Storage of Medical Gases
advertisement

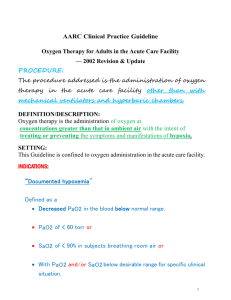
Oxygen Therapy & Adjuncts RET 2274 Respiratory Care Theory 1 Module 4.0 Oxygen Therapy & Adjuncts In consultation with the physician, a skilled clinician should be able to assess the patient’s need for oxygen therapy, determine the desired goals of therapy, select the mode of administration, monitor the patient’s response, and recommend and implement timely and appropriate changes Oxygen Therapy & Adjuncts General Goals and Clinical Objectives Correct documented or suspected acute hypoxemia Decrease symptoms of associated with chronic hypoxemia Decrease the workload hypoxemia imposes on the cardiopulmonary system Oxygen Therapy & Adjuncts AARC Clinical Practice Guidelines (Excerpts) Indications Demonstrated hypoxemia as evidenced by: PaO2 60 mm Hg or an SaO2 90% on room air Neonates: PaO2 <50 mm Hg, SaO2 <88%, or capillary PO2 <40 mm Hg Acute care situation in which hypoxemia is suspected Severe trauma Acute myocardial infarction Short-term therapy, e.g., post anesthesia recovery Oxygen Therapy & Adjuncts Assessing Need – Monitoring Aids ABG Pulse oximetry PaO2 SaO2 SpO2 Bedside Calculations CaO2 O2 Oxygen Therapy & Adjuncts Assessing Need – Clinical Signs & Symptoms Respiratory Cardiovascular Tachypnea Dyspnea Cyanosis Tachycardia Hypertension Neurologic Restlessness Confusion Headache Oxygen Therapy & Adjuncts Assessment of Outcome Improvement of Need Indicators ABGs SpO2 Physical Symptoms Respiratory Cardiovascular Neurologic Oxygen Therapy & Adjuncts Hazards of Oxygen Therapy Oxygen Toxicity (lung tissue destruction) Oxygen-Induced Hypoventilation In patients with chronic hypercapnia Absorption (Absorptive) Atelectasis At FiO2s ≥ 50% Nitrogen washout Retinopathy of Prematurity (ROP) AKA retrolental fibroplasia Possible at FiO2s as low as 30% Oxygen Therapy & Adjuncts Oxygen Delivery Systems Low-Flow O2 Delivery Devices Provide part of the patient’s inspiratory gas flow needs – remainder comes from the room air FiO2 is variable because it is dependent upon the patient’s tidal volume (Vt) and respiratory rate (f) Note: Increases or decreases in Vt or respiratory rate f alter the delivered FiO2 Oxygen Therapy & Adjuncts Oxygen Delivery Systems High-Flow O2 Delivery Devices Provide a given oxygen concentration at a flow that equals or exceeds the patient’s inspiratory gas flow needs – all the inspired gas the patient breathes is delivered by the oxygen device and none is provided by the room air Note: Increases or decreases in Vt or f do not alter the delivered FiO2 Oxygen Therapy & Adjuncts Low-Flow O2 Delivery Devices Nasal Cannula A disposable plastic device consisting of two nasal prongs (approximately 1 cm in length) that insert directly into the vestibule of the nose and are connected to several feet of small-bore oxygen tubing. The oxygen supply tubing connects directly to a flowmeter or bubble humidifier. Oxygen Therapy & Adjuncts Low-Flow O2 Delivery Devices Nasal Cannula Oxygen flow from 1 – 6 L/min enters the patient’s nose, filling the anatomic reservoir (nasopharynx and oropharynx) First 50 ml of each breath (adult) is pure oxygen, the remainder consists of oxygen mixed with room air FiO2 varies with patient’s Vt and respiratory rate Oxygen Therapy & Adjuncts Low-Flow O2 Delivery Devices Nasal Cannula Cautions Too high of a flow can cause discomfort, nasal dryness, bleeding Newborns and infants – maximum 2 L/min Oxygen Therapy & Adjuncts Low-Flow O2 Delivery Devices Nasal Cannula Oxygen supplied via nasal cannula at flowrates ≤ 4 L/min need not be humidified Oxygen Therapy & Adjuncts Low-Flow O2 Delivery Devices Nasal Cannula Oxygen Concentrations 100% O2 flow in liters 1L 2L 3L 4L 5L 6L Approximate FiO2 0.24 0.28 0.32 0.36 0.40 0.44 Oxygen Therapy & Adjuncts Low-Flow O2 Delivery Devices Nasal Catheter A soft plastic tube with several small holes at the tip. It is advanced along the nasal passage until the tip rests at the level of the uvula If blindly inserted, insert it to depth equal to the distance from the nose to the ear lobe (too deep can cause gagging and possible aspiration) FiO2 delivery is similar to nasal cannula Oxygen Therapy & Adjuncts Low-Flow O2 Delivery Devices Transtracheal Catheter A Teflon (polytetrafluoroethylene) catheter that is surgically inserted into the trachea between the 2nd and 3rd cartilage ring Held in place by a custom-sized chain necklace Connects directly to flowmeter – no humidifier Oxygen builds up in the expanded anatomic reservoir during exhalation Achieves a given PaO2 using 40% - 60”% less O2 Oxygen Therapy & Adjuncts Low-Flow O2 Delivery Devices Transtracheal Catheter Cautions Infection Airway obstruction If patient becomes SOB or has increased WOB, the catheter may be obstructed and needs to be flushed Subcutaneous emphysema Hemoptysis Oxygen Therapy & Adjuncts Low-Flow O2 Delivery Devices Reservoir and Pendant Cannula Reservoir Cannula Designed to conserve oxygen Incorporate a mechanism for gathering and storing oxygen between breaths Decrease oxygen use by providing FiO2 comparable with that of nonreservoir systems but at lower flows Flow: ¼ - 4 L/min, FiO2 0.22 – 0.35 Can reduce O2 use by 50% to 75% Pendant Cannula Oxygen Therapy & Adjuncts Low-Flow O2 Delivery Devices Simple Oxygen Mask Lightweight mask applied to the patient’s face that adds reservoir space (the mask) in addition to the anatomical reservoir During the pause between exhalation and inspiration, the mask and anatomic reservoir fill with 100% O2. During the first part of inspiration, 100% O2 is inhaled. During the latter part, O2 and room are mixed in the mask and inhaled Oxygen Therapy & Adjuncts Low-Flow O2 Delivery Devices Simple Oxygen Mask Input flow range: 5 – 12 L/min FiO2 range: 35% - 50% - varies with patient’s Vt and f Must maintain enough oxygen flow to flush mask of exhaled carbon dioxide Oxygen Therapy & Adjuncts Low-Flow O2 Delivery Devices Partial Rebreathing and Non-Rebreathing Masks Sometimes referred to as reservoir masks Each has a 1 liter flexible reservoir bag attached to the oxygen inlet Because the bag increases the reservoir volume, both masks can provide a higher FiO2 than a simple mask Partial Rebreathing Mask Non-Rebreathing Mask Oxygen Therapy & Adjuncts Low-Flow O2 Delivery Devices Partial Rebreathing Masks When the patient exhales, approximately the first third of expiration is from the anatomic dead space (does not participate in gas exchange and is rich in oxygen) fills the reservoir bag. The remaining exhaled gas exits through the ports in the mask. Between exhalation and inspiration, additional oxygen flows into the mask and reservoir bag. When the patient inhales, a mixture of oxygen and air is inhaled. Has no valves Oxygen Therapy & Adjuncts Low-Flow O2 Delivery Devices Partial Rebreathing Masks Input flow range: 6 – 10 L/min A sufficient enough flow should be applied so that the reservoir bag does not completely collapse during the patient’s inhalation FiO2 range: 40% - 70% - varies with patient’s Vt and f Has no valves Oxygen Therapy & Adjuncts Low-Flow O2 Delivery Devices Exhalation valve Non-Rebreathing Masks Oxygen continually feeds into the reservoir from the O2 supply tubing During inspiration, the expiratory valves close (preventing air dilution) and the inhalation valve opens, providing oxygen to the patient from the reservoir bag During exhalation, the inhalation valve closes (preventing exhaled gas from entering the bag) and the expiratory valve opens allowing exhaled gas to exit the mask Inhalation valve Has 2 one-way valves Oxygen Therapy & Adjuncts Low-Flow O2 Delivery Devices Exhalation valve Non-Rebreathing Masks Input flow range: Minimum of 10 L/min A sufficient enough flow should be applied so that the reservoir bag does not completely collapse during the patient’s inhalation FiO2 range: 60% - 80% - varies with patient’s Vt and f Inhalation valve Has 2 one-way valves Oxygen Therapy & Adjuncts Low-Flow Devices Advantages Ease of use Lower Cost Patient comfort Minimal equipment monitoring and maintenance Useful when precise FiO2 is not required Disadvantages Does not provide precise FiO2 FiO2 varies with respiratory pattern Oxygen Therapy & Adjuncts High-Flow O2 Delivery Devices All high-flow O2 devices mix air and oxygen via an air entrainment system to achieve a given FiO2 All the inspired gas the patient breathes is delivered by the oxygen device and none is provided by the room air Note: Increases or decreases in Vt or f do not alter the delivered FiO2 Oxygen Therapy & Adjuncts High-Flow O2 Delivery Devices Basic components of an air-entrainment system. Pressurized gas passes through a nozzle or jet, beyond which are air-entrainment ports. Shear forces at the jet orifice entrain air into the primary gas stream, diluting the oxygen and increasing the total flow output of the device. Oxygen Therapy & Adjuncts High-Flow O2 Delivery Devices Venti or Air-Entrainment Mask The device consists of a jet orifice around which is an air-entrainment port. The body of the mask has large ports that allow excess flow from the device and exhaled gas from the patient to escape Oxygen Therapy & Adjuncts High-Flow O2 Delivery Devices Venti or Air-Entrainment Mask FiO2 is regulated by using different adaptors with specific combinations of entrainment ports and jet sizes developed by manufacturers Oxygen Therapy & Adjuncts High-Flow O2 Delivery Devices If enough flow is provided from the device, the patient will not entrain any room air, thus, preventing the dilution of the FiO2 being delivered by the device – the patient will receive a constant FiO2 with every breath This remains true only if the patient’s inspiratory flow demands do not exceed the flow from the mask Oxygen Therapy & Adjuncts Total device flow must equal 3 – 4 times the patient’s minute volume As a rule of thumb, total flow from an air entrainment device should be at least 60 lpm To accomplish that objective . . . Using the device’s air/oxygen entrainment ratio, determine the oxygen flow required to guarantee the prescribed FiO2. Oxygen Therapy & Adjuncts High-Flow O2 Delivery Devices Air to Oxygen Entrainment Ratios Room Air-to-O2 Ratio 25:1 10:1 8:1 5:1 3:1 1.7:1 1:1 0.6:1 0:1 O2 Concentration 24% 28% 30% 35% 40% 50% 60% 70% 100% Oxygen Therapy & Adjuncts High-Flow O2 Delivery Devices Computing Air-to-Oxygen Ratios Liters of Air Liters of O2 = 100 – %O2 %O2 – 21 Oxygen Therapy & Adjuncts High-Flow O2 Delivery Devices Computing Air-to-Oxygen Ratios %O2 40% Liters of Air Liters of O2 Liters of Air Liters of O2 = 100 – 40 40 – 21 Liters of Air Liters of O2 = 60 19 Liters of Air Liters of O2 = 3 1 = 100 – %O2 %O2 – 21 Oxygen Therapy & Adjuncts High-Flow O2 Delivery Devices Computing Air-to-Oxygen Ratios – Magic Box Value for Air Value for Oxygen Oxygen Therapy & Adjuncts High-Flow O2 Delivery Devices Computing Total Flow Output What is the total flow out put of a 40% Venti mask running at 12 L/min? 1. 2. Add air-to-oxygen ratio parts 3+1=4 Multiply the sum of the ratio parts by the O2 input flow 4 x 15 = 48 Answer: A 40% venti mask running at 12 L/min has a total flow output of 60 L/min Oxygen Therapy & Adjuncts When giving a higher FiO2 with an air-entrainment device (e.g., 0.50 – 1.0), it may be necessary to use two devices in conjunction in order to provide a sufficient total flow to meet the patient’s inspiratory demands Oxygen Therapy & Adjuncts High-Flow Adjuncts Aerosol mask Trach mask (collar) Face tent T piece (Brigg’s adaptor) Oxygen Therapy & Adjuncts High-Flow Systems Advantages Provide precise and dependable FiO2 Psychological benefit for some patients due to high flow Disadvantages More complex to use More costly Require closer monitoring and more maintenance Oxygen Therapy & Adjuncts Enclosures Enclosing a patient in a controlled-oxygen atmosphere is among the oldest approaches to oxygen therapy. Liquid Oxygen Tent Designed by Dr. Frank Hartman, 1943 Oxygen Therapy & Adjuncts Enclosures With today’s simpler airway devices, enclosures are generally used only in the care of infants and children. Oxygen Therapy & Adjuncts Enclosures Three major types of oxygen enclosures Oxygen Tents Oxygen Hoods Incubators Oxygen Therapy & Adjuncts Enclosures Oxygen Tents AKA – mist tents, croup tents, croupettes Clear plastic tent or canopy Large enough to enclose a small child Oxygen Therapy & Adjuncts Enclosures Oxygen Tents Provides environmental control of … O2 concentration (.21 - .50) High-output aerosol device (air-entrainment) Humidity High-output aerosol device Temperature Refrigeration coils containing Freon Oxygen Therapy & Adjuncts Enclosures Oxygen Tents Primary usage Pediatric aerosol therapy Croup or cystic fibrosis Problems Wide swings in FiO2 due to opening and closing of tent Canopy must remain tucked in Constant leakage makes a high FiO2 impossible Oxygen Therapy & Adjuncts Enclosures Oxygen Hoods Clear plastic enclosure Placed around the patient’s head Fixed oxygen concentration Air-entrainment device, or blender, connected to inlet port Flow rate must be a minimum of 7 L/min to ensure CO2 is flushed out of hood Oxygen Therapy & Adjuncts Enclosures Oxygen Hoods Cautions Oxygen seems to be layered (highest concentration near the bottom of hood) O2 concentration needs to be measured intermittently with an O2 analyzer near the infants face When caring for premature infants, ensure that the gas is warmed to a precise temperature and humidified May induce cold-stress O2 consumption and even apnea Oxygen Therapy & Adjuncts Enclosures Incubators Plexiglas enclosures Provide a neutral thermal environment Servo-controlled heating Supplemental oxygen Humidity is provided with an external heated humidifier or nebulizer Oxygen Therapy & Adjuncts Enclosures Incubators FiO2 is highly variable because of frequent opening Best way to control FiO2 in an incubator is with a Oxyhood FiO2 and gas temperature must be measured within the Oxyhood – continuously Oxygen Therapy & Adjuncts Enclosures Incubators Mechanical ventilation can be provided for infant while in the incubator Ventilator circuit temperature probe must be outside of the incubator