory cells called zymogenic (chief) cells, which secrete digestive enzymes Parietal cells secrete hydrochloric acid (HCl) and intrinsic factor Mucous cells secrete mucus Ulcers will develop if this lining breaks down Functions of the Stomach: 1. Mechanical Digestion – accomplished by mixing and churning actions 2. Chemical Digestion – provided by gastric juice Several enzymes are present, but most importantly, pepsin is present – secreted by zymogenic cells in an inactive form called pepsinogen Pepsin is a powerful protein-splitting enzyme capable of beginning the breakdown of nearly all proteins Pepsin and its acidic environment are kept from digesting the stomach wall by the protective layer of mucus that coats the mucosa 3. Absorption Limited amount of absorption takes place across the stomach lining Materials the can cross this barrier are: small amounts of water, certain salts, glucose, alcohol, aspirin, and some lipid-soluble drugs 4. Propulsion Propulsion Provided by peristalsis The material that is ready to enter the small intestine has been converted by mechanical and chemical digestion into a semi-fluid paste of small food particles and gastric juice known as chyme Additional role of the stomach: Secretes a substance called intrinsic factor, which aids in absorption of vitamin B12 by the small intestine (vital for survival due to its role in the production of mature red blood cells Pancreas An accessory organ of the digestive system and has an endocrine function Soft, oblong organ that lies behind the stomach in the upper abdominal cavity Extends across the abdomen from its head near the duodenum to its tail, which touches the spleen – middle portion is the body Within the pancreas are groups of exocrine secretory cells called acini The secretory cells release a mixture of enzymes known as pancreatic juice into the duct The ducts from all the acini drain into the pancreatic duct, which fuses with the common bile duct before entering the small intestine Scattered among the acini are clusters of endocrine cells called the islets of Langerhans, which contain the cells that produce the hormones insulin and glucagon and release them right into the blood Functions of the pancreas Digestive function of the pancreas is the secretion of pancreatic juice, which finds its way into the duodenum of the small intestine In an average adult, about 1500mL of this watery, clear fluid is produced daily The pancreatic enzyme responsible for digesting carbs is known as pancreatic amylase The enzyme that aids in the digestion of fats is called pancreatic lipase The enzymes that digest nucleic acids are called nucleases Liver Largest visceral organ of the body Occupies the upper right side of the abdominal cavity and presses against the diaphragm Like the pancreas, the liver is associated with the small intestine by way of the common bile duct One of its primary functions is the production of bile that is necessary in fat digestion and absorption Structure of the Liver Divided into two main sections, called lobes The large right lobe and the smaller left lobe The falciform ligament, a fold of the peritoneum, separates the right and left lobes and suspends the liver from the diaphragm and anterior abdominal wall Each lobe is further divided into numerous liver lobules Liver cells, which are known as hepatocytes, are arranged within each liver lobule into columns that converge toward a central vein Columns are separated from adjacent columns by channels lined with endothelial cells These channels are filled with flowing blood and are called sinusoids Kupffer cells remove bacteria arriving with blood from the digestive tract Bile canaliculi carry a fluid secreted by hepatocytes known as bile Bile is a yellowish-green fluid that contains water, bile salts, bile pigments, cholesterol, and electrolytes Functions of the Liver Digestive role of the liver is the secretion of bile Emulsification – breaking apart clumps of fat molecules into tiny droplets HDL (high density lipoproteins) – good lipoproteins LDL (low density lipoproteins) – not good, can cause health problems Gallbladder The gallbladder is a small, thin-walled sac that serves as an accessory organ associated with the liver It is located immediately behind the liver, where it lies in a shallow depression tucked in against the lower margin of the right lobe The main function of the gallbladder is to store and concentrate bile secreted by the liver Small Intestine Body’s most important digestive organ It completes the processes of mechanical and chemical digestion, and is the main site of nutrient absorption Longest segment of the alimentary canal Extends from the stomach to the large intestine for about 6 m (20 feet) It is 2.5cm (1 inch) in diameter Suspended in the abdominal cavity by the mesentery, which anchors it to the abdominal wall It is framed by the large intestine Has three segments: duodenum, jejunum, and ileum Segments of the Small Intestine Duodenum Receives chyme from the stomach through the pyloric sphincter Only about 25cm (10 inches) long and is relatively immovable At the distal end of the duodenum, the small intestine continues as the more mobile jejunum Jejunum Extends for about 2.5m (8 feet) to the third segment, the ileum Ileum Longest segment at about 3.6m (12 feet) It unites with the large intestine at the ileocecal valve, which helps regulate the flow of material from the ileum to the large intestine Small Intestine Wall Mucosa Extremely specialized for the absorption of nutrients Has tiny projections known as intestinal villi Villi project about 1mm into the lumen of the small intestine where they come in contact with its contents Covering each villus is the mucosa, whose cells are bristled with thousands of tiny microprojections called microvilli Within each villus are capillaries and a lymphatic vessel (called a lacteal), which carry absorbed nutrients away with blood Submucosa Contains numerous lymphatic nodules, known as Peyer’s patches, which protect the body against infectious microorganisms that try to penetrate the intestinal wall Also contains a collection of mucous glands, called Brunner’s glands, found only in the duodenum – help neutralize acidic chyme from stomach Functions of the Small Intestine Chemical Digestion Completes chemical digestion by using a mixture of enzymes and bile Receives a wide spectrum of pancreatic enzymes from the pancreas and bile from the liver by way of the common bile duct Breaks down a wide spectrum of food (maltase, lactase, sucrase, and dextrase – all digest monosaccharides, which are carbs) Absorption Small intestine is the main site of nutrient absorption Effectiveness is due to the vast surface area of its mucosa (villi) Carb digestion begins in the mouth and ends in the small intestine Protein digestion by pepsin in the stomach and later in the small intestine by enzymes from the pancreas and intestinal mucosa results in the availability of amino acids Fat digestion occurs by the action of bile salts and enzymes within the small intestine Propulsion The propulsion of chyme through the small intestine is done by peristalsis Slow propulsion that takes between 3 and 10 hours to move chyme all the way through Large quantities of water and electrolytes are also absorbed by the villi Out of 3 liters of water, only 1 passes through to the large intestine If infection occurs, peristaltic contractions may dramatically increase, causing a very rapid movement of material through it, resulting in diarrhea Large Intestine Extends about 1.5m (5 feet) from its union with the small intestine at the ileocecal valve to the anus Its large diameter, which measures about 7cm (almost 3 inches), provides it with its name The main functions of the large intestine are to dry out indigestible material by absorbing water, and to eliminate this waste Structure of the Large Intestine Divided into 4 main segments Cecum: receives material from small intestine Attached to the cecum is the appendix Colon: ascending, transverse, descending, sigmoid Rectum: located against the sacrum in the pelvic cavity; extends downward as a straight tube until it converges with the last segment of the large intestine, the anal canal Anal canal Wall of the Large Intestine Its mucosa lacks the villi that are found in the small intestine In the mucosal lining are enormous numbers of mucus-secreting cells to allow for easy passage of fecal matter Muscular structure is called taenia coli The propulsion of feces through the large intestine and out through the anus is called defecation It normally takes 18 – 24 hours for material to pass through the 1.5m of the colon, whereas it takes only 3 – 10 hours to pass through the 6m of the small intestine