Pediatric Cardiopulmonary Resusscitation
advertisement

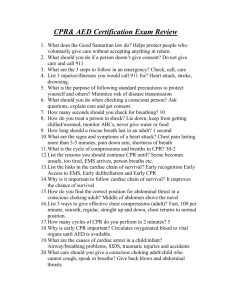
Pediatric Cardiopulmonary Resuscitation Hany El-Zahaby Ain Shams University 2011 Aim “It is not a substitute for getting trained in Pediatric Life Support Courses rather than providing theoretical background that will help you having more solid information about different aspects of pediatric life support” Historical Background Early 19th century: Neonates successfully resuscitated with mouth-tomouth resuscitation In 1814, a description of the Rules of the Humane Society for recovering drowned persons Let one the mouth, and either nostril close While through the other the bellows gently blows. Thus the pure air with steady force convey, To put the flaccid lungs again in play. Should bellows not be found, or found too late, Let some kind soul with willing mouth inflate; Then downward, though but lightly, press the chest. And let the inflated air be upward prest. External cardiac massage was successfully conducted more than 100 years ago in two children (ages 8 and 13 years) after circulatory arrest precipitated by chloroform anesthesia. In 1904, Crile described the effectiveness of external cardiac compressions in maintaining the circulation of dogs. 1947: Beck and associates successfully internally defibrillated the human heart. 1956: Zoll and colleagues performed the first successful external defibrillation of a human heart. 1958: The National Academy of Sciences National Research Council recommended mouth-to-mouth resuscitation with maximum backward tilt of the head as the preferred technique for all individuals requiring emergency artificial ventilation. 1960: External cardiac compression as a resuscitation technique was revived, combined with artificial respirations. Epidemiology and Outcome of In-hospital Pediatric Cardiopulmonary Arrest 70% 60% 50% 40% 30% 20% 10% 0% ICU ER Wards OR/PACU • • • • • A 2006: National Registry of Cardiopulmonary Circulation registered 880 pediatric events, excluding delivery room or neonatal intensive care unit. The median age was 5.6 years. The mean duration of cardiopulmonary resuscitation (CPR) for the children who survived to hospital discharge was 27.3 minutes (median, 15 minutes). 27% percent of the children survived to hospital discharge. 58% of these with a good neurologic outcome. Diagnosis of Cardiac Arrest (10 Seconds) Outside OR: -absence of signs of life (response to stimuli, breathing, movement). -absence of pulse. Inside OR: -ECG will indicate nonperfusing rhythms such as VF or asystole. -ETCO2 will decrease precipitously. -Pulse oximeter will lose its regular waveform. - absence of pulse. Mechanics of CPR ABC algorithm (Airway, Breathing, Circulation) with the exception that the child with VF or pulseless VT should receive electrical defibrillation without delay. CPR should be conducted up until the earliest moment when the shock can be delivered. ABC: A-Airway Bag-valve-mask (BVM) ventilation with proper head tilt-chin lift and jaw thrust (avoid gastric insufflations). Tracheal intubation ensures optimal control of the airway for effective ventilation, multiple attempts at intubation by the inexperienced operator may seriously compromise the child's ability to recover. Auscultation of the is useful in verifying endotracheal tube placement in children together with in-line capnography. ABC: B-Breathing • Visible chest movement (F.B., bilateral tension pneumothorax) • Avoid over-ventilation (decrease venous return, less than normal minute ventilation to match less COP) Ventilations/Compressions for All Ages Respirations Chest Compressions Notes BMV 2 /15 2/30 (single rescuer) 100/min Aspirate stomach if interferes with ventilation ETT 8-10/min 100/min Do not pause compressions during ventilation ABC: C-Circulation Chest-encircling method for cardiac compressions in a neonate (<6M) Infant chest compression: two-finger technique ABC: C-Circulation Chest compression in small children Chest compression in older children ABC: C-Circulation (1) ensuring adequate rate. (2) ensuring adequate chest wall depression (one third to one half of the anteroposterior chest diameter). (3) releasing completely between compressions to allow full chest wall recoil. (4) minimizing interruptions in chest compressions. (5) ensuring that the child is on a sufficiently hard surface to allow effective chest compressions. In short, “push hard and push fast,” release completely, and don't interrupt compressions unnecessarily. Mechanisms of Blood Flow Compliant Chest Wall Cardiac pump Thoracic pump Defibrillation/Cardioversion • Immediate management in children with VF or pulseless VT. • Ventricular fibrillation is terminated due to simultaneous depolarization and sustained contraction of a critical mass of myocardium, which allows return of spontaneous coordinated cardiac contractions, assuming the myocardium is well oxygenated and the acid-base status is relatively normal. Practical Aspects of Pediatric Defibrillation • Correct paddle size: The largest paddle size appropriate for the child should be used to reduce the density of the current flow, which in turn reduces myocardial damage (adult size>10kg). • Paddle force (firmly applied). • Paddle position: One paddle is placed to the right of the upper sternum below the clavicle, the other is positioned just caudad and to the left of the left nipple. An alternative approach is to place one paddle anteriorly over the left precordium and the other paddle posteriorly between the scapulae. • Gel pads interface not touching each other. • Free flowing oxygen 1 meter away to avoid sparking, but keep closed ventilator circuit connect ventilator on. Acute cardiac dysfunction inside OR • Open-Chest Defibrillation: 2 cm for infants, 4 cm for children, 5J in infants. • Automated External Defibrillation: Appropriate for use in children older than 1 year of age with pediatric mode or with pediatric attenuator pads. • Transcutaneous Cardiac Pacing For temporary electrical cardiac pacing in children with asystole or severe bradycardia due to defect in impulse formation or conduction with preserved myocardial function. Vascular Access and Fluid Administration • ‘’Early IV access is a key factor for success’’. • Intraosseous Access: • IO needle, 16-18G cannula, or 18G spinal • 2cm below, 1cm medial to tibial tuberosity. • Complications: osteomyelitis, fat or bone marrow embolism or compartment syndrome. Endotracheal Medication Administration • Epinephrine, atropine, Lidocaine, and naloxone. • Ionized medications such as sodium bicarbonate or calcium chloride is not recommended by this route. • 10% serum level of the IV route ► 10 times dose (0.1mg/kg) for bradycardia or pulseless arrest with maximum volume of 5ml with each injection why?. • Complication? Monitoring During CPR Adequacy of bilateral chest expansion. Constantly reevaluate the depth of compression and the position of the rescuer's hands in performing chest compressions by palpation of a major artery. Pulse oximeter. ETCO2 reflects adequate CPR (transient ↓ after epinephrine) Direct diastolic arterial pressure ► coronary & cerebral perfusion. Temperature: - hypothermic arrest ► continue CPR until 35◦. Peri-arrest hyperthermia should be aggressively treated to improve outcome. Medications Used During CPR Epinephrine Actions: - α- adrenergic stimulation: ↑ PVR & SVR , ↑ SBP & DBP, ↑ coronary BF and likelihood of return of spontaneous circulation. - β-adrenergic stimulation: ↑ myocardial contractility & HR, relaxes smooth muscle in the skeletal muscle vascular bed & bronchi,↑ the vigor and intensity of ventricular fibrillation, increasing the likelihood of successful defibrillation. Medications Used During CPR Epinephrine Complications: • Worsen myocardial ischemic injury. • ↑oxygen demand. • Post-resuscitative tachyarrhythmias, hypertension, pulmonary edema. • ↑ hypoxemia (increase alveolar dead space ventilation by pulmonary BF redistribution). • VC impairs reperfusion of kidneys & GIT. ‘’Routine use of large dose epinephrine in in-hospital pediatric cardiac arrest should be avoided’’. Medications Used During CPR Atropine • Parasympatholytic agent, increasing the sinus rate and shortening atrioventricular node conduction time. • Dose: 20µ/kg, with a minimum dose of 100µ (why?) and a maximum dose of 2.0 mg. • Route, IV, IO, ET, IM, SC. • Onset: 30 seconds, peak 1-2 min after IV dose. “Epinephrine is the drug of choice for asystole or severe bradycardia with hypotension in pediatric CPR” Medications Used During CPR Vasopressin • Because of the paucity of pediatric data, vasopressin is considered Class Intermediate by the American Heart Association in pediatric CPR although Class IIB for adults to replace the second or third dose of epinephrine. Medications Used During CPR Sodium Bicarbonate • The routine use of sodium bicarbonate during CPR remains controversial, and it remains American Heart Association Class Indeterminate. Medications Used During CPR Calcium Indication: Hypocalcemia, hyperkalemia, hypermagnesemia, and calcium channel blocker overdose. Doses: Calcium chloride 20 mg/kg (maximum 0.5 to 1g). Calcium gluconate 60 mg/kg (maximum 2 g). Slowly through a large-bore, free-flowing intravenous line, preferably a central venous line. When administered too rapidly, calcium may cause bradycardia, heart block, or ventricular standstill. Severe tissue necrosis occurs when calcium infiltrates into subcutaneous tissue. Medications Used During CPR Glucose • The administration of glucose during CPR should be restricted to children with documented hypoglycemia because of the possible detrimental effects of hyperglycemia on the brain during or after ischemia Medications Used During CPR Amiodarone • Amiodarone has now supplanted lidocaine as the first drug of choice for medical management of shock-resistant ventricular tachycardia and fibrillation. α- adrenergic blocking ► VD & ↑ coronary BF β- adrenergic blocking CCB► ↓ A-V conduction K+ channel blocking with tissue accumulation Doses: life threatening arrhythmia 5mg/kg (over10 min) then 1020 mg/kg/day Avoided in hypomagnesemia & electrolyte imbalance for fear of “torsades de pointes”. Heart block (postoperative) with drugs that prolong QT interval as inhalational anesthetics. Lidocaine Class IB antiarrhythmic ,↓ automaticity of ectopic focci in ventricles, ↓conduction & ↑effective refractory period in Perkinje fibers. Normal cardiac and hepatic function, bolus of 1mg/kg of lidocaine followed by a intravenous infusion at a rate of 20 -50μg/kg/min is given. If the arrhythmia recurs, a second bolus at the same dose can be given. In children with severe diminution of cardiac output, a bolus of no greater than 0.75 mg/kg, followed by an infusion at the rate of 10 to 20 μg/kg/min, is administered. In children with hepatic disease, dosages should be decreased by 50%. Toxic effects of lidocaine occur when the serum concentration exceeds 7 to 8 μg/ml: seizures, psychosis, drowsiness, paresthesia, disorientation, agitation, tinnitus, muscle spasms, and respiratory arrest. Adjunctive CPR Techniques Open-Chest CPR • During and after thoracic surgery in ICU. • Compared with closed-chest CPR, it generates greater cardiac output and vital organ blood flow, with less elevation of intrathoracic, right atrial, and intracranial pressure, resulting in greater coronary and cerebral perfusion pressure and greater myocardial and cerebral blood flow. Adjunctive CPR Techniques Extracorporeal Membrane Oxygenation • In institutions with the ability to rapidly mobilize an extracorporeal circuit, extracorporeal CPR should be considered for refractory pediatric cardiac arrest when the condition leading to arrest is reversible and when the period of no flow (cardiac arrest without CPR) was brief. Survival with a good neurologic outcome is possible after more than 50 minutes of CPR in selected children who were resuscitated via extracorporeal CPR. • Extracorporeal CPR should be reserved for children who have effective CPR initiated immediately after cardiac arrest. Adjunctive CPR Techniques Active Compression-Decompression • Negative-pressure “pull” on the thorax during the release phase of chest compression using a hand-held suction device. • Improve vascular pressures and minute ventilation during CPR in animals and humans by enhancing venous return. • Studies: Contradicting results. • Complications: Fatal rib and sternal fractures. Adjunctive CPR Techniques Interposed Abdominal Compression • IAC-CPR : The delivery of an abdominal compression during the relaxation phase of chest compression. 1- Return venous blood to the chest during chest relaxation. 2- Increase intrathoracic pressure and augments the duty cycle of chest compression. 3- Compress the aorta and return blood retrograde to the carotid or coronary arteries. • Human studies : increase in aortic pressure and coronary perfusion pressure during IAC-CPR compared with conventional CPR. The risk of injury to intra-abdominal organs during IAC-CPR has not been evaluated. Special Cardiac Arrest Situations Hyperkalemia • Diagnosis: history, progression of ECG changes, initial laboratory results. • Aim of treatment: 1-Antagonize the effects of hyperkalemia at the myocardial cell membrane, increasing the threshold for fibrillation by calcium chloride/gluconate. 2-Shift potassium from the extracellular to the intracellular compartment by sodium bicarbonate and hyperventilation, insulin with dextrose (0.1 unit/kg of insulin with 2 ml/kg of dextrose 25%). Special Cardiac Arrest Situations Supraventricular Tachycardia • It is a common arrhythmia in infants and children. • If no circulatory compromise: vagal maneuver such as ice to the face may be tried first before adenosine. • The initial dose is 0.1 ► 0.2 ► 0.4 mg/kg given as a rapid intravenous bolus (central Vs peripheral). • In neonates, repeated doses of 0.05 mg/kg are given until termination of the arrhythmia up to a maximum dose of 0.25 mg/kg. • If circulatory compromise: immediate synchronized cardioversion of 0.5 J/kg. If intravenous access is available, adenosine can be administered as cardioversion is being prepared (but not delayed). Special Cardiac Arrest Situations Pulseless Electrical Activity • PEA: organized ECG activity, excluding ventricular tachycardia and fibrillation, without clinical evidence of a palpable pulse or myocardial contractions. • Primary (cardiac) due to depletion of myocardial energy. Drugs used to treat primary PEA are epinephrine, atropine, calcium, and sodium bicarbonate. Special Cardiac Arrest Situations Pulseless Electrical Activity 4 H’s 4 T’s Hypoxemia Hypovolemia Hypothermia Tension pneumothorax Tamponade (cardiac) Thromboebolism Hypoelectrolemia Toxins (anesthetic overdose) When the cause of PEA is unknown and the child does not respond to medications, one should consider giving a fluid bolus and inserting needles into the pleural space to rule out pneumothorax and into the pericardial space to rule out cardiac tamponade Anaphylaxis • Flushing, pallor, or urticaria, airway edema obstruction, bronchospasm, and cardiovascular collapse. • Severe anaphylaxis in situations of decreased endogenous catecholamines as in children taking β blockers or receiving spinal or epidural anesthesia. • Resuscitation rests on reversing airway obstruction and restoring intravascular volume and vascular tone. • In the child with impending cardiac arrest, 0.01 mL/kg of subcutaneous epinephrine (1 : 1000 concentration). • Large volume fluid resuscitation of BSS. • Diphenhydramine (Benadryl), 1 mg/kg. • Methylprednisolone (Solu-Medrol), 2 mg/kg. • Albuterol may help reverse bronchospasm. • The airway should be secured early before being difficult to secure. THANK YOU • Continue resuscitation until: • The child shows signs of life (normal breathing, cough, movement or definite pulse of greater than 60 min-1). • Further qualified help arrives. • You become exhausted. Chest compression in children aged over 1 year: „hƒn Place the heel of one hand over the lower half of the sternum (as above). „hƒn Lift the fingers to ensure that pressure is not applied over the child’s ribs. „hƒn Position yourself vertically above the victim’s chest and, with your arm straight, compress the sternum to depress it by at least one-third of the depth of the chest. „hƒn In larger children, or for small rescuers, this may be achieved most easily by using both hands with the fingers interlocked. • Chest compression in infants: • The lone rescuer should compress the sternum with the tips of two fingers. • If there are two or more rescuers, use the encircling technique: • o Place both thumbs flat, side by side, on the lower half of the • sternum (as above), with the tips pointing towards the infant’s • head. • o Spread the rest of both hands, with the fingers together, to • encircle the lower part of the infant’s rib cage with the tips of the • fingers supporting the infant’s back. • o Press down on the lower sternum with your two thumbs to • depress it at least one-third of the depth of the infant’s chest. For all children, compress the lower half of the sternum: To avoid compressing the upper abdomen, locate the xiphisternum by finding the angle where the lowest ribs join in the middle. Compress the sternum one finger’s breadth above this. Compression should be sufficient to depress the sternum by at least onethird of the depth of the chest. Don’t be afraid to push too hard. Push “hard and fast”. Release the pressure completely, then repeat at a rate of 100 - 120 min-1 After 15 compressions, tilt the head, lift the chin, and give two effective breaths. Continue compressions and breaths in a ratio of 15:2. • If you are confident that you can detect signs of a circulation within 10 s: • Continue rescue breathing, if necessary, until the child starts breathing effectively on his own. • Turn the child onto his side (into the recovery position) if he starts breathing effectively but remains unconscious. • If there are no signs of life, unless you are CERTAIN that you can feel • a definite pulse of greater than 60 min-1 within 10 s • Start chest compression. • Combine rescue breathing and chest compression. • • • • • • • • • • • • Assess the child’s circulation (signs of life): Take no more than 10 s to: Look for signs of life. These include any movement, coughing, or normal breathing (not abnormal gasps or infrequent, irregular breaths). If you check the pulse take no more than 10 s: o In a child aged over 1 year – feel for the carotid pulse in the neck. o In an infant – feel for the brachial pulse on the inner aspect of the upper arm. o For both infants and children the femoral pulse in the groin (mid way between the anterior superior iliac spine and the symphysis pubis) can also be used. For both infants and children, if you have difficulty achieving an effective breath, the airway may be obstructed: • Open the child’s mouth and remove any visible obstruction. Do not perform a blind finger sweep. • Ensure that there is adequate head tilt and chin lift but also that the neck is not over extended. • If head tilt and chin lift has not opened the airway, try the jaw thrust method. • Make up to 5 attempts to achieve effective breaths. If still unsuccessful, move on to chest compression. Rescue breaths for an infant: • Ensure a neutral position of the head (as an infant’s head is usually flexed • when supine, this may require some extension) and apply chin lift. • Take a breath and cover the mouth and nasal apertures of the infant with • your mouth, making sure you have a good seal. If the nose and mouth • cannot both be covered in the older infant, the rescuer may attempt to seal • only the infant’s nose or mouth with his mouth (if the nose is used, close the • lips to prevent air escape). • Blow steadily into the infant’s mouth and nose over 1-1.5 s sufficient to make • the chest rise visibly. • Maintain head position and chin lift, take your mouth away, and watch for his • chest to fall as air comes out. • Take another breath and repeat this sequence four more times. Rescue breaths for a child over 1 year: Ensure head tilt and chin lift. Pinch the soft part of his nose closed with the index finger and thumb of your hand on his forehead. Open his mouth a little, but maintain the chin lift. Take a breath and place your lips around his mouth, making sure that you have a good seal. Blow steadily into his mouth over about 1-1.5 s sufficient to make the chest rise visibly. Maintaining head tilt and chin lift, take your mouth away and watch for his chest to fall as air comes out. Take another breath and repeat this sequence four more times. Identify effectiveness by seeing that the child’s chest has risen and fallen in a similar fashion to the movement produced by a normal breath. • 5A. If the child is breathing normally: • Turn the child onto his side into the recovery position (see below). • Send or go for help – call the relevant emergency number. Only leave the child if no other way of obtaining help is possible. • Check for continued normal breathing. • • • • 5B. If the breathing is not normal or absent: Carefully remove any obvious airway obstruction. Give 5 initial rescue breaths. While performing the rescue breaths note any gag or cough response to your action. These responses, or their absence, will form part of your assessment of ‘signs of life’, described below. • In the first few minutes after cardiac arrest a child may be taking infrequent, noisy gasps. Do not confuse this with normal breathing. Look, listen, and feel for no more than 10 s before deciding – if you have any doubts whether breathing is normal, act as if it is not normal. • 4. Keeping the airway open, look, listen, and feel for normal breathing by • putting your face close to the child’s face and looking along the chest: • Look for chest movements. • Listen at the child’s nose and mouth for breath sounds. • Feel for air movement on your cheek. • 3B. If the child does not respond: • Shout for help. • Turn the child onto his back and open the airway using head tilt and chin lift: • o Place your hand on his forehead and gently tilt his head back. • o With your fingertip(s) under the point of the child’s chin, lift the • chin. Do not push on the soft tissues under the chin as this may • block the airway. • o If you still have difficulty in opening the airway, try the jaw thrust • method: place the first two fingers of each hand behind each side • of the child’s mandible (jaw bone) and push the jaw forward. • 1. Ensure the safety of rescuer and child. • 2. Check the child’s responsiveness: • Gently stimulate the child and ask loudly, ‘Are you all right?’ • Do not shake infants, or children with suspected cervical spine injuries. • 3A. If the child responds by answering or moving: • Leave the child in the position in which you find him (provided he is not in further danger). • Check his condition and get help if needed. • Reassess him regularly. Rescuers Taught the Adult BLS Rescuers who have been taught adult BLS, and have no specific knowledge of pediatric resuscitation, should use the adult sequence with the following modifications : -Give 5 initial rescue breaths before starting chest compression. -If you are on your own, perform CPR for 1 min before going for help. -Compress the chest by at least one-third of its depth. - Use two fingers for an infant under 1 year; use one or two hands for a child over 1 year as needed to achieve an adequate depth of compression.