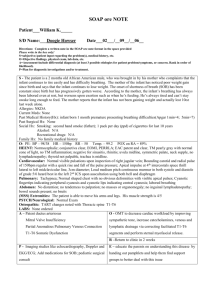
Infant/Child Basic Life Support
advertisement

Infant/Child Basic Life Support Infant/Child Basic Life Support Aim • This resource aims to introduce you to Basic Life Support (BLS) and the appropriate use of the Recovery Position for infants and children in and out of hospital. The timetabled practical workshop will enable supervised practice of all techniques. • All techniques are taught in accordance with the Resuscitation Council UK (RCUK) “Standards for clinical practice and training”(2004) and the latest (October 2011) Resuscitation guidelines which are available to download from www.resus.org.uk Infant/Child Basic Life Support Learning Outcomes At the end of this learning experience you should be able to: 1.Describe the ABC of Basic Life Support (BLS). 2.Describe the underlying anatomy and physiology of BLS. 3.Demonstrate effective BLS for all age groups. 4.Identify the differences in technique required when applying the principles of BLS to different age groups. 5.Demonstrate the Recovery Position. 6.Demonstrate how to relieve a foreign body obstruction in all age groups. 7. Demonstrate effective use of a pocket mask. Infant/Child Basic Life Support Basic Life Support is the series of measures intended to maintain adequate ventilation and circulation until expert help arrives. It may be required in the following situations; • An unconscious non breathing casualty (respiratory arrest). • An unconscious casualty who is not breathing and has no heart beat (cardio-respiratory arrest). • A casualty who is breathing and has a heartbeat but is unconscious and will need to be put into the recovery position wherever possible. Infant/Child Basic Life Support in terms of BLS • Infants are less than I year in age • Children are aged 1-8 In practice the size of the child is more important than the age Infant/Child Basic Life Support In order to live we need a regular supply of glucose and oxygen to all parts of the body. The brain in particular becomes severely damaged if deprived of oxygen for more than a few minutes (usually 3 to 4). Infant/Child Basic Life Support To ensure that the brain and other organs are supplied with oxygen three things are essential: Airway Clear and open to enable air containing oxygen to pass into lungs. Infant/Child Basic Life Support Breathing This process delivers air into lungs so oxygen can enter the blood. Infant/Child Basic Life Support Circulation Requires a pumping heart and sufficient blood to carry oxygen around the body. Infant/Child Basic Life Support Basic Life Support (BLS), is the emergency treatment needed to overcome failure of one or all of these functions. Cardio respiratory arrest or cardiac arrest - when breathing has stopped and the heart is not maintaining an adequate cardiac output -is most likely to occur in infants and children as a result of respiratory failure and hypoxia. The Resuscitation Guidelines are based on this premise. Basic Life Support buys the casualty time preventing organ damage resulting from a lack of oxygen but is unlikely to cause the heart to re-start therefore summoning expert help is vital Infant/Child Basic Life Support Before approaching a casualty always check for: Danger • To yourself • The Casualty • Bystanders Infant/Child Basic Life Support Check RESPONSE • Tap or flick the sole of the foot • Call the child’s name NEVER SHAKE A BABY Infant/Child Basic Life Support and then……. Call for expert help Infant/Child Basic Life Support Anatomy of the airway of infants and children • The cartilaginous rings surrounding the airway are softer than in adults making it more susceptible to occlusion if the head is incorrectly positioned. • In infants the occiput is very large tending to push the head forward and occluding the airway. • Infants and children have larger tongues relative to their size increasing the chance of airway obstruction. • The airway is narrower meaning that any inflammation of the airway could cause severe distress. • The airway is “funnel shaped” becoming narrower at the level of the larynx any foreign body can become lodged here. Infant/Child Basic Life Support Open the Airway By using the head tilt chin lift manoeuvre. The head is maintained in a neutral position. Breathing Check for •Look at the chest for movement. •Listen for breath sounds •Feel for air on your cheek Infant/Child Basic Life Support This check should take 10 seconds if the child is breathing normally and it is safe to do so, place him in the recovery position( and summon help from the ambulance service by calling 999 OR 112 (the later number is valid throughout Europe) . Stay with the child and reassess regularly. Infant/Child Basic Life Support ALTERNATIVE METHOD OF OPENING AIRWAY WHEN THERE IS SUSPECTED NECK (CERVICAL) INJURY JAW THRUST Infant/Child Basic Life Support • Remember the most likely cause of cardiac arrest in infants in children is hypoxia so in a non-breathing child give five rescue breaths first. Infant/Child Basic Life Support • In the older child place the mouth over the child’s mouth creating a seal an pinch the nose. • For both age groups deliver each breath slowly over 1-1.5 seconds taking a breath yourself between each one • Check for chest movement Infant/Child Basic Life Support • Having given 5 effective rescue breaths check for Circulation • Look for signs of life such as coughing movement or normal breathing. • It is also recommended to check for the presence of an effective central pulse. • In babies either the brachial or femoral pulse can be used. • In children the carotid pulse can be used. Infant/Child Basic Life Support Brachial site Femoral site Infant/Child Basic Life Support Carotid site Infant/Child Basic Life Support Ensure an ambulance has been called. • Place two fingers on the lower third of the sternum one fingers breadth below the nipple line. • Commence 15 chest compressions at a speed of 100 -120 per min Infant/Child Basic Life Support Ensure an ambulance has been called. • Place the heel of one hand on the lower third of the sternum. • Commence 15 chest compressions at a speed of 100 -120 per min. Infant/Child Basic Life Support Alternative approach for compressions in infants When there are two rescuers present ; • Place both thumbs on the lower third of the sternum one fingers breadth below the nipple line. • The hands should encircle the infants chest and support his back. • Commence 15 chest compressions at a speed of 100 -120 per min. Infant/Child Basic Life Support • Defibrillation Defibrillation is a rare event in paediatric cardiac arrests In an out of hospital situation a defibrillator will either come with the ambulance or may be available in supermarkets trains stations etc. In hospital this will be part of the cardiac arrest or “crash” trolley. Defibrillators should only be used by those trained in their use The outcome of paediatric cardiac arrest is poor (Kitamuara et al 2010) The child’s best chance of survival is recognition of the signs of deterioration in the sick child. The Airway Breathing Circulation Disability Exposure mnemonic gives priority to the key management steps in the assessment and treatment of sick children. It should be used in all children and SAVES LIVES Infant/Child Basic Life Support • If following the assessment the child is discovered to be breathing normally but not fully conscious he should be placed in the recovery position. • The rationale for this is to maintain a safe airway by maintaining the head tilt chin lift and prevent inhalation of any blood or vomit which may threaten the patency of the airway. • Whilst the recovery position is the safest position for an unconscious casualty NEVER try to move someone if you think they might have other injuries which may be made worse by moving. In this situation maintain the airway and wait for expert help to arrive. • See how to place a child in the recovery position here http://www.youtube.com/watch?v=mMnzn8T_3Q8 Infant/Child Basic Life Support • The sequence of actions you should take in hospital are the same and should be commenced as soon as possible; • The ONLY differences are; • You should call the emergency response team (Crash Team) on the specially designated number stating that it is a paediatric arrest. A safety alert issued by National Patient Safety Agency (NPSA 2004) required NHS hospitals to standardise this number to 2222, but always check. • When performing rescue breathing always use a pocket mask, or, if you know how to use it, a bag valve mask (RC/UK 2003). 29 Infant/Child Basic Life Support Pocket Mask Infant/Child Basic Life Support Bag Valve Mask Infant/Child Basic Life Support • If a solid or liquid object enters the airway the child will immediately react with vigorous coughing. • If the object completely obstructs the airway (Foreign Body Airway Obstruction FBAO) normal movement of air is prevented and asphyxia and hypoxia will rapidly develop. • Airway obstruction can also be caused by infection and inflammation resulting in oedema or an allergic response. In this instance emergency medical care must be sought. • The two causes of airway obstruction are managed differently. Infant/Child Basic Life Support Recognition of FBAO • The event may be witnessed • If not witnessed clues could be a history of eating or playing with small items or toys immediately before the episode. • The airway obstruction develops suddenly without any other signs of illness or infection. Infant/Child Basic Life Support Infant/Child Basic Life Support Back Blows Infant Child Infant/Child Basic Life Support Chest Thrust Infant Infant/Child Basic Life Support Abdominal Thrust Child Infant/Child Basic Life Support If the child becomes unconscious: • • • • Place on a firm flat surface Send for help if still not available Open the mouth and look for any obvious object If seen make one attempt to remove with a single finger sweep DO NOT ATTEMPT MULTIPLE OR BLIND FINGER SWEEPS • Open the airway attempt five rescue breaths • Commence CPR at a ratio of 15:2 • Re-check the airway with each set of rescue breaths and remove if seen as above. Infant/Child Basic Life Support • Now attempt the Multiple choice questions. References and Resources •Resuscitation Guidelines 2010 Resuscitation Council (UK). •Safer Handling during Resuscitation Resuscitation Council (UK) 2009. • Standards for clinical practice and training (2008) A Joint Statement from The Royal College of Anaesthetists, The Royal College of Physicians of London, The Intensive Care Society, The Resuscitation Council (UK) •Teaching- Bag -Valve Mask RC(UK) Statement June 2003. All the above available from Resuscitation Council UK Website: www.resus.org.uk • Kitamura T. Iwami T. Kawamura T. et al “Conventional and chest compression only cardiopulmonary resuscitation by bystanders for children who have outof-hospital cardiac arrests: a prospective, nationwide ,population based cohort study” Lancet 2010; 375: 1347-54