Assessment 6 Pulmonary
advertisement
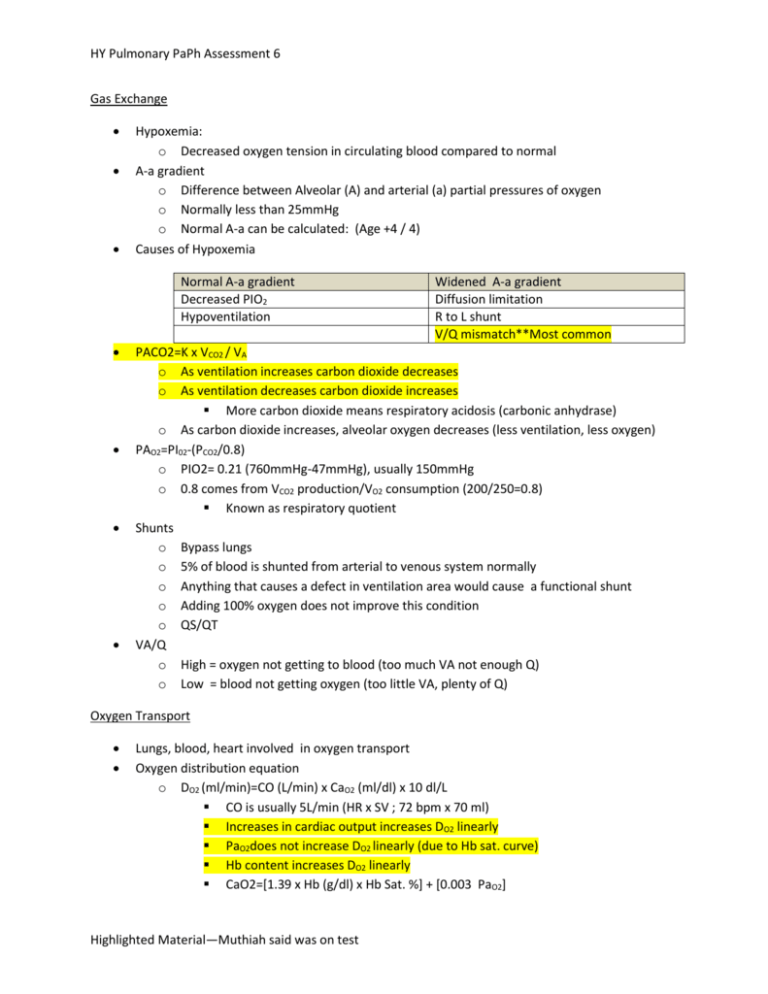
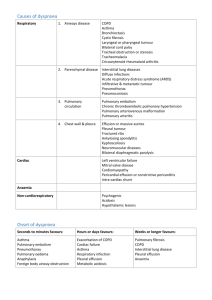
HY Pulmonary PaPh Assessment 6 Gas Exchange Hypoxemia: o Decreased oxygen tension in circulating blood compared to normal A-a gradient o Difference between Alveolar (A) and arterial (a) partial pressures of oxygen o Normally less than 25mmHg o Normal A-a can be calculated: (Age +4 / 4) Causes of Hypoxemia Normal A-a gradient Decreased PIO2 Hypoventilation Widened A-a gradient Diffusion limitation R to L shunt V/Q mismatch**Most common PACO2=K x VCO2 / VA o As ventilation increases carbon dioxide decreases o As ventilation decreases carbon dioxide increases More carbon dioxide means respiratory acidosis (carbonic anhydrase) o As carbon dioxide increases, alveolar oxygen decreases (less ventilation, less oxygen) PAO2=PI02-(PCO2/0.8) o PIO2= 0.21 (760mmHg-47mmHg), usually 150mmHg o 0.8 comes from VCO2 production/VO2 consumption (200/250=0.8) Known as respiratory quotient Shunts o Bypass lungs o 5% of blood is shunted from arterial to venous system normally o Anything that causes a defect in ventilation area would cause a functional shunt o Adding 100% oxygen does not improve this condition o QS/QT VA/Q o High = oxygen not getting to blood (too much VA not enough Q) o Low = blood not getting oxygen (too little VA, plenty of Q) Oxygen Transport Lungs, blood, heart involved in oxygen transport Oxygen distribution equation o DO2 (ml/min)=CO (L/min) x CaO2 (ml/dl) x 10 dl/L CO is usually 5L/min (HR x SV ; 72 bpm x 70 ml) Increases in cardiac output increases DO2 linearly PaO2does not increase DO2 linearly (due to Hb sat. curve) Hb content increases DO2 linearly CaO2=[1.39 x Hb (g/dl) x Hb Sat. %] + [0.003 PaO2] Highlighted Material—Muthiah said was on test HY Pulmonary PaPh Assessment 6 Normally 165 Normally 15g of Hb in 1 dl of blood 15g x 1.39=20.85g/dl Note: The 1.39 is at 100% hemoglobin saturation Normally adult consumes 250 ml O2/min VO2 (ml O2/min) = CO(L/min) x [CaO2-CvO2]x 10 (dl/L) This equation calculates the consumption of oxygen in the body CvO2=1.39 x Hb x SvO2 +(.003 x PvO2) Figure 1. Hb Sat. Curve (KNOW THIS) Curve shifts to Rdeceased affinity for oxygen COPD Chronic bronchitis is a disease of airways, not alveoli o 3 months in 2 years of excessive coughing with copious sputum production o Increased reid index Emphysema is a disease of alveoli and small airways Bronchiectasis=necrotizing infection of bronchi leading to dilation of airways COPD definition: disease state characterized by airflow limitation that is not completely reversible o Major mechanism of hypoxemia in COPD patients is a V/Q mismatch445 Allergic Bronchopulmonary asperigillosis o Criteria: o 1)asthma, 2)immediate cutaneous rx. To a. fumigates, 3)IgG ab to A. fumigates, 4)IgE>1000ng/ml, 5) Increased IgE Ab to A. fumigates o Type III hypersensitivity Nocturnal asthma Highlighted Material—Muthiah said was on test HY Pulmonary PaPh Assessment 6 o Decline of catecholamines/cortisol at night (thus decreased b-2 activity) leads to nocturnal asthma o Tx. o Tx. With albuterol or salmoterol o PEFR worse at night due to this, best at 4pm worst at 4am Methacholine challenge w/ no asthma signs can rule out asthma (High NPV) Drug induced asthma triad o Aspirin o Nasal polyps o Asthma Restrictive Lung Disease Can be due to loss of lung, pleura, chest wall, or NMJ abnormalities Respiratory failure=hypoxemia in absence of hypercapnia Ventilatory failure= hypercapnia Hypercapnia develops from o Increase in dead space o Decrease in minute ventilation o Increase in carbon dioxide poisoning Give oxygen to hypercapnic patients! o Three reasons why carbon dioxide goes up after giving oxygen o Haldane effect o Worsening V/Q mismatch ** main cause o PCO2 inversely related to ventilation o Pt. with COPDgiven 40% oxygen and CO2 goes up, should we cut oxygen? NO Keep on oxygen and increase until at least 88% sat. Keep on mechanical vent. CO2 increases upon giving oxygen due to Haldane effect, and respiratory muscle fatigue Hypoxemia of ILD due to V/Q mismatch Type II pneumocytes increase in ILD Ground glass appearance on CXR Increased lymphocytes=sarcoidosis, Increased PMN’s=pneumonia Normal BAL: 90% macrophages, 10% lymphocytes, <1% PMNs Increased thickness and decreased surface area cause a decrease in DLCO!!! 40 y/o sandblaster, FEV<80%, DLCO less than 80% what was involved? Silicosis o What does this predispose to ? TB o ARDS TNF-alpha, IL-1: Inflammation, Coagulation, Tissue Repair Highlighted Material—Muthiah said was on test HY Pulmonary PaPh Assessment 6 ARDS characterized by acute decrease in lung compliance High grade systemic inflammation in ARDS Treatment w/ Mechanical Ventilator’ in ARDS, 6-8c, decrease in tidal volume prevents further damage and decreased mortality Increase PEEP to improve oxygenation in ARDS Non-survivors have increased pro-inflammatory cytokines o Patients have a huge shunt area once alveoli are collapsed o PEEP allows to break shunt o MODS can develop Pleural Effusions Visceral pleura: cells are loose Parietal pleura: cells are tight Normal content of pleural fluid: colorless, protein<1.5g, 1500 cells/ml Pleural fluid moves from parietal pleuravisceral pleura where it is reabsorbed o Hydrostatic pressure gradient o (Pc-Ppl) - (pic-pipl) Only parietal pleura has lymphatic openings Increased hydrostatic pressureheart failuretransudate Decreased pleural pressureatelectasistransudate Decreased oncotic pressure of plasmalow albumintransudate Increased oncotic pressure of pleural fluidinflammationexudate o o o o o pH, glucose, cell count etc. do not effect difference between transudate and exudates KNOW THIS FOR TEST KNOW FOR TEST Know the differences between exudates and transudates Protein>0.5 and LDH > 0.6 are indicative of an exudates (ratio’s of fluid/serum amounts), also >60mg/dL cholesterol Most frequent cause of pleural effusion is heart failure Increased permeability (Slide 14) o Increased production of fluid due to increased inflamed area (infection, inflammation, cancer) causes increased vascular permeability and increased protein concentration in pleural effusion o KNOW FOR TEST Etiology of Pleural Effusion (Slide 17) o Heart failure is the leading cause, KNOW THIS o Know what is present in pleural fluid (remember must have >10mm on lateral decubitus film to perform!) Especially: Color, total protein, LDH, cholesterol, and WBC count o Know lymphocytic exudates in pleura Most likely cause: Tuberculosis or cancer Rule in TB with acid fast bacteria stain Highlighted Material—Muthiah said was on test HY Pulmonary PaPh Assessment 6 <1000cell/ml=transudate >5k=chronic exudates (TB, cancer) >10K=inflammation (pneumo, pancreatitis, pulmonary infarction) >50K = parapneumonic effusions only Pneumonia Aspiration=bacteria Inhalation=atical pneumonia, viruses, etc. Test questions (from Dr. Muthiah): 1. What determines outcome in patients with pneumonia? Host response 2. Bronchial breath sounds are a sign of consolidation. THIS IS ON TEST. 3. ARDS can be is frequently a complication of pneumonia. 4. Resolution of pneumonia if right antibiotic is started, first thing that gets better is oxygenation (respiratory rate decreases). Radiologic resolution of pneumonia lags behind clinical resolution of pneumonia (especially if patient has other lung disease) 5. Patient detioriates rapidly is most likely due to MRSA (strain USA-300) and also produces a Panton-valentine-leukocydin toxin which destroys neutrophils 6. Drug of choice for MRSA? Vancomycin. A. Know: Age, social habits, occupation, geography, co-morbidities, are all risk factors for CAP. Don’t memorize the specifics just the general categories. Resolution happens usually within 6-8 weeks DVT/PE II. Test Question: (Slide 2),KNOW FOR TEST A. 25 year old man studying for the bar exam the last two weeks is confined to a chair 20 hours per day. Now at Methodist hospital ER, he has developed right sided pleuretic chest pain. 1. Pleuretic pain is sharp well localized to the lateral area of chest increasing with cough (inflamed pleura rub against other pleura) 2. Afebrile, HR=122, RR=32, D-Dimer =2200 ng/ml, CXR is clear Highlighted Material—Muthiah said was on test HY Pulmonary PaPh Assessment 6 3. Diagnosis is pulmonary embolism most likely from deep venous thrombosis B. Which of the following statements are true regarding pulmonary thromboembolism? (this is on our test) 1. Pathognomonic EKG finding of S1Q3T3 is seen only in a minority of patients. a) KNOW THIS FOR TEST III. Factor V leiden mutation (KNOW FOR TEST) A. Factor V activates protein C which is a natural anticoagulant IV. Protein C/S, antithrombin III deficiencies V. Prothrombin G20210A deficiency VI. Estrogen use, hormonal changes, malignancy, and thrombocytosis can cause a hypercoaguable state (Slide 14) A. KNOW ABOUT ESTROGEN USE AND DVT FOR TEST VII. Impaired gas exchange A. Most likely due to V/Q mismatch (#1 cause of hypoxemia in patients), KNOW FOR TEST VIII. Compensation by the circulation KNOW FOR TEST, (Slide 20) A. Vasodilation of uninvolved vasculature 1. Decrease the increase in pulmonary vascular resistance 2. Improves V/Q ratio 3. Improves overall oxygenation IX. (Age +4) / 4 is normal A-a gradient for a person 1. Note A-a gradient may be normal in pulmonary embolisms X. Chest Radiography PE (Slide 29) A. Usually they are normal, KNOW FOR TEST B. Pleural effusions are pretty small when present with pulmonary embolism XI. Westermark’s Sign (Slide 34), KNOW FOR TEST A. No vascular markings in R.lung because of a massive PE that cutoff circulation in the r. pulmonary artery XII. Recap (Slide 59) A. More than 90% of emboli come from lower extremities B. Normal perfusion scan excludes PE If scan is normal or d-dimer is <500 the possibility of DVT is extremely low. Applicable in low clinical probability settings. KNOW FOR TEST XIII. Fat Embolism (Slide 74), KNOW FOR TEST A. Farmer who falls of tractor, tractor runs over long bones (which is associated with fat emboli) and goes to lungs and causing a triad of: 1. Mental status change 2. Thrombocytopenia 3. Petechiae in chest and neck 4. Diagnosis is fat embolism, KNOW FOR TEST COPD Test Questions: (From Dr. Muthiah) 1. Photomicrograph of emphysema asking you to ID emphysema Highlighted Material—Muthiah said was on test HY Pulmonary PaPh Assessment 6 Normal Emphysema 2. Case scenario asking physician who has COPD, descriptive statements about chronic bronhicits vs. emphysema (both have obstructive patterns, emphysema has out of proportion decrease in DLCO differentiates chronic bronchitis from emphysema) 3. Treatments that prolong life in COPD: Smoking cessation and oxygen therapy a. Management of stable COPD includes all of the following except? i. Oral systemic glucocorticoids in patients with mild COPD, KNOW FOR TEST b. Used short & long acting bronchodilators, anti-cholinergic bronchodilators can also be used c. Long term management with oxygen therapy (at least 15-24 hours a day), KNOW FOR TEST d. PaO2 less than 55 is an indication for oxygen therapy e. Characterized by abnormal enlargement of airspaces distal to terminal bronchioles i. Centri-lobular 1. Most common due to cigarette smoking ii. Pan-Acinar 1. Most common due to alpha-1-antitrypsin def. iii. Centrilobular emphysema is most common, KNOW FOR TEST f. Major site of airflow limitation is the small conducting airways (<2mm in diameter), KNOW FOR TEST. 4. In asthma there is predominately CD4 T lymphocytes, in COPD there is predominately CD8 Tlymphocytes. KNOW FOR TEST. a. Production of sputum for 3 months in 2 consecutive years is the clinical definition of chronic bronchitis. KNOW FOR TEST b. DLCO is reduced in COPD patients with emphysema (it is normal in chronic bronchitis, and asthma!), KNOW FOR TEST c. TB has caseating granuloma’s (will be on assessment 7), KNOW FOR TEST 5. Pulmonary embolism (Slide 63) a. Most common is a normal chest radiograph, KNOW FOR TEST b. Features of benignity, KNOW FOR TEST i. Well defined nodules ii. No assosciated lymph node or mediastinal masses iii. No satellite lesions iv. Calcified nodules Highlighted Material—Muthiah said was on test HY Pulmonary PaPh Assessment 6 6. Types of Benign Calcification (Slide 70) a. Dense calcification and popcorn calcifications b. Lamellar calcification c. KNOW FOR TEST 7. Features of malignancy (Slide 72) a. Lymph node spread b. Spiculated nodules c. Pressence of cavitation d. Non-calcified nodules e. Larger nodules f. KNOW FOR TEST 8. Slide 57 is on our test, KNOW FOR EXAM. 9. Know anatomy of lung for the exam 10. Two questions will be on our test from this picture A. Westermark’s sign (complete lack of vasculature in one of lungs), KNOW FOR TEST, Slide 66 (see below figure) Highlighted Material—Muthiah said was on test