acute spinal cord lession
advertisement

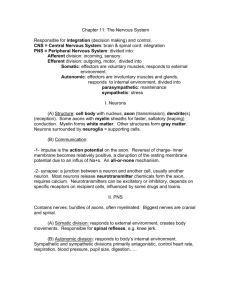
ACUTE SPINAL CORD LESSION MEITI FRIDA DEPARTMENT OF NEUROLOGY FACULTY OF MEDICINE ANDALAS UNIVERSITY ANATOMY OF SPINE AND SPINAL CORD The spine has three major components: the spinal column (bones and discs) neural elements (the spinal cord and nerve roots) supporting structures (muscles and ligaments) The spinal column consists of: seven cervical vertebrae (C1–C7) i.e. neck twelve thoracic vertebrae (T1–T12) i.e. upper back five lumbar vertebrae (L1–L5) i.e. lower back five bones (that are joined, or "fused," together in adults) to form the bony sacrum three to five bones fused together to form the coccyx or tailbone Adult spinal cord: Inside vertebral canal 31 segments, each associated with a pair of dorsal root ganglia Extends to L1/ L2 (Conus medularis) Cauda equina - origin of spinal nerves extending inferiorly from conus medullaris Spinal Meningen Three membranes surround all of CNS 3) Pia mater 1) Dura mater - "tough 2) Arachnoid mother", strong 2) Arachnoid - spidery looking, carries blood vessels, etc. Subarachnoid space 3) Pia mater - adheres tightly to surface of spinal cord 1) Dura mater Organization of Cord Cross Section Gray matter posterior - somatic and visceral sensory nuclei anterior (and lateral) gray horns – somatic and visceral motor control gray commissures - axons carrying information from side to side White matter posterior white column anterior white column lateral white column anterior white commissure Functions ascending tracts - sensory toward brain descending tracts - motor from brain White Matter: Pathway Generalizations Vascular anatomy - Anterior spinal artery Anterior spinal artery originates in upper cervical region, from anterior spinal branches of vertebral artery. 6-10 anterior radicular arteries contribute to it throughout its length. Supplies anterior two thirds of cord, via central branches and penetrating branches of pial plexus Vascular anatomy – posterior spinal artery Run along posterolateral cord Sometimes discontinuous Originates from verterbral artery Has contribution from 10-23 posterior radicular a. Supplies posterior one third of cord Vascular anatomy - arteries and venous Acute lession of spinal cord Traumatic spinal cord injury Vascular Myelopathies Infectious Myelopathies Inflammatory Myelopathies Traumatic spinal cord injury Mechanism of injury Flextion and flextion-rotation injury Compression injury Hyperextention injury Level of injury Quadriplegia : injury in cervical region all 4 extremities affected Paraplegia : injury in thoracic, lumbar or sacral segments 2 extremities affected Complete and Incomplete Spinal Cord Syndromes can be classified into either complete or incomplete categories Complete – characterized as complete loss of motor and sensory function below the level of the traumatic lesion Incomplete – characterized by variable neurological findings with partial loss of sensory and/or motor function below the lesion Spinal Shock An immediate loss of reflex function, called areflexia, below the level of injury Signs: ◦ ◦ ◦ ◦ ◦ Slow heart rate Low blood pressure Flaccid paralysis of skeletal muscles Loss of somatic sensations Urinary bladder dysfunction Spinal shock may begin within an hour after injury and last from several minutes to several months, after which reflex activity gradually returns Brown-Sequard Syndrome (Special Form of Spinal Cord Injury) Results from an injury to only half of the spinal cord and is most noticed in the cervical and thoracal region Often caused by spinal cord penetrating trauma Motor loss is evident on the same side as the injury to the spinal cord Sensory loss is evident on the opposite side of the injury location (pain and temperature loss) Bowel and bladder functions are usually normal Person is normally able to walk although some bracing or stability devices may be required ASIA Impairment Scale of spinal cord injury ASIA – American Spinal Injury Association : A – Complete: no sensory or motor function preserved in sacral segments S4 – S5 B – Incomplete: sensory, but no motor function in sacral segments C – Incomplete: motor function preserved below level and power graded < 3 D – Incomplete: motor function preserved below level and power graded 3 or more E – Normal: sensory and motor function normal ATLS principles A irway; protect spine B reathing C irculation D isability E xpose patient Treat Secondary survey Pharmacologic Therapy Option: Methylprednisolone NASCIS II (1992) ◦ 30mg/kg IV loading dose + 5.4 mg/kg/hr (over 23hrs) effective if administered within 8 hours of injury NASCIS III (1997) ◦ If initiated < 3hrs continue for 24 hrs, if 3-8 hrs after injury, continue for 48hrs (morbidity higher increased sepsis and pneumonia) Vascular Myelopathies Spinal Cord Ischemia Spinal Hemorrhage Spinal Cord ischemia In most cases Sensory features ( pain ) emerge first , followed by weakness within minutes or hours Pain often follows radicular pattern ( common presentation ) Maximum weakness is observed within 12 hrs of onset Lower thoracic and lumbar spinal levels are most commonly affected Urinary retention : in acute phase Involuntary voiding or defecation : associated with onset of ischemic insult STROKE SYNDROME FEATURE ANTERIOR SPINAL ARTERY INFARCT Bilateral motor deficit with Spinothalamic sensory deficit ANTERIOR UNILATERAL INFARCT Hemiparesis with Contralateral spinothalamic sensory deficit POSTERIOR UNILATERAL INFARCT Hemiparesis with Homolateral lemniscal sensory deficit CENTRAL INFARCT Bilateral Spinothalamic sensory deficit without motor deficit POSTERIOR SPINAL ARTERY INFARCT Bilateral motor deficit with lemniscal sensory deficit TRAVERSE INFARCT Bilateral motor deficit with complete sensory deficit Spinal Cord Hemorrhage Spinal cord dysfunction – due to hemorrhage into Sub arachnoid space Sub dural space Epidural space Onset : Sudden & Painful Triggers : Trauma Bleeding diatheses Vascular malformations Investigations : CSF Analysis : usually normal can be xanthochromic raised protein MRI Contrast enhanced CT scan with sagittal / coronal reformatting is useful in pts who cannot undergo MRI MR Angiography Selective Spinal Angiography using Digital Substraction Techniques Treatment : SCH is surgical emergencies Immediate surgery Laminectomy and clot evacuation Angiographically directed embolization of vascular malformation Infectious Myelopathies Virus Enteroviruses (poliovirus, coxsackie virus, and enterovirus 71), Flaviviruses (West Nile virus and Japanese encephalitis virus) have been known to target the gray matter (Anterior horn cells) producing acute lower motor neuron disease CMV,VZV, HSV I &II, HCV, and EB HIV Bacterial Mycoplasma (acute and post infectious), Listeria monocytogenes TB Lyme disease Schistosomiasis (in endemic areas) Clinical features of infectious process Fever Meningismus Encephalopathy Rash Lymphadenopathy Known systemic infection Immunocompromised status Known exposure to infectious agent Inflammatory Myelopathies Acute Disseminated Encephalomyelitis Transverse Myelitis Acute Disseminated Encephalomyelitis Characterized by acute to subacute onset of fever, meningismus, encephalopathy and multifocal symptoms & signs of CNS dysfunction More common in children Recent vaccination or systemic infection is noted in ½ of cases Brain MRI reveals numerous medium to large size , fairly symmetrical subcortical white matter lesions often with involvement of deep gray matter Transverse Myelitis (TM) Immune-mediated process results in neural injury to the spinal cord Varying degrees of weakness, sensory alterations and autonomic dysfunction Up to half of idiopathic cases will have a preceding respiratory or gastrointestinal illness TM Diagnostic Criteria Treatment of Myelitis Acute myelitis attacks are typically treated with IV Corticosteroids Methyl prednisolone Resistant cases : Plasmapheresis Very severe attacks : combination of Corticosteroids, Plasmapheresis, Cyclophosphamide No evidence supports use of IV Ig in inflammatory myelitis Neoplastic & Paraneoplastic Myelopathies Most primary tumors of cord do not cause acute myelitis syndromes Lymphoma is the only exception – causes a subacute myelopathy - corticosteroid responsive Breast carcinoma : antiamphiphysin antibodies and severe spastic myelopathy Ovarian and Non small cell lung cancer : glutamic acid decarboxylase 65 autoantibodies causing stiff man like syndrome with brain stem features and ataxia