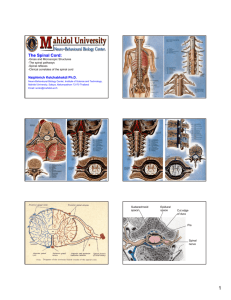
Internal structure of spinal cord
advertisement

Internal Structure of Spinal Cord Laminae of Rexed • 10 divisions based on cellular architecture of the spinal cord. It is numbered from dorsal to ventral • Lamina I. top of dorsal horn - thin layer of small stellate cells & large neurons – receive incoming Dorsal Root fibers – send some axons to contralateral spinothalamic tract • Lamina II. substantia gelatinosa - very small, dense cells (gelatinosa cells) with highly branched dendrites – receive afferent dorsal root axon collaterals & descending fibers from reticular formation – send unmyelinated axons to dorsolateral tract - ascend or descend a few segments – give off branches at several levels to other laminae of dorsal horn – thought to be involved especially in modulation & throughput of pain perception • Lamina III. interneurons - receive dorsal root axons; send axon branches to other Dorsal Horn laminae – II and III (substantia gelatinosa) functions in regulating afferent input to the spinal cord. • Lamina IV. tract cells - long dendrites extend into Lamina II, III; – axons cross midline to contralateral spinothalamic tract – projects to the lateral cervical nucleus, the posterior column nuclei and the thalamus (spinothalamic tract) • Lamina I-IV all receive inputs from dorsal root, IV most • V-VI. base of Dorsal Horn (indistinguishable in humans) – has long-dendrite tract cells similar to IV; and many various interneurons – afferent fibers = some dorsal root afferent; and especially. descending corticospinal fibers (their major target) – Tracts cells from Lamina IV, V, and VI are generally referred as nucleus proprius – Lamina 5 and 6 receives proprioceptive input AND sensory information relayed by lamina 4. These are the sites of origin of ascending projections to higher centers • Intermediate zone: – VII. largest region of the spinal gray matter • many interneurons with collaterals within their segment and long axons that go out into the white matter & travel up/down to other segments’ gray matter • VII also contains a few other cell columns (not part of the Lamina system) – Nucleus dorsalis (nucleus thoracicus /Clarke’s column:) • in medial/base of dorsal horn/upper intermediate, T1-L3 big neurons, axons make up dorsal spinocerebellar tract • ventral spinocerebellar tract originates from lamina V, VI and VII and from neurons from the edge of the ventral horn in lumbar region (spinal border cells) – Intermediolateral cell column: in lateral horn of T1-L2 • Cell bodies of preganglionic neurons of sympathetic nervous system • Anterior / Ventral horn: (motor & interneurons) • VIII. mostly in medial side of ventral horn ( covers width of ventral horn in part of thoracic segments) – receives terminals of descending fibers from vestibulospinal & reticulospinal tracts – sends to ipsilateral & contralateral to lamina VII & IX at their level & a few other close levels – participates in movements of muscles in the head and neck • IX. columns of motor neurons within boundary of VII or VIII – axons make up ventral roots: alpha-motor neuron to skeletal muscle (gamma motor neuron to muscle spindles) four motor neuron columns = dorsolateral; central; ventromedial; ventrolateral . The axial muscles (neck, trunk) are represented medial and ventrally whereas limbs are represented in lateral and dorsal part of the spinal cord • In Cervical cord (L IX): – a. Phrenic nucleus: in ventromedial column, C3-C5, innervates diaphragm muscle – b. Spinal accessory nucleus: C1-C5, lateral VH • axons in rootlets join to form spinal root, ascends through foramen magnum; joins with cranial root (XI cranial nerve) to form accessory nerve - exits through jugular foramen • spinal root innervates trapezius & sternocleidomastoid • Nucleus of Onuf at S2 level – most ventral part of ventral horn – contribute to pudendal nerve - pelvic floor, including sphincters of fecal and urinary continence. • Commissural area: • X. immediately around central canal, smaller neurons than surrounding laminae – receives some afferents from dorsal root – contains decussating (crossing) fibers, glia cells – contains neurons that project to the opposite side of the cord • Dorsal afferent fibers predominately terminate in the dorsal horn. Impulses concerned with pain, temperature, and touch reach the tract cells from which spinothalamic tract originates. Pain signals are modified mainly in Lamina II. Dorsalis nucleus of thoracic and upper lumbar gives off dorsal spinocerebellar tract. • Dorsal horn – Each dorsal root branches into six to eight rootlets. These axons enter the dorsallateral tract (Lissauer) where they divide into ascending or descending branches terminating in their own or immediately adjacent segments. • Ventral horn – Lamina IX has two types of motor neurons, alpha (numerous, large in diameter) and gamma (less numerous, small). Alpha innervates muscle cells and gamma innervates muscle spindles. • Lateral horn – Sympathetic efferent neurons, located in the thoracic and upper lumbar segments only (T1 – L2). • Intermediate zone: – Sacral autonomic nucleus: lateral horn S2S4 • – Cell bodies of sacral PSN preganglionic Intermediomedial cell column: just lateral to X (through out the length of spinal cord • thought to be involved in visceral reflexes; Internal structure of spinal cord • A. White matter - stains black or dark blue with Weigert's stain – is composed of axons that form tracts or funiculi – ascending or descending - travel rostrally or caudally – divided into 3 areas: dorsal, ventral & lateral funiculi Dorsal Funiculus • between dorsal gray horns • axons from dorsal root ganglia (DRG) ascend ipsilaterally; • carry sensory discrimination for tactile, proprioception, movement, vibration, synapse in Nuclei gracile and nuclei cuneate in medulla then cross over to the contralateral side. • Different pathway for discriminative touch and proprioception Receptors • Sensory receptors: – exteroceptors: response to pain, temperature, touch, pressure on skin • like free nerve endings, Merkel endings, Pacinian corpuscles – proprioceptors: in muscles, tendons, joints, provide information for awareness of position and movement • like neuromuscular spindles, Golgi tendon organs (neurotendinous spindles) Discriminative touch • Receptors are tactile receptors (Meissner’s corpuscles), sent to dorsal root ganglia – fasciculus gracilis - medial - lower extremity, somatotopic origins (lower = more medial) – fasciculus cuneatus - lateral - appears above midthoracic level (information from the upper extremity) – Both funiculi terminate to gracile and cuneate nucleus, respectively at medulla level. Then by internal arcuate fibers cross over to the contralateral side, project to ventral posterior nucleus of thalamus by medial lemniscus, then to the ipsilateral primary somesthetic cortex (be aware the medial lemniscus turns 90, then lower body information is on the lateral side now) . Three levels of perception • primary afferents neurons (pathway) at dorsal root ganglia (spinal cord level) • At the medulla, the primary afferents finally synapse. The neurons receiving the synapse are now called the secondary afferents neurons. • At thalamus, a third and final neuron will go to cerebral cortex, the final target. Proprioception • Receptors are neuromuscular spindles, neurotendeninous spindles, • Upper limb: – Same as above mentioned mechanism Proprioception • Lower limb: – dorsal funiculus goes only up to mid-thoracic level, terminates into nucleus dorsalis – axons from nucleus dorsalis ascend ipsilaterally as dorsal spinocerebellar tract. At medullar level, before entering cerebellum by inferior cerebellar peduncle, gives off collaterals entering nucleus Z (rostral to gracile nucleus), which are concerned with conscious proprioception from the lower limb. – Cells from nucleus Z then give rise to internal arcuate fibers that cross the midline and join the medial lemniscus, then enter the ventral posterior nucleus of thalamus, then primary somatosensory cortex ipsilaterally. Proprioception • - also carry descending fibers: • a. from nucleus gracile, and nucleus cuneate modulation of sensations from higher centers • b. from dorsal root ganglia afferents - help coordinate / integrate sensory info from nearby levels • c. spinal gray - thought to coordinate upper & lower limbs in reflexes Lateral funiculus • Ascending: • 1. dorsal spinocerebellar tract: – begins from above L3 – axons from ipsilateral Nucleus dorsalis (Clarke’s column cells) to ipsilateral cerebellar cortex via inferior cerebellar peduncl – Participates the pathway for lower limb proprioception (see above) Lateral funiculus • 2. ventral spinocerebellar tract: – mostly from contralateral spinal border cells of ventral horn at edge of lumbar sacral ventral horn – largely crossed fibers ascend up to midbrain level turns into superior cerebellar peduncle – fibers cross again in cerebellum before entering to cerebellar cortex – therefore, deliver sensory info from same side of body – Both spinocerebellar (ventral and dorsal) carry same side of the information into cerebellum. Although, dorsal tract entering the cerebellum via the inferior cerebellar peduncle and ventral by the superior cerebellar peduncle. Lateral funiculus • lateral spinothalamic tract: carry pain, temperature, light touch sensations • Receptors are nociceptor (nerve endings) for pain, Merkel etc for light touch, unknown receptors for temperature. Fibers enter the dorsal lateral tract. Axons from dorsal horn (nucleus proprius) IV, VVI cross the midline in ventral white commissure, then travels ipsilaterally in the ventral part of lateral funiculus end in the ventral posterior nucleus of the thalamus. Spinothalamic • upper limb is represented more medial (close to the gray matter); lower is lateral, superficially (somatotopically arranged) • From medulla level up , spinothalamic fibers constitute most of the spinal lemniscus, which also includes fibers from spinotectal tract Lateral funiculus • Other tracks in lateral funiculus – spinotectal tract: same source as spinalthalamic tract; cross, then up to superior colliculus, midbrain reticular formation – spinoreticular tract: • probably pain perception for internal organs • originates from laminae IV-VIII crossed midline to pontine reticular formation (crossed) • from ipsilateral side, terminates to medullary reticular formation (uncrossed) Lateral funiculus • Descending: (modify ascending activities) • lateral corticospinal tract: – Originate from frontal and parietal lobes, pass through internal capsule, basis pedunculi, midbrain, pons – Cross as medullar level to enter (become) lateral funiculus. • a. fibers from frontal lobe: end in ventral horn & intermediate zone of gray matter • b. fibers from parietal lobe : end in dorsal horn gray matter Lateral Corticospinal Tract • Functionally, these tracts (lateral and anterior) have a strong influence on voluntary motor activity. Some of the fibers of the lateral corticospinal tract terminate directly on the motor neurons (anterior horn cells) of the spinal cord, particularly those involved in fine motor control of the fingers and hand. Most others act via the interneurons of the anterior horn, which then influence the motor neurons. Lateral Corticospinal Tract • Damage to the corticospinal tract results in changes in modulation of the deep tendon reflexes to cause hyperreflexia and spasticity at segments below the level of corticospinal damage. The three clinical characteristics of hyperreflexia are amplitude of reflex, speed of action and spread of reflex. Other descending tracts • Rubrospinal tract – from contralateral Red Neucleus - only extends to C2 in humans • Medullary reticulospinal tract: – – – – from nucleus reticular formation control motor neurons mostly ipsilateral, but some fibers cross in medulla control of un/ subconscious motor activity (corticospinal tracts control skilled/conscious movement) Ventral funiculus • Descending: • 1. ventral corticospinal tract = uncrossed portion of corticospinal tract • These then cross in the anterior commissure of the cord at the level where fibers synapse with the anterior horn cell Anterior Spinothalamic Tract • Light (crude) touch and pressure – Info to dorsal spinal ganglion, synapse with substantia gelatinosa group (Lambda II, III) – Second order cross to the opposite side and ascend as anterior spinothalamic tract, new fibers are added to the medial aspect of the track as it goes up (lower lateral, upper medial) – At medula level, joins with lateral spinothalamic tract and spinotectal tract to form spinal lemniscus Anterior Spinothalamic Tract • The spinal lemniscus continues to ascend to the ventral posterolateral nucleus of thalamus (third order neuron) • Axons from third order neuron, then project to post central gyrus Other tracks in anterior funiculus • (lateral) vestibulospinal tract: uncrossed fibers from lateral vestibular nucleus of medulla – terminates at Lamina VIII, & medial VII – mediates equilibrium reflexes • descending medial longitudinal faciculus: (also called medial vestibulospinal tract) – from medial vestibular nucleus of medulla – mediates equilibrium-oriented head movements primarily in upper cervical levels Spinal cord damage • 1. This initial period of "hypotonia" after upper motor neuron injury is called “Spinal Shock” and reflects the decreased activity of spinal circuits suddenly deprived of input from the motor cortex and brainstem Spinal cord damage • After several days, however, the spinal cord circuits regain much of their function for reasons that are not fully understood. Thereafter, a consistent pattern of motor signs and symptoms emerges, including: Upper motor neuron damage • The Babinski sign – Seen in spinal cord injury and infants with incomplete upper motor neuron control Upper motor neuron damage • Spasticity. Spasticity is increased muscle tone, hyperactive stretch reflexes, and clonus (an oscillatory motor response to muscle stretching). Extensive upper motor neuron lesions may also be accompanied by rigidity of the extensor muscles of the leg and the flexor muscles of the arm (called decerebrate rigidity; see below). Spasticity is probably caused by the removal of inhibitory influences exerted by the cortex on the postural centers of the vestibular nuclei and reticular formation. Upper motor neuron damage • Hyporeflexia of superficial reflexes. Further signs are the decreased vigor (and increased threshold) of superficial reflexes such as the corneal reflex, superficial abdominal reflex (tensing of abdominal muscles in response to stroking the overlying skin), and the cremasteric reflex in males (elevation of the scrotum in response to stroking the inner aspect of the thigh). The mechanism of this diminishment of superficial reflexes is not well understood. Upper motor neuron damage • A loss of the ability to perform fine movements. If the lesion involves the descending pathways that control the lower motor neurons to the upper limbs, the ability to execute fine movements (such as independent movements of the fingers) is lost. Lower motor neuron damage • The cell bodies of the lower neurons are located in the ventral horn of the spinal cord gray matter and in the motor nuclei of the cranial nerves in the brainstem. • Symptoms include paralysis (flaccid), loss of or paresis (weakness) of the affected muscles, loss of reflexes (areflexia) due to interruption of the efferent (motor) limb of the sensory motor reflex arcs Assessment of Spinal Cord Damage • Dermatome Assessment of Spinal Cord Damage • Spinal reflexes: – – – – Biceps reflex: C5 to C6 Triceps reflex: C6 to C8 Quadriceps reflex (Knee jerk reflex), L2 – L4 Gastrocnemius reflex (ankle reflex), S1 to S2 Biceps reflex • The biceps reflex is elicited by placing your thumb on the biceps tendon • Biceps reflex: C5 to C6 Triceps reflex • The triceps reflex is measured by striking the triceps tendon directly with the hammer while holding the patient's arm with your other hand • Triceps reflex: C6 to C8 Knee Jerk Reflex • With the lower leg hanging freely off the edge of the bench, the knee jerk is tested by striking the quadriceps tendon directly with the reflex hammer • Quadriceps reflex (Knee jerk reflex), L2 – L4 Ankle Reflex • The ankle reflex is elicited by holding the relaxed foot with one hand and striking the Achilles tendon with the hammer and noting plantar flexion • Gastrocnemius reflex (ankle reflex), S1 to S2 Lou Gehrig's disease • Amyotrophic lateral sclerosis (ALS), sometimes called Lou Gehrig's disease, is a rapidly progressive, invariably fatal neurological disease that attacks the nerve cells (neurons) responsible for controlling voluntary muscles. Both upper and lower motor neurons are damaged. Lou Gehrig's disease • Symptoms of upper motor neuron damage include stiffness (spasticity), muscle twitching (fasciculations), and muscle shaking (clonus). Symptoms of lower motor neuron damage include muscle weakness and muscle shrinking (atrophy).