Controlling Asthma: Preventing episodes before they occur
advertisement

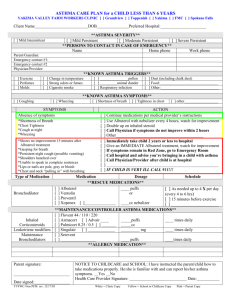
Controlling Asthma: Preventing Episodes Before They Occur Is There A Cure For Asthma? Asthma cannot be cured, but it can be Controlled “We should expect nothing less”! Goals Of Asthma Control Prevent Symptoms • No coughing or wheezing • No shortness of breath or rapid breathing • No waking up at night Maintain normal or near “normal” pulmonary function Maintain normal activity levels (including exercise and other physical activities Prevent exacerbations of asthma and minimize ER/UC and hospital visits Minimal or no adverse effects from medications Meet patients/family’s expectations and satisfaction with asthma care Exerts from NAEPP EPR2 Guidelines for Diagnosis and Management of Asthma 1997 Asthma Control Do Most Students Have It? Unfortunately NO! Many students who have asthma: • Have poor asthma control • Use “quick relief” medicine (e.g. albuterol) on a regular basis • Cough, experience chest tightness, wheezing, or shortness of breath regularly • Assume suffering from symptoms are “normal” • Remain indoors and cannot fully participate in sports, PE or recess • Miss school due to asthma Examples Of Students Whose Asthma Is NOT Optimally Controlled • A 10th grader, says he feels fine except when he runs in PE class, then his chest hurts. He coughs most mornings and whenever he gets a cold or virus. He often can’t keep up with the other kids and needs to stop and rest. • A 12th grader, carries an OTC Primatine Mist inhaler & uses it a few times every day. He says he “grew out” of his asthma. Examples Of Students Whose Asthma IS Optimally Controlled • A 6th grader, doesn’t need his “reliever”(albuterol) since consistently using his controller medications twice daily. He now plays soccer without developing symptoms or having to take preexercise albuterol. • A kindergartener, no longer coughs or wheezes and easily keeps up with the other kids at recess. Her dad bought special dust mite proof covers for her mattresses and pillow. She now takes her controllers daily, uses her Asthma Action Plan, and sees her health care provider every 6 months for a well asthma check-up. Asthma Severity Level vs Asthma Control Asthma Severity Levels (Mild Intermittent, Mild Persistent, Moderate Persistent, and Severe Persistent) Based on signs and symptoms before a student starts on controller medications Levels can change over time Asthma Control (or “Current Asthma Severity”) Is the students current severity levelregardless if they are on medications, experiencing symptoms (episodes) and/or able to be fully active Asthma Control Proactive vs Reactive • Going from a reactive to a proactive approach Instead of thinking“ How do I treat these symptoms?” e.g. with albuterol after the fact Think“ How could have the symptoms have been prevented in the first place?” e.g. daily controller medications, pre-exercise meds, asthma action plan, environmental control Controlling Asthma Medical & Environmental Management Controlling Asthma Medical Management How To Achieve Good Asthma Control Have regular asthma check-ups with a primary healthcare provider, even when feeling well • At least every 6 months (more often if having symptoms) Monitor symptoms and peak flow readings daily Ask for and use a personalized Asthma Action Plan Know personal green- yellow- red zones, what each zone feels like and what to do in each zone Asthma Control Continued... Get a flu shot every fall Avoid asthma triggers Asthma’s not in control? Check in regularly at school health office for: • Peak flow check /symptom evaluation • Lung sounds / respiratory rate check • Pre-exercise and/or controller meds • Asthma education • Care coordination Asthma Action Plan See MDH Asthma Action Plan F1 Written Asthma Action Plans Developed by the health care provider for each individual child with asthma Medications are determined by asthma severity level Based on symptoms and peak flow rates Lists daily & rescue medications Symptom management and emergency plan Copies to be shared by clinic, family and school Asthma Action Plan Zones Green Zone: All Clear/Breathing Good/Go – No asthma symptoms and/or – Peak flow 80-100% Predicted or Personal best Yellow Zone: Caution/Slow Down – Some asthma symptoms and/or – Peak flow 50-80% Predicted or Personal best Red Zone: Medical Alert/Stop – Severe asthma symptoms and/or – Peak flow < 50% Predicted or Personal best What Can A Student Do To Stay In The Green Zone? Select The Incorrect Answer A. Take their controller (anti-inflammatory) medication every day B. Avoid cigarette smoke and other asthma triggers C. Take their pre-exercise (usually reliever) medicine before P.E. or at recess D. Wash their bathroom often with bleach to avoid mold and mildew build-up What Can A Student Do To Stay In The Green one? Select The Incorrect Answer A.Take their controller (anti-inflammatory) medication every day B. Avoid cigarette smoke and other asthma triggers C. Take their pre-exercise (usually reliever) medicine before P.E. or at recess D. Wash their bathroom often with bleach to avoid mold and mildew build-up If A Student Is In The Yellow Zone, They Should: A.Be cautious. Breathing isn’t their best. Take action B.Eat a lot of yellow foods such as bananas, which are high in potassium C.Automatically stay home from school D.Call their doctor or nurse practitioner immediately If A Student Is In The Yellow Zone, They Should: A. Be cautious. Breathing isn’t their best. Take action B. Eat a lot of yellow foods such as bananas, which are high in potassium C. Automatically stay home from school D. Call their doctor or nurse practitioner immediately (correct answer: call if they aren’t fully back into the green zone within 48-72 hours). R1 Which Is One Symptom/ Clinical Indicator Is NOT Associated With The Red Zone? A. Mild coughing B. Peak Flow reading < 50% of personal best C. Significant breathing problems D. Persistent wheezing or no wheezing at all indicating severely limited aeration Which Is One Symptom/ Clinical Indicator Is Not Associated With the Red Zone? A. Mild coughing B. Peak Flow reading < 50% of personal best C. Significant breathing problems D. Persistent wheezing or no wheezing at all indicating severely limited aeration Activity Group Case Discussion The first month of school, you are called to an elementary school by a substitute teacher. She sent a 3rd grader to the nurse’s office alone, and told her to lay down. When you arrive, child has neck vein distension, accessory muscle retractions, dark/dusky color. No inhaler available Mom is 45 min. away. Grandma is in town WHAT DO YOU DO? Answer: Provide emergency care and medication per AAP/ Management plan and CALL 911! Controlling Asthma Environmental Management Common Environmental Triggers At Schools • Indoor Triggers • Outdoor Triggers Animals with fur Ozone Dust mites Particulate matter Mold Diesel exhaust Pests Chemicals (e.g. re-surfacing the playground or roof, etc.) Secondhand smoke Chemicals (e.g. strong smelling cleaning supplies, perfume, air fresheners) Animals • Dander, urine & saliva are triggers • Triggers remain months after animal pet removed • Actions: Prohibit/remove animals from schools if able If removal is not possible: » Keep animals in cages or localized areas » Clean cages often » Keep animals away from fabric furniture, carpet & ventilation system » Locate sensitive students away from animals Pre-notify parents if animals with fur/feathers visit • Sample Animals in School Guidelines in manual R1 Dust Mites • Both cause & trigger asthma; live in pillows, carpet, fabriccovered furniture, curtains • Actions: Keep classrooms clutter-free Make informed decision: presence of carpet Vacuum often when people with asthma/allergies are gone (HEPA filter vacuum cleaners may help) Pillows/mattress/box spring in dust-mite proof zipped covers Wash bedding and stuffed toys weekly in HOT water (>130 degrees F) Keep room humidity < 50% if possible Mold • Moisture control is key • Actions: Report leaks and wet/moist areas right away Wash mold off hard surfaces Replace moldy porous items such as ceiling tiles & carpet Avoid carpet in areas with regular moisture such as drinking fountains & sinks E9 Pests • Droppings or body parts can trigger asthma • Actions: Use integrated pest management (IPM) methods » » » » Don’t leave food, water or garbage exposed Don’t eat or drink in classroom Seal entry points for pests Use pesticides only as needed Parent Right to Know Act: must notify parents & employees when using specific pesticides F32, F33, F34 Secondhand Smoke • Causes asthma in young children & triggers asthma in children & adults • Contains over 4,000 substances • State law prohibits tobacco use in K-12 public schools • Actions: Enforce smoking bans (for anyone on school property) Include anti-smoking message in curriculum Encourage parents/guardians to quit smoking or to not smoke inside their home Outdoor Air • Ozone & fine particles are concerns in MN • Staff have little control over outdoor air • Actions: Sign up for Air Quality Index notice » Pollution Control Agency sends e-mail alerts when they expect poor air quality (regional) Avoid being outside at high pollen count times, especially if students are allergic to particular pollen/s Sept. 14, 2000/June 28, 2001 The AQI Average Number Of Alerts 6-12 alerts per year in last few years Most due to PM2.5 Not violation of federal air quality standards thus far Health issues still valid 2003 – Air Pollution Health Alerts Expanded AQI to Duluth, St. Cloud, Rochester Detroit Lakes, Marshall coming soon Expanded media coverage (Pioneer Press, TV meteorologists, health reporters, others) Expanded web & e-mail alert signup MPCA’s AQI web page 1 MPCA’s AQI web page 2 School Buses • State law requires: Reduce unneeded idling in front of schools Reroute bus parking zones away from air intakes, if possible • Actions: Post “no idling” signs Maintain bus fleet Invest in cleaner fuels Purchase newer, cleaner buses over longterm R2, R3, R4 Other Environmental Issues • • • • Indoor Air Quality Management Plan Cleaning & cleaning products Flooring Air cleaners R7 Home Environment Resources • US Environmental Protection Agency Asthma Home Environment Checklist » 8 page checklist of common asthma triggers » Questions to identify triggers & action steps Clear Your Home of Asthma Triggers fact sheet • EPA website www.epa.gov/iaq/asthma/resources.html Communication & Care Coordination Key Communication Triad Parent/ Guardian Child School Health Office Health Care Providers Care Coordination / Communication (Health Assistant / Paraprofessional/LPN Role) Health Assistants / Paraprofessionals / LPNs must alert LSN/PHN/RNs of students who come in frequently with asthma type symptoms Monitor students with asthma as directed by LSN/PHN/RN Perform delegated responsibilities once skills have been validated per district/school policies Care Coordination /Communication (LSN/RN/PHN) • Examples of asthma care coordination activities Request AAPs on students Review AAP and/or IHP and develop/modify plan for care coordination Determine medical insurance status and connect to appropriate provider(s) Arrange for special transportation (in rare cases) prn Connect to community resources Care Coordination/ Communication • Communicating with Students • Educate them to: Follow an individualized Asthma Action Plan Avoid or control exposure to their triggers Use medication appropriately • Long-term-control medicine • Quick-relief medicine Monitor symptoms and response to treatment • Understand symptoms and peak flow levels • Seek a health care providers help when needed Communicating w/ Students Continued.. Get regular follow-up care Be able to exercise/ play at optimal levels Be responsible for carrying and using their asthma medications per school policies Ask for help when they need it! Care Coordination/ Communication • Communicating with parents/guardians Review parent/guardian and student questionnaires Determine current asthma severity levels Provide education to family/student as needed Encourage questions and give feedback Contact parent/guardian every time a student has asthma symptoms and or if having poor asthma control Obtain a signed consent to release/ share information F11, F14, F3, E1, F7 Care Coordination / Communication • Communicating with health care providers Report status changes and re-evaluation needs Advocate for pre-exercise and /or controller medications as appropriate Arrange for asthma education Complete IHP and/or ECP if needed Document as appropriate in Pupil Health Record Evaluate symptoms, lung sounds and peak flow regularly on poorly controlled students F17, F18 Communicating With School Staff Share information with staff on a need to know basis only Maintain student confidentiality Provide general asthma education to staff proactively Provide asthma first aid training to staff Act as a resource to school staff for questions and concerns Health Office Scenario • A 4th grade student who you have not seen in the health office this year for asthma symptoms, has a diagnosis of asthma in her record, and has albuterol MDI / orders in the health office at school, but no Asthma Action Plan. She comes into the health office with a persistent cough. • What would you do for her? Health Office Scenario Continued... • Actions Physical Assessment (respiratory rate, breath sounds, severity of symptoms) Ask what she was doing before coming into the health office / what may have precipitated symptoms Ask frequency of day / nighttime symptoms Check height/PF chart for predicted PF and initiate Asthma Record F5 Health Office Scenario Continued... Check her Peak Flow reading and document in SHOAR F4 » Instruct the child how to do a PF reading Give albuterol (observe inhaler technique) Teach/reinforce proper inhaler technique, use of spacer or holding chamber with inhaler Monitor her for response to medication Send note home with the child using the AVN and a PAQ F11 F8 Health Office Scenario Continued... • Two days later, she returns to the health office, with cough and shortness of breath • What would you do for this 4th grader first? • What would be the next steps or what else should you do at this point? Health Office Scenario Continued… • What else should you do now? Re-evaluate her respiratory status and treat as appropriate Call her parent / guardian to notify, ask for parent questionnaire/more info. Suggest she see her health care provider Ask the child to come see you the next day for a follow up check If you have consent, fax Asthma Medical Referral/Request to health care provider F9 Asthma Management In The School Health Office Sample Forms For Optimal School Asthma Management Key Asthma Tools • Components of Asthma Management in the Health Office E2, E3 • Asthma Action Plan w/ imbedded consents, parent letter F1, F2 • Asthma Visit Notification form F7, F8 • Asthma Medical Request/Referral F9, F10 • Pathway for Acute School Asthma Care E6, E7 • Emergency Care Plan - Asthma F18 • Individualized Health Plan - Asthma F17 Key Asthma Tools • Parent/Guardian Breathing/Asthma Questionnaire F11, F12, F13 • Student Breathing/Asthma Questionnaire F14, F15, F16 • School Health Office Asthma Record F4, F5, F6 • Self-administration Asthma Medication Authorization F19, F20 • First Aid for Asthma poster / pocket cards E4, E5 • Asthma Green/Yellow Zone Update F23, F24 • Permanent Health Office Pass F25 Components Of Asthma Management In School Health Office Two Models Provided in School Asthma Manual LSN + Health Assistant (Mpls. Public Schools model) E2 • LSN + Secretary (St. Paul Public Schools model) E3 • Purpose: Provides job specific instructions for providing quality asthma care in the school health office • Licensed School Nurse, Public Health Nurse, Registered Nurse • Licensed Practical Nurse • Health Aid/Service Assistant / Paraprofessional • Secretary / Administrative Assistant Asthma Screening Questions Include these 3 questions into your existing student health questionnaire 1. Does your child have asthma or other breathing problems? 2. Has your child ever been diagnosed by a doctor as having asthma? 3. Has your child had episode(s) of wheezing (whistling in the chest) in the last 12 months? Asthma Action Plan (AAP) • Purpose Provides a plan to guide the asthma management of individual students Includes imbedded consents: » Allow parents/guardians and providers to give permission for medications to be given at school » Allow for sharing/release of information between school, clinic, hospital, child care provider and home care • Available in English and Spanish Asthma Visit Notification Form (AVN) • Purpose Increases communication between the school health office, parents/guardians, and primary care/asthma care providers Fill out and send home whenever the student is in the health office with asthma symptoms Or when delegated by the LSN/PHN/RN F7,F8 Asthma Medical Request (AMR) • Purpose To facilitate communication and care coordination between the health care provider and the school nurse about the student’s asthma status/management Fill out and fax, mail to health care providers You must have the parents written consent to collect medical information first F9, F10 Pathway for Acute School Asthma Care • Purpose Assists school nurses in making decisions regarding the provision of acute asthma care in the school health office or other school setting Designed to be used for students experiencing mild, moderate or severe asthma symptoms E6, E7 Asthma Emergency Care Plan (ECP) • Purpose Provides special instructions to selected school staff on how to respond to an asthma emergency Used with students with severe or labile asthma Individualized for each student with asthma F18 Asthma Individualized Health Plan (IHP) • Purpose Provides a Nursing Plan of Care and promotes care coordination and communication between the school nurse and health office staff regarding students whose asthma is not in good control • Also used to document special education nursing services F17 Parent / Guardian Asthma Questionnaire (PQ) • Purpose • Used To: Gather baseline information about the child’s asthma symptoms Determine the child’s asthma severity level Determine if the child’s asthma is under control Develop an appropriate plan of care Typically used for students in 5th grade or lower Student Breathing Questionnaire (SBQ) • Purpose Used to: Determine the student’s asthma severity level Determine if the student’s asthma is under control Develop an appropriate plan of care Determine student’s familiarity of their meds, triggers, symptoms etc. • Used with students in grades 6th grade or higher F14, F15 School Health Office Asthma Record (SHOAR) • Purpose Provides a user-friendly document on which to record many aspects of a student’s asthma care • Allows health office staff to: Record Asthma Medication Record Peak Flow Readings Document Asthma Symptoms Document Education F4, F5 Self-Administration Of Asthma Medication Authorization / Agreement • Purpose To systematize practice regarding selfcarrying of asthma medications between schools Promotes strong asthma self care skills in students Agreement between student and school nurse Used in conjunction with an Asthma Action Plan or may stand alone F19, F20 First Aid For Asthma Poster / Pocket Cards • Purpose Provides basic first aid care for asthma and asthma symptoms with directions when to call 911 Place posters in locations in the school where students and staff are usually present Pocket cards may be given to physical education teachers or coaches or other staff as needed E4, E5 Prioritizing In A Busy School Health Office There’s Never Enough Time, What Can I Do? • It isn’t possible for school health office staff to get deeply involved with every student who has asthma so • Prioritization is essential! Determine which students seem to be having the most difficulty, and focus on them first How Do I Prioritize? 1. Prioritize by “current asthma control / severity level” 2. Focus first on students with the poorest asthma control regardless of severity level 3. Start working with students whose asthma is poorly controlled in the moderate to severe persistent asthma levels Which Of These Students With Asthma Would You Focus On First? 1. A boy with diagnosed moderate persistent asthma who can run, play, attend school without symptoms and rarely uses his albuterol 2. A girl with current mild persistent asthma who is unable to fully participate in PE class 3. A girl who’s original severity level was severe persistent but whose “current asthma severity level” (control) is moderate persistent. She can play outside better than originally, but still needs albuterol for symptoms 3-4 times a week at school Which Of These Students With Asthma Would You Focus On First? 3. A boy with diagnosed moderate persistent asthma who can run, play, attend school without symptoms and rarely uses his albuterol. 2. A girl with current mild persistent asthma who is unable to fully participate in PE class. 1. A girl who’s original severity level was severe persistent but whose “current asthma severity level” (control) is moderate persistent. She can play outside better than originally, but still needs albuterol for symptoms 3-4 times a week at school. Education In The School Health Office Components Of Student & Family Education Concept of asthma control Pathophysiology of asthma Environmental control and triggers Controller vs. reliever medications and refilling medications Use of Asthma Action Plan and treatment of episodes Peak flow meter use Components Of Student & Family Education Cont… Signs and symptoms of respiratory distress and when to seek help MDI with spacer / DPI technique Nebulizer use and technique (prn) Importance of relationship with provider and well-asthma check-ups Flu shot every fall Self-care, especially for students as they get older Strategies To Educate When Time Is Limited Give short asthma education messages when meeting with with students Use innovative / interactive asthma education tools (computerized asthma games, internet-based asthma control tools, videos) with students / families The Best Laid Plans.. You can increase the likelihood of asthma management success (compliance) by: 1. Reviewing Asthma Action Plan and making sure student understands how to use it 2. Ask how controller medications fit into the student’s daily routine (can they handle it?) 3. Identify obstacles or barriers to the student/family carrying out the plan as prescribed “I Can’t Manage This By Myself. Who Else Should Be Involved”? Referring To Community Resources For Education And Case Management LSN/PHN/RNs can utilize case managers, home visiting professionals, and asthma educators from health plans, hospitals, clinics, public health, to help educate and/or case manage students whose asthma is poorly controlled Connect students/family to community education, asthma camp, other community resources Coordinated School Health: Partnering For Optimal Asthma Management In Schools CDC’s Strategies For Addressing Asthma Within A Coordinated School Health Program Six Strategies 1. Establish management and support systems for asthma-friendly schools 2. Provide appropriate school health and mental health services for students with asthma 3. Provide asthma education and awareness programs for students and school staff Strategies Continued… 4. Provide a safe and healthy school environment to reduce asthma triggers 5. Provide safe, enjoyable physical education and activity opportunities for students with asthma 6. Coordinate school, family, and community efforts to better manage asthma symptoms and reduce school absences among students with asthma Asthma Goals For School Health Healthy school environment Health services in school Asthma education Supportive policies Sound communication 1997 National Asthma Education and Prevention Program (NAEPP) Spearheading School-wide Asthma Best Practices At Your School See Checklist in manual for suggestions Create a multi-disciplinary plan for improving asthma management in your health office, school and/or district Improve own practice Educate other school staff Involve all disciplines within the school setting Community Involvement Get involved with the Minnesota Asthma Coalition, and/or the regional Asthma Coalition in your area Contact your legislators and insist on legislation to support asthma-friendly policies Anti-smoking laws Healthy housing initiatives Supporting Clean Indoor act Support stricter pollution control measures Conclusion Asthma is a big challenge for Minnesota Working together with parents and health care providers, we have the ability to positively and dramatically impact the health of children who have asthma!