Birth cohorts: What have we learned? The next Frontier
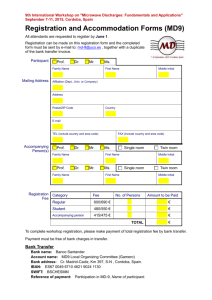
advertisement

The C anadian H ealthy I nfant L ongitudinal D evelopment Study – Preliminary data November 27, 2015 Padmaja Subbarao, MD, MSc FRCP(C) Clinician-Scientist Co-Director, CHILD Study Hospital for Sick Children University of Toronto Toronto, Canada Disclosures No commercial or other interests other than a bias towards pulmonary function outcomes! Objectives • to review the CHILD study pulmonary function measures • to discuss the Toronto subcohort infant pulmonary function measures • to present preliminary data from the Toronto subcohort pulmonary function group N Engl J Med 2003; 349: 1414-1422 Longitudinal lung function by asthma outcome at age 26 Sears MR, et al. N Engl J Med 2003;349:1414-22 Males Males It all happens in early Re childhood Canadian Healthy Infant Longitudinal Development Study Exposures Pollution Work & School environment Home environment Genetics Immune phenotypes Clinical phenotypes Infant Pulmonary Function Microbiome Stress Diet Viruses SES Pets Recruitment of a general population cohort Inclusion criteria Exclusion criteria • Pregnant women aged >18 years (19in Vancouver) • Residential proximity (<50km) to participating delivery hospital • Able to read, write and speak English • Willing to donate cord blood • Planning to deliver at a designated recruitment centre participating hospital • Infant born at or after 35 weeks • Children born with major congenital abnormalities or respiratory distress syndrome • Expectation of moving away from a recruitment centre within 1 year of recruitment • Children of multiple births • Children resulting from in-vitro fertilization • Children who will not spend at least 80% of nights in the index home Current recruitment sites for CHILD National Coordinating Centre Key variables obtained by questionnaires HOME MOTHER FATHER CHILD Current residence Maternal demographics Paternal demographics Mode of delivery Previous residences (12 mo) Maternal health Paternal health Medications around birth Changes of residence Maternal medications Paternal medications Sleeping arrangements Type and age of home Maternal smoking Paternal smoking Activities outside home Characteristics of home Maternal respiratory symptoms Paternal respiratory symptoms Colds and infections Attached garage Maternal diagnosed asthma Paternal diagnosed asthma Coughing episodes Heating and cooling systems Maternal allergies Paternal allergies Wheezing episodes Humidifiers Maternal occupation Paternal occupation Medications Basement/crawl space Health of other children Hobbies and activities in home Food allergy Water leaks and mold Health during pregnancy Atopic dermatitis / eczema Swimming pool, spa Diet before and in pregnancy Doctor visits Renovations Vitamins and supplements Hospital/ER visits Furniture Prenatal/postnatal maternal stress Breastfeeding Cooking systems Socioeconomic status Introduction of milk, solids Cleaning habits Depression module Vaccinations Chemicals used in home Labor and delivery Time/activity/locations Smoking in the home Post-partum health Travel times and exposures Characteristics of bedroom Post-partum stress Daycare arrangements Animals in home (pets) Breastfeeding Insects and pests in home Parenting stress Model of genetic and environmental determinants of lung function PRENATAL EXPOSURE ASSESSMENT POSTNATAL EXPOSURE ASSESSMENT ETS Air Pollution (GIS Modelling) Child Nutrition Maternal Nutrition Breastfeeding Viral infection PFT (Entire cohort) 3 year 5 year – complete 2019 PFT (Toronto) PFT (Toronto) 18 month PFT (Toronto) 12 month PFT (Toronto) 3 month PFT (Toronto) Nasal microbiome Birth Mould* (28-32 weeks) Dust allergen & Microbiome* Nasal microbiome Birth weight Prenatal *From standardized home assessment Diagnosis of Asthma in > 8 • 3 features must be considered: 1. Symptoms. 2. Variable airflow obstruction. a) Spirometry: >12% BDR, >20% FEV1 b) PEF: >20% variability c) Methacholine challenge: <8mg/mL 3. Airway inflammation (not required for diagnosis). Canadian Asthma Consensus Guidelines, 1999 Preschool Asthma Diagnosis Ducharme CRJ 2015 Preschool prediction rule Frequent wheezing < 3y AND: Minor Criteria Major Criteria 1. Parental MD asthma 2. MD eczema 3. Sensitivity to aeroallergen 1. 2. 3. 4. MD allergic rhinitis Wheezing apart from colds Eosinophilia ≥ 4% Sensitivity to egg, milk or peanut 1/2 Major + 2/3 Minor: 97% sensitivity but PPV 47%. Castro-Rodriguez, AJRCCM, 2000 Guilbert, Cont Clin Trials, 2004 Pulmonary Function Measures 1. Spirometry – infancy, 3 & 5 years 2. Multiple Breath Washout – infancy, 3 & 5 years 3. Forced Oscillation tests – 3 & 5 years *In the full cohort only spirometry at 5 years SPIROMETRY FVC FVC Spirometry in Preschool • Tracking • 73% success rate in 2-4 year olds if accept FEV0.5 • Need to have incentive programs • Technical aspects • End of test criteria Raised Volume Rapid Thoracoabdominal Compression • Sedated infant • Mask applies extra volume • Jacket provides assisted expiration Journal of Applied Physiology 1998 Pre 1 ** * * Pre 2 Post Multiple Breath Washout (MBW) • An inert gas washout test – first described 60 years ago – repurposed for modern use • Tidal breathing measure, requires virtually no effort and thus is possible in all ages. • Sensitive measure of gas mixing in the small peripheral airways. • Add complementary information to spirometry. Multiple Breath Washout (MBW) - an inert gas washout test Inert gases Do not participate in gas exchange Low solubility in blood and tissue Resident inert gases: Ar (40), N2 (28) Extrinsic inert gases: CH4 (16), He (4), SF6 (146) (MM) = Molecular Mass Ventilation distribution homogeneity The efficiency with which inspired gas mixes with the resident gas in the lungs Tidal volume Ventilation distribution Nitrogen Washout Factors and mechanisms involved in the gas exchange IV III II I Expired Gas Volume Airway resistance Diffusion V´A/Q´matching Lung elasticity Tidal volume Ventilation inhomogeneity Nitrogen Washout Factors and mechanisms involved in the gas exchange IV III II I Expired Gas Volume Airway resistance Diffusion V´A/Q´matching Lung elasticity Tidal volume Ventilation inhomogeneity Nitrogen Washout Factors and mechanisms involved in the gas exchange IV III II I Expired Gas Volume Airway resistance Diffusion V´A/Q´matching Lung elasticity Multiple Breath Washout (MBW) SF6 Gas Supply 4% SF6 Flow Analyzer Mass Spec Wash-in Phase 26 Multiple Breath Washout (MBW) SF6 [SF6] 4% 4% SF6 Sample time Flow Analyzer Mass Spec Wash-out Phase Expiration 27 Multiple Breath Washout (MBW) SF6 [SF6] 4% Room Air 4% SF6 Sample time Flow Analyzer Mass Spec Wash-out Phase Inspiration 28 Multiple Breath Washout (MBW) SF6 [SF6] 4% 4% SF6 Sample time Mass Spec Wash-out Phase Expiration 29 Multiple Breath Washout (MBW) SF6 Healthy Infant Healthy infant Infant with cystic fibrosis Parameters from MBW Lung Clearance Index • Most commonly reported parameter • Measures ventilation distribution homogeneity (the efficiency with • which inspired gas mixes with the resident gas within the lung). The number of FRC lung volumes to reduce the inert tracer gas to 1/40th (2.5%) of its initial starting concentration. LCI = Cumulative Expired Volume FRC A higher LCI = “worse” lung disease Data from CHILD Infant Pulmonary Function (IPFT) Subcohort Toronto Cohort N= 768 231 Infants 430 Infant Test visits IPFT Cohorts: 1. Tucson – 127 2. Perth – 250 3. COPSAC (hi-risk) – 400 None have longitudinal data in preschool. Early Infant visit N = 132 Mid Infancy N = 221 Late Infancy N = 77 109 MBW 75 Pleth 50 RVRTC 183 MBW 165 Pleth 107 RVRTC 59 MBW 38 Pleth 28 RVRTC IPFT & Preschool Subcohort Toronto Cohort N= 768 231 Infants 430 Infant Test visits 635 (82%) 3 year visits completed Still on going 177 (77%) F/U from IPFT 523 (80%) acceptable PFT 369 (70%) MBW 348 (66%) Spiro IPFT Cohorts: 1. Tucson – 169 – F/U 11y (74%) 2. Perth – 243 – F/U 6 y (48%) 3. COPSAC (hi-risk) – 400 – F/U – 7 years (77% f/u) None have longitudinal data in preschool. Demographics of the full dataset 3 Month N Mean Std 1 year N Mean Std 18 month N Mean Std Birth weight (gram) 118 3432.16 447.9 182 3421 488 85 3297 464.7 Birth length (cm) Weight (kg) Height (cm) Age (year) Calulated BMI=weight / squared(_CLENHEI) BMI-for-age z-score Length/height-for-age zscore Weight-for-age z-score Weight-for-length/height zscore Age in months 78 119 119 119 51.79 7.56 66.05 0.5 5.83 1.22 3.36 0.14 124 184 184 184 50.82 9.76 75.34 1.08 2.88 1.2 3.54 0.15 52 85 85 85 51.01 11.09 81.25 1.61 2.51 1.34 4.3 0.16 119 17.25 1.87 184 17.17 1.51 85 16.81 1.93 112 0.04 1.21 181 0.4 0.99 85 0.63 1.23 112 -0.27 1.09 181 -0.26 1.12 85 -0.53 1.36 112 -0.12 1.01 181 0.14 0.96 85 0.11 0.91 112 0.11 1.22 181 0.36 0.97 85 0.52 1.18 119 6.03 1.71 184 12.94 1.85 85 19.28 1.89 In conclusion • Very little is known about the early life lung function trajectories. • We found that many factors impact lung function and some differentially. • The interaction of the microbiome and virome with diet and dust and its associations with pulmonary function is a key area of interest for CHILD. Strategic Focus of CHILD Research • To understand key relationships and interactions among the many genetic determinants and environmental exposures associated with the development of asthma, and use this understanding to prevent it and improve its treatment. • Multiple asthma/allergy hypotheses related to: Innate immunity Genetic risk, epigenetic effects Microbiome Nutrition Infant lung function Viral infections Psychosocial effects, stress Environmental exposures • Data collection has been expanded to provide for the study of development of other chronic non-communicable diseases including metabolic (obesity, diabetes) and cardiac disorders. 38 CHILD Study Funding Private donors – Sick Kids Foundation