lipid digestion & absorption
advertisement

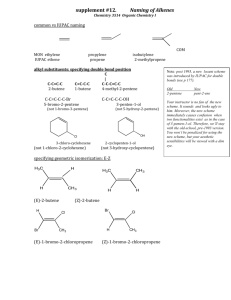
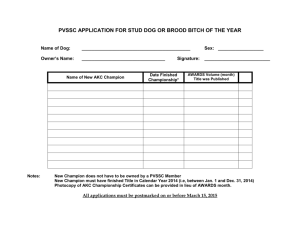
Lipids – Part 2 McCafferty LIPID DIGESTION & ABSORPTION Absorbable forms: Remember “hydrolysis?” Mouth Mechanical: chewing, mixed w/saliva for lubrication Chemical: Stomach Mechanical: peristalsis/churning ____________ Chemical: For digestion to continue, these fat droplets must be emulsified Small Intestine Fat droplets enter small intestine gallbladder contracts and releases __________ synthesized in the ______, stored in the __________ made from _________ Once fat is emulsified into the liquid, enzymes can work: Pancreas releases: pancreatic lipase TG _________________________________ (DRAW BELOW:) Lipid Absorption Small lipid fragments: Glycerol and Short Chain FAs (SCFAs) Absorbed directly into the bloodstream Portal vein to liver Lipid Absorption Big lipid fragments Monoglycerides and LCFAs need help! If absorbed into the blood: They need to be emulsified. Big lipid fragments, cont. Enter intestinal cell, re-form TG TG is incorporated into Lipoprotein carriers: Chylomicrons (CM) Lipoprotein = lipid associated w/proteins “Shuttle” Protein and phospholipid act as emulsifiers for the other lipids Lymph vessel The tissues can extract what they need from the CMs. CM remnants Lipoproteins -- Overview Lipids bound to protein Spherical structure – “Shuttle” Classes of Lipoproteins What is denser, lipid or protein? CM chylomicron – made in intestinal cells Transports ________TG from ________ to tissues eg. adipose and muscle VLDL – very low density lipoprotein made in liver Carries TG to tissues LDL – Made in liver Carries HDL – Made in liver & intestine Associated w/ risk for CVD Recommended Levels Total cholesterol For 30 yrs For 30 yrs (for kids 170 mg/dl) LDL cholesterol HDL cholesterol Triglycerides (TG) *note controversy surrounding these numbers LDL to HDL ratio Men: Women: LDL cholesterol increases with HDL cholesterol increases with STORAGE & USE OF FAT Overview: TG is main form of stored E in the body Adipose – When body needs fuel Storing Fat TG in blood (in CMs and VLDL) (need to get TG into adipose & muscle cells) INSULIN present Activates enzyme on blood vessel wall: LPL Lipoprotein Lipase LPL binds w/CM or VLDL and extracts TG Breaks down TG glycerol & 3FAs enter cell Storing Fat In adipose, TG fat droplets Storing Fat In adipose, TG Adipose cells stretch to hold fat Once filled to max capacity, cells begin to multiply Mobilizing Stored Fat TG in adipose; want to release FAs for E Activates enzyme inside adipose cell HSL Hormone-sensitive lipase HSL breaks down TG G & FAs FAs blood Hydrophobic, so bound to protein carrier: albumin cells metabolized for E USING FAT TO MAKE ATP What kind of fat gets used for energy? What is triglyceride made of? ______________ _____________ C-C-C _____________ C-C Krebs ATP ETS C-C C-C C-C C-C C-C C-C C-C C-C C-C C-C C-C C-C C-C C-C C-C C-C C-C C-C C-C C-C C-C C-C C-C C-C Glycerol is converted to pyruvate can either glucose or acetyl CoA /Krebs/ATP Fatty Acids (too large to enter Krebs cycle) can ONLY enter energy metabolism at Therefore, So what’s the point? If we are out of glycogen and need to make glucose for those glucosedependent tissues, we aren’t going to be able to use fatty acids to do it. Summary of ATP Production From Fat Fat is comprised mainly of TG molecules Glycerol and 3 FAs Glycerol (3C) enters energy metabolism at pyruvate FAs (broken down to 2C units) enter at acetyl CoA Fat can provide a very small amount of glucose form the glycerol Complete oxidation of TG yields ATP, CO2, H2O and body heat. Cardiovascular Disease Cardiovascular Disease – general term for diseases of the heart and blood vessels Coronary Heart Disease (CHD) – AKA Coronary Artery Disease– lack of blood flow to the network of blood vessels surrounding (and serving) the heart. major cause: atherosclerosis. Atherosclerosis – thickening and hardening of the walls of the blood vessels 2 deposits of fatty material (plaque) esp. coronary and carotid arteries and abdominal aorta Heart Attack – Lack of blood flow to the heart muscle resulting in tissue damage and sometimes sudden death Stroke –blood flow to a part of the brain is cut off “brain attack.” Usually due to atherosclerosis in the carotid arteries. Atherosclerosis Slow, progressive disease which begins in childhood and takes decades to advance. Coronary arteries are most often affected. “Response to Injury Theory” Fatty streaks form along arterial walls Proliferation of smooth muscle cells, WBCs and calcium plaques Plaques cause the arteries to lose elasticity Thrombosis: Embolism: Angina: pain, pressure, and tightness in chest, back, neck, and arms caused by Hypertension The FOUR major risk factors: 1. Smoking HDL, BP, increases platelet stickiness (clots) 2. Hypertension cardiac work, arterial damage Risk : 3. Elevated blood cholesterol major lipid in plaque 4. Lack of regular exercise Sedentary people (60% of US) have double the risk of developing CVD as active people. Other risk factors include: Heredity – parent or sibling male under 55, woman under 65 Gender – male women post menopause without estrogen Age Stress and personality type Type “A” personality, stress, depression Elevated triglycerides Inversely correlated w/HDL’s Homocysteine Strong + correlation w/premature disease with inadequate B vitamins (folate, B6 and B12 – fruits and veggies, lean meats) Also: Exercise Strengthens heart muscle Lower body fat (also affects diabetes) Better glucose control blood pressure stress Exercisers are less likely to be smokers Improved lipid profile (LDL, HDL) blood clotting Dietary Prevention of Heart Disease Fat Saturated fat Mono vs. Poly Trans FAs Sodium Alcohol Antioxidants and Phytochemicals Fiber Fish Soy