Substance related disorders

PSYCHIATRIC NURSING
SUBSTANCE-RELATED
DISORDERS
Substance-Related Disorders
•
2 groups of substance-related disorders:
1. Substance-use disorders (dependence and abuse).
2. Substance-induced disorders (intoxication, withdrawal, delirium, dementia, amnesia, psychosis, mood disorder, anxiety disorder, sexual dysfunction, and sleep disorders).
Age (18-24), gender (male more than female).
3
• Substance abuse can be defined as using a drug in a way that is inconsistent with medical or social norms and despite negative consequences
I. Substance-use disorders
1.
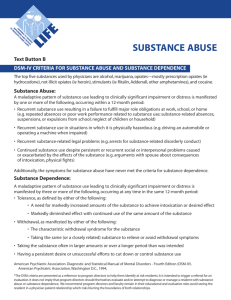
Substance abuse: a maladaptive pattern of substance use manifested by recurrent and significant adverse consequences related to repeated use of the substance, as manifested by one (or more) of the following, occurring within a 12-month period:
A. Recurrent substance use resulting in failure to fulfill major role at work, school, or home.
B. Recurrent substance use in situations in which it is physically hazardous.
C. Recurrent substance –related legal problems.
D. Continued substance use despite having persistent or recurrent social or interpersonal problems.
•
And never met criteria for dependence
4
I. Substance-use disorders
2. Substance dependence a) Physical dependence is evidenced by:
•
A cluster of cognitive, behavioral, & physiological symptoms indicating that the individual continues use of substance even with substance-related problems.
As this condition develops, the repeated administration of the substance is necessary to prevent the appearance of unpleasant effects.
Dependence is promoted by Tolerance: the need for increasing the dose or frequency of the substance in order to obtain desired effects originally produced by a lower dose.
5
I. Substance-use disorders
b) Psychological dependence: this happens when there is an overwhelming desire to repeat the use of particular drug to produce pleasure or avoid discomfort.
• At least three of these characteristics must be present for a diagnosis of substance dependence :
* evidence of tolerance
* evidence of withdrawal symptoms
* a great deal of time is spent in activities necessary to obtain the substance
* impairment/reduce of social, occupational, or recreational activities
* continued substance use despite knowledge that has persistent or recurrent physical or psychological problems
6
7
Substance-use disorders
• persistent desire or unsuccessful efforts to cut down or control use of substance
• substance is often taken in larger amounts or over a longer period than was intended.
II. Substance-induced disorders
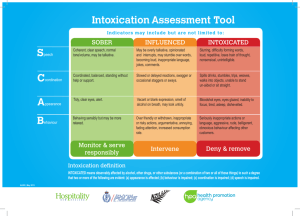
1. Substance intoxication:
Development of a reversible substance-specific syndrome caused by the recent use or exposure to substance. Effect of the substance on the CNS. CNS
Symptoms include violence, mood lability, cognitive impairment, impaired judgment, impaired social or occupational functioning (e.g. alcohol intoxication, getting high or wasted).
Different substances may induce similar effects
Substances inducing intoxication identified in the DSM IV
• Alcohol
• Amphetamines
• Caffeine
• Cannabis
• Cocaine
• Inhalants
• Opiates
• Sedatives/hypnotics/anxio lytics
Clinical picture of intoxication depends on:
• Substance
• Dose
• Duration/chronicity
• Individual degree of tolerance
• Time since last dose
Substance-induced disorders
2. Substance withdrawal: the development of substance–specific syndrome caused by the cessation of, or reduction in, heavy & prolonged substance use.
11
Etiology of substance use disorders
•
Biological factors: a. Genetics (alcoholic children 4 times) b. Biochemical (e.g. alcohol)
• Psychological factors: a. Developmental influences b. Personality factors
•
Socio-cultural factors: a. Social learning (modeling) b. Conditioning (the effect of substance itself…many substances create pleasure)
•
Cultural and ethnic influences.
12
13
Alcohol abuse and dependence
A profile of the substance
• Alcohol is a natural substance formed by the reaction of fermenting sugar with yeast spores.
• Alcohol in drinks is known as ethyl alcohol (C
2 H 5 OH).
• Sometimes seen in medical records as ETOH.
• Classified as food because it contains calories; however, it has no nutritional value.
•
Examples: beer, wine, whisky
• Alcohol produce depressant effect on the CNS (changes in behavior and mood).
• Factors that influence alcohol behavioral changes are: slow consumption, individual size, individual stress or fatigue, whether the stomach contains food.
14
Effects of alcohol on the body
• Peripheral neuropathy.
• Alcoholic myopathy.
• Wernicke’s encephalopathy (ataxia, opthalmoparesis, short memory loss)
• Korsakoff’s psychosis (sever memory loss, apathy, quick change)
• Alcoholic cardiomyopathy.
• Esophagitis.
• Pancreatitis.
• Cirrhosis or hepatic encephalopathy (cause by acetaldehyde).
• Leukopenia.
• Thrombocytopenia.
• Sexual dysfunction.
15
16
Patterns of alcohol use/abuse
• People use alcoholic beverages to enhance the flavor of food with meals, at social gatherings to encourage relaxation & friendliness among the guests, & to promote celebration at special occasions such as weddings & birthdays.
Alcohol intoxication
• BAL (blood alcohol level) 0.08 or 0.1 g/dl- legal definition
• Intoxication occurs at blood alcohol levels between 100-200 mg/dl.
• Death has been reported at levels ranging from 400-700 mg/dl.
•
Symptoms of intoxication: a. Mood lability b. Impaired judgment c. Incoordination d. Unsteady gait e. Flushed face f. Slurred speech g. Nystagmus (uncontrolled movement of the eyes ) h. Impaired social or occupational functioning
17
Alcohol withdrawal
• Occurs within 4 –12 hours of cessation of or reduction in heavy and prolonged alcohol use.
•
Symptoms of withdrawal: a. Nausea or vomiting b. Malaise or weakness c. Tachycardia d. Sweating e. Headache f. Insomnia g. Increased blood pressure h. Coarse tremor of hands, tongue, or eyelids i. Anxiety, depressed mood or irritability j. Transient hallucinations or illusions
18
Sedative, hypnotic, or anxiolytic abuse and dependence
A profile of the substance
•
All these substances are capable of inducing varying degrees of CNS depression, from relief of anxiety to anesthesia, coma, & even death.
1.
The effects of CNS depressants are additive with one another and with the behavioral state of the user.
2.
CNS depressants are capable of producing physiological & psychological dependence to achieve maximum level of functioning or feeling of well-being.
3.
Cross-tolerance & cross-dependence may exist between different CNS depressants.
19
Categories of CNS depressants
•
Barbiturates: a . Pentobarbital–street name (yellow jackets) b . Amobarbital–blue angels
•
Nonbarbiturate hypnotics: a. Triazolam–sleepers b. Flurazepam–sleepers c. Chloral hydrate–Peter, Mickey
•
Antianxiety agents: a. Diazepam (Valium ) b. Alprazolam (Xanax) c. Lorazepam (Ativan )
20
Effects on the body
•
CNS: depression of CNS from sedation to death.
•
Sleep & dreaming: decrease the amount of sleep time spent in dreaming.
•
Cardiovascular: hypotension , decreased cardiac output & decrease cerebral blood flow.
•
Respiratory depression.
•
Decreased body temperature.
•
Produce jaundice: (stimulate the production of liver enzymes).
21
22
Patterns of use/abuse
1) CNS depressants prescribed by physicians as treatment for anxiety or insomnia, & then, independently, the individual increases the dose or frequency to produce the desired effect.
2) Use of substances that were obtained illegally. The initial objective is to achieve euphoria.
Sedative, hypnotic, or anxiolytic
• Mood lability intoxication
• Impaired judgment
• Inappropriate sexual or aggressive behavior
• Impaired social or occupational functioning
• Incoordination
• Unsteady gait
• Impaired attention or memory
• Slurred speech
• Stupor or coma
23
Sedative, hypnotic, or anxiolytic withdrawal
• Short-acting anxiolytics (lorazepam or oxazepam) may produce Sx. within 6-8 hrs of decreasing blood levels. Longer half-lives (diazepam) may not develop Sx. for more than a wk, peaking during 2 nd wk, & decrease in wk 3-4.
•
Symptoms include: a. Sweating. b.Tachycardia (HR>100).
c. Hand tremor. d. Insomnia.
e. Nausea or vomiting. f. Hallucinations.
24 g. Illusions. h. Agitation & anxiety.
CNS stimulant abuse and dependence
A profile of the substance
• The CNS stimulants are identified by the behavioral stimulation & psychomotor agitation that they induce.
• Induce stimulation by augmentation of neurotransmitters, or by direct action on the cellular activity.
• The most prevalent and widely used stimulants are caffeine & nicotine.
• When used in moderation, these stimulants tend to relieve fatigue & increase alertness.
25
Categories of CNS stimulants
Amphetamines: a. Dextroamphetamine–street name (Dexies ) b. Methamphetamine (Meth, speed, ice)
Nonamphetamine stimulants: a. Pemoline b. Phentermine c. Benzphetamine d. Phendimetrazine
Cocaine (crack, lady, snow)
Caffeine (java, cocoa)
Nicotine (weeds, chaw)
26
Patterns of use/abuse
1. Using the substance for the appetitesuppressant effect in an attempt at weight control.
2. The daily user may take large or small doses & may use the drug several times a day. Chronic users tend to depend on
CNS stimulants to feel more powerful, more confident, & more decisive
(vital).
27
Effects on the body
• CNS: CNS stimulation (tremor, anorexia, insomnia, agitation, increased motor activity). Increased alertness & decreased fatigue from amphetamines, nonamphetamines, & cocaine. Chronic use results in paranoia, hallucinations, aggressive behavior.
•
Cardiovascular/pulmonary: hypertension, tachycardia, cardiac arrhythmias, vasoconstriction
(MI), pulmonary hemorrhage, chronic bronchiolitis,
& pneumonia.
GI & renal: constipation, contraction of the bladder sphincter, diuretic effect (caffeine), diarrhea
(nicotine), anorexia, increase body temperature
(amphetamines).
28
•
CNS stimulant intoxication: euphoria, anxiety, tension, anger, stereotyped behaviors, impaired judgment. Pupillary dilation, tachy- or bradycardia, nausea, vomiting, chills, muscular weakness, respiratory depression, chest pain, coma. Hypo- or hypertension, restlessness, nervousness, GI disturbance.
• CNS stimulant withdrawal: dysphoria, unpleasant dreams, insomnia or hypersomnia, increased appetite & wt gain, retardation, agitation, depressive symptoms, nausea, vomiting, fatigue, muscles pain & stiffness.
29
Inhalant abuse and dependence
A profile of the substance
• Aliphatic & aromatic hydrocarbons found in substances such as fuels, solvents, adhesives, & paint thinners.
•
Examples: gasoline, varnish remover, airplane glue, & spray paint.
Patterns of use/abuse :
• Highest use seen from 12-25 years. Less common after age 35 yrs.
• Children may use inhalants several times a wk, often on weekends & after school.
• Adults may use the substance at varying times during each day.
• Methods of using include huffing & bagging.
30
Effects on the body
•
CNS : central & peripheral nerve damage, generalized weakness, peripheral neuropathy, cerebral atrophy, whitematter lesions.
•
GI : abdominal pain, nausea, vomiting, rash around nose and mouth, unusual breath odors.
•
Renal & respiratory : chronic renal failure, respiratory depression leading to death.
31
Inhalant intoxication
Two or more of the following signs are present:
* Dizziness * Blurred vision or diplopia
* Incoordination * Stupor or coma
* Slurred speech * Muscle weakness
* Unsteady gait * Psychomotor retardation
* Lethargy * Tremor
* Depressed reflexes * Euphoria
32
Opioid abuse and dependence
A profile of the substance
• The term
OPIOID refers to a group of compounds that includes opium (juice), opium derivatives, & synthetic substitutes.
• Opioids exert both a sedative & an analgesic effect (relief of pain, Tx. of diarrhea, & relief of coughing).
• Methods of administration of opioid drugs
33 include oral, smoking, S/C, I/M, I/V.
Categories of opioids
Opioids of natural origin
Morphine
Codeine street name
(White staff)
Cody, syrup
Opioid derivatives Heroin
Hydromorphone
Horse, Harry
Lords, little D
Synthetic opiatelike drugs
Meperidine
Methadone
Fentanyl
34
Doctors
Dollies
China girl
Patterns of use / abuse
1. Obtain the drug by prescription from physician for relief of a medical problem then increase dose, justifying this behavior as Sx. treatment.
2. Use the opioid drugs for recreational purposes & obtain them from illegal sources.
• Opioids may be used alone or in combination with stimulants or other drugs to enhance the euphoric effect.
35
Effects on the body
•
CNS: euphoria, mood changes, mental clouding, pain reduction, drowsiness, pupillary constriction, antitussive response, respiratory depression, nausea
& vomiting.
•
GI: therapeutic effect in the treatment of severe diarrhea. Constipation & fecal impaction with chronic use.
•
Cardiovascular: relieve pulmonary edema & pain of cardiac infarction (morphine). Hypotension at high doses (direct action on heart or opioid-induced histamine release).
• Sexual functioning: decreased sexual pleasure
(from heroin). Retarded ejaculation, impotence, & orgasm failure.
36
37
Opioid intoxication
Symptoms include:
Initial euphoria followed by…
Apathy
Dysphoria
Impaired judgment
Agitation or retardation
Pupillary constriction (or dilation)
Slurred speech
Impaired attention or memory
Respiratory depression, coma, & even death (with severe intoxication)
Opioid withdrawal
Symptoms occur within 6-12 hrs, peaking in 1-3days, & subside in 5-7 days:
* Dysphoric mood * Sweating
* Nausea or vomiting * Insomnia
* Muscle aches * Diarrhea
* Pupillary dilation * Fever
* Abdominal cramping * Piloerection
* Rhinorrhea or lacrimation
38
Hallucinogen abuse and dependence
A profile of the substance
• Hallucinogenic substances are capable of distorting an individual’s perception of reality; they have the ability to alter sensory perception (“mind expanding”).
• Some are produced synthetically; others are natural products of plants and fungi.
39
Categories of hallucinogens
Naturally occurring Mescaline (half moon ) hallucinogens
Psilocybin & psilocyn
Synthetic compounds
Phencyclidine (Peace pill)
Lysergic acid diethylamide
[LSD] (acid, big D, cupcakes)
40
Effects on the body
* Nausea and vomiting * Chills
* Pupil dilation * Increased V/S
* Mild dizziness * Loss of appetite
* Sweating * Insomnia
* Paranoia, panic * Euphoria
* Fear of losing control * Derealization
* Sense of slowing of time
* Heightened body awareness
* Heightened response to color & sounds
41
42
Hallucinogen intoxication
• Marked anxiety or depression
• Ideas of reference
• Fear of losing one’s mind
• Paranoid ideation
• Depersonalization
• Illusions & hallucinations
• Pupillary dilation
• Blurred vision
• Tremors & incoordination
• Palpitations
Cannabis abuse and dependence
A profile of the substance
• Is second only to alcohol as the most widely abused drug.
• It occurs naturally in the plant
Cannabis sativa .
• Cannabis products are usually smoked, can also be taken orally.
• It produces CNS depression.
43
Cannabinoids (cannabis category)
Cannabis Marijuana Mary Jane
Hay
Texas tea
Composed of dried leaves, stems, & flowers of the plant.
Hashish Ganja
Bhang
Hash
Derived from the flowering tops of the plant.
44
45
Patterns of use/abuse
• Many people incorrectly regard cannabis as substance of low abuse potential; this false belief has promoted use of this substance by some individuals who believe it is harmless.
• Tolerance, although it tends to decline rapidly, does occur with chronic use.
• Marijuana is the
MOST WIDELY USED illicit drug among high school students.
Effects on the body
•
Cardiovascular: Tachycardia, hypotension, decreased myocardial oxygen supply, & increased oxygen demand.
•
Respiratory: Laryngitis, bronchitis, cough, hoarseness, lung damage & cancer, bronchodilatation.
•
CNS: Euphoria, relaxed inhibitions, disorientation, depersonalization, sensory alterations, impaired recent memory & judgment, tremor, muscle rigidity, conjunctival redness.
46
Cannabis intoxication
Symptoms of intoxication include:
• Impaired motor coordination
• Euphoria & anxiety
• Sensation of slowed time
• Impaired judgment
• Dry mouth
• Increased appetite
• Tachycardia
• Conjunctival injection
47
Cannabis withdrawal
The symptoms of withdrawal appear only when individuals abruptly stop taking high doses of cannabis. Symptoms of cannabis withdrawal include:
• Irritability
• Restlessness
• Insomnia
• Anorexia
• Mild nausea
48
49
Application of the nursing process
Assessment
• In the pre-introductory phase of relationship development, the nurse must examine his/her feelings about working with a client who abuses substances.
• The role that alcohol or other substances has played in the life of the nurse will affect the way in which he/she approaches interaction with substance-abusing client.
• Unless nurses understand & accept their own attitudes & feelings, they cannot be empathetic toward clients’ problems.
•
Michigan Alcoholism Screening Test (MAST) is one of the most useful assessment tools for drug abuse patients.
50
Diagnosis
Possible nursing diagnoses for clients with substance-related disorders:
• Ineffective denial related to weak, underdeveloped ego evidenced by “ I don’t have a problem with (substance).
I can quit any time I want to”
• Ineffective coping related to inadequate coping skills & weak ego evidenced by use of substances as a coping mechanism
• Risk for infection related to malnutrition & altered immune condition
• Risk for suicide related to depressed mood (withdrawal from CNS stimulants )
51
Outcome
• Has not caused harm to self or others
• Demonstrates more adaptive coping mechanisms that can used in stressful situations (instead of taking substances)
• Shows no signs or symptoms of infection or malnutrition
• Verbalizes importance of abstaining from use of substances in order to maintain optimal wellness
52
Planning
• Detoxification :
provide a safe & supportive environment.
administer substitution therapy as ordered .
• Intermediate care:
provide explanations of physical symptoms.
promote understanding & identify the causes of substance dependency.
provide education & assistant in course of treatment to client
& family.
• Rehabilitation:
assist client to identify alternative sources of satisfaction.
provide support for health promotion & maintenance.
promote participation in outpatient support system.
53
Client/family education
•
Nature of the illness:
* effects of substance on the body.
* ways in which use of substance affects life.
• Management of the illness:
* relaxation techniques.
* problem-solving skills.
* the essentials of good nutrition.
• Support services:
* financial assistance.
* legal assistance.
* one-to-one support person.
54
55
56
Psychopharmacology for substance intoxication & substance withdrawal:
SUBSTITUTION THERAPY
57
Alcohol
• Benzodiazepines, Librium, Serax, Valium, &
Xanax are
THE MOST COMMONLY
USED
agents for substitution therapy in alcohol withdrawal.
• Anticonvulsant therapy (Carbamazepine,
Gabapentin) for management of withdrawal seizures.
• Multivitamin therapy, in combination with daily thiamine, is required to prevent neuropathy, confusion, & encephalopathy.
58
59
Opioids
• Opioid intoxication is treated with narcotic antagonists such as naloxone, naltrexone, or nalmefene.
• For withdrawal, methadone is given on the
1 st day to suppress the symptoms.
• Buprenorphine is less powerful than methadone, but is considered safer and causes fewer side effects.
• Clonidine also has been used to suppress opiate withdrawal symptoms.
Depressants
• Substitution therapy for CNS depressant withdrawal (particularly barbiturates) is most commonly with long-acting barbiturate phenobarbital
(Luminal).
60
• Long-acting benzodiazepines are commonly used for substitution therapy when the abused substance is a nonbarbiturate CNS depressant.
Stimulants
• Treatment of intoxication begins with minor tranquilizers such as chlordiazepoxide
(Librium), & progresses to major tranquilizers such as haloperidol (Haldol).
• Treatment of withdrawal is usually aimed at reducing drug craving & managing severe depression.
• Desipramine has been especially successful with symptoms of cocaine withdrawal & abstinence (self-control).
61
Hallucinogens and cannabinols
• Substitution therapy is not required with these drugs.
• When adverse reactions occur (anxiety or panic), benzodiazepines (diazepam) may be prescribed to prevent harm to the client or others. Psychotic reactions may be treated with antipsychotic medications.
62